2025 Vol. 7, No. 2
The widespread adoption of integrase strand transfer inhibitors (INSTIs) has led to the emergence of INSTI-associated drug-resistance mutations. This cross-sectional study conducted a comprehensive national survey to investigate the prevalence of pretreatment drug resistance (PDR) to INSTIs among newly diagnosed human immunodeficiency virus (HIV) individuals in China.
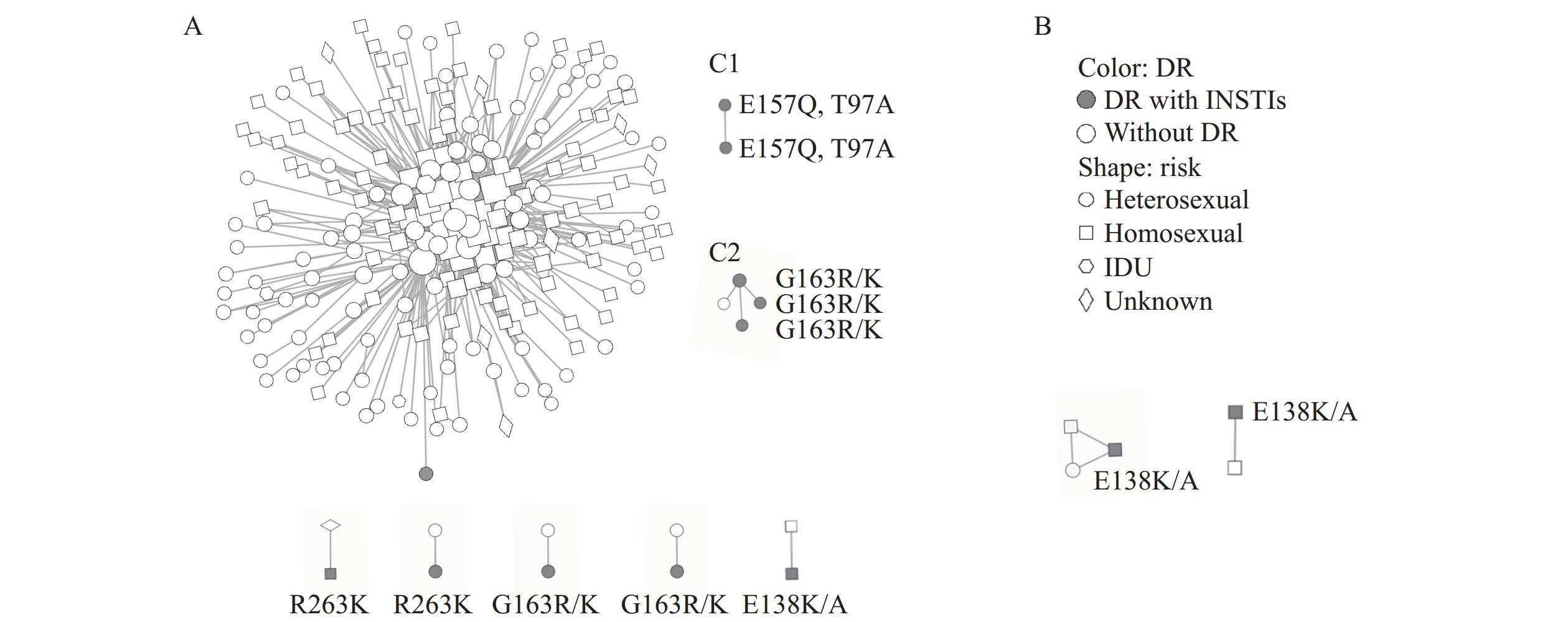
The study enrolled 10,654 individuals from 31 provincial-level administrative divisions between 2018 and 2023. All participants underwent integrase region genotypic resistance testing. PDR to INSTIs was analyzed using the Stanford HIV drug resistance database, and molecular transmission networks were constructed using HIV-TRACE.
The overall PDR prevalence of INSTIs was 0.95%. The predominant major and accessory mutations identified were E138K/A (n=19) and G163R/K (n=29), respectively. Multivariable logistic regression analysis revealed that age ≥50 years [adjusted odds ratio (aOR)=1.87, 95% confidence interval (CI): 1.03, 3.42] and HIV subtype B (aOR=3.87, 95% CI: 1.97, 7.58) were significant risk factors for PDR. Molecular network analysis showed that 1,257 (26.0%) CRF07_BC sequences formed 432 transmission clusters, while 811 (27.6%) CRF01_AE sequences were associated with 335 clusters. The identified drug-resistance mutations included E138K/A, R263K, Y143H, G163R/K, E157Q, and T97A.
The current prevalence of PDR to INSTIs in China remains low. However, given the increasingly widespread use of INSTIs, continuous surveillance of drug resistance emergence and transmission patterns is essential.
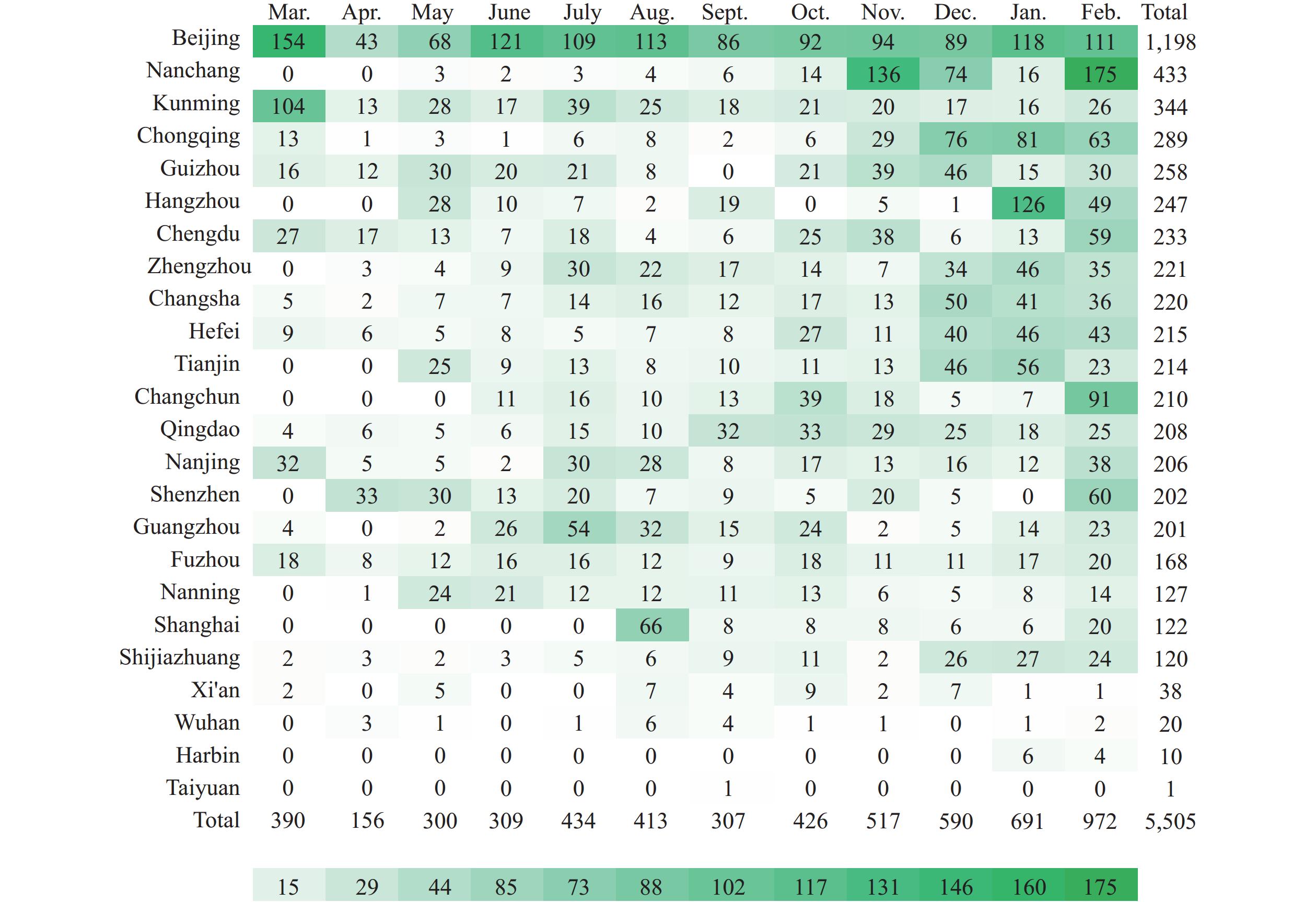
Men who have sex with men (MSM) are highly vulnerable to human immunodeficiency virus (HIV) infection and demonstrate significant mobility patterns. Understanding post-diagnosis migration patterns among HIV-positive MSM is crucial for targeted case management, yet comprehensive data from China remains limited.
Among 204,394 HIV-positive MSM, 20,117 (9.8%) migrated after diagnosis, with primary movement from economically developed regions like Guangdong Province and Shanghai Municipality to less developed provincial-level administrative divisions such as Sichuan Province and Anhui Province. Key predictors of migration included age under 50 years, unmarried status, lower educational attainment, employment as commercial staff or student status, and diagnosis before 2020.
Enhanced healthcare resources, strengthened case management systems, and targeted HIV-related services are essential to ensure consistent treatment access and improved health outcomes for migrant HIV-positive MSM.
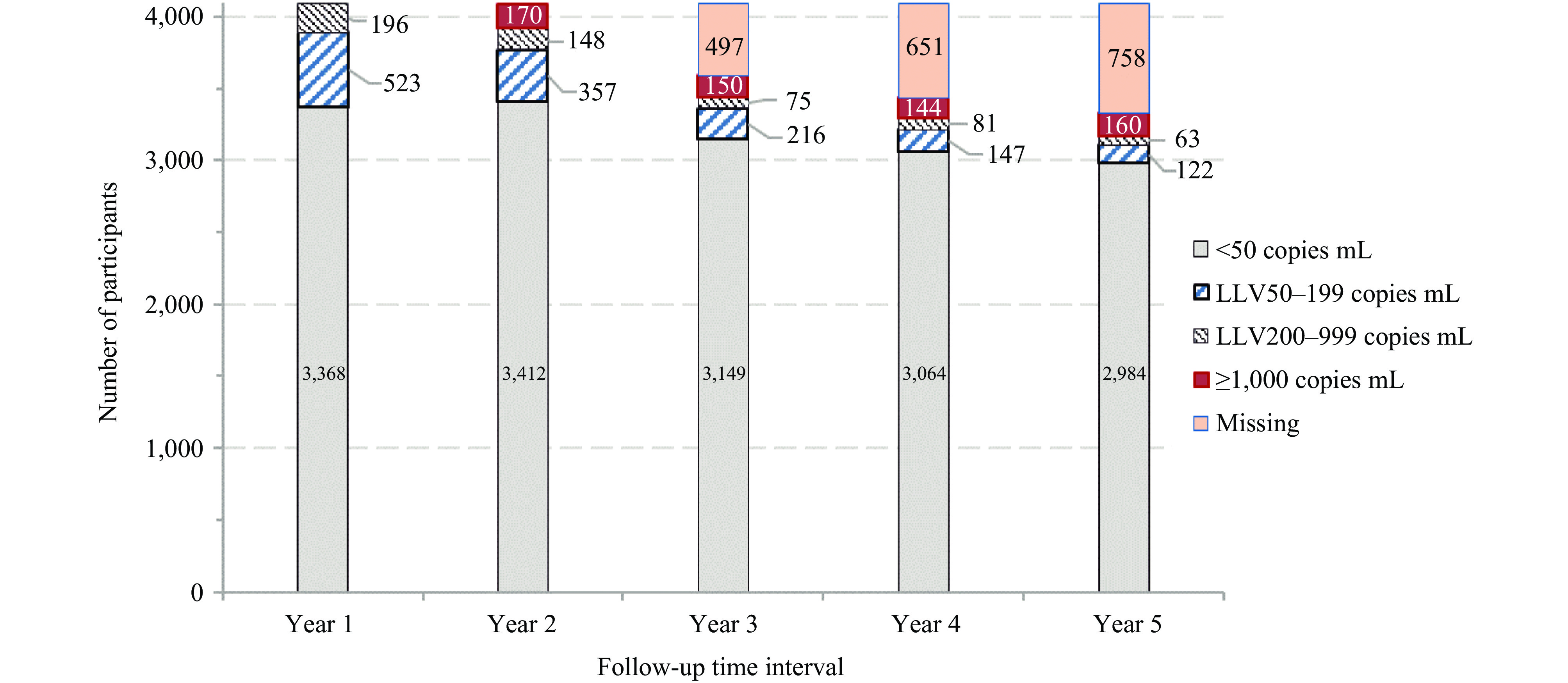
Human immunodeficiency virus (HIV) low-level viremia (LLV) during antiretroviral therapy (ART) occurs frequently in Dehong Dai and Jingpo Autonomous Prefecture, Yunnan Province.
Among people living with HIV who achieved virological success [viral load (VL) <1,000 copies/mL] after initiating ART in Dehong Prefecture, Southwest China, 17.6% experienced first-year LLV of 50–999 copies/mL First-year LLV emerged as an independent risk factor for subsequent viral non-suppression compared with participants maintaining first-year VL <50 copies/mL.
Enhanced monitoring and interventions for early LLV occurrence during the first year of ART are essential, including adherence education and timely VL testing.
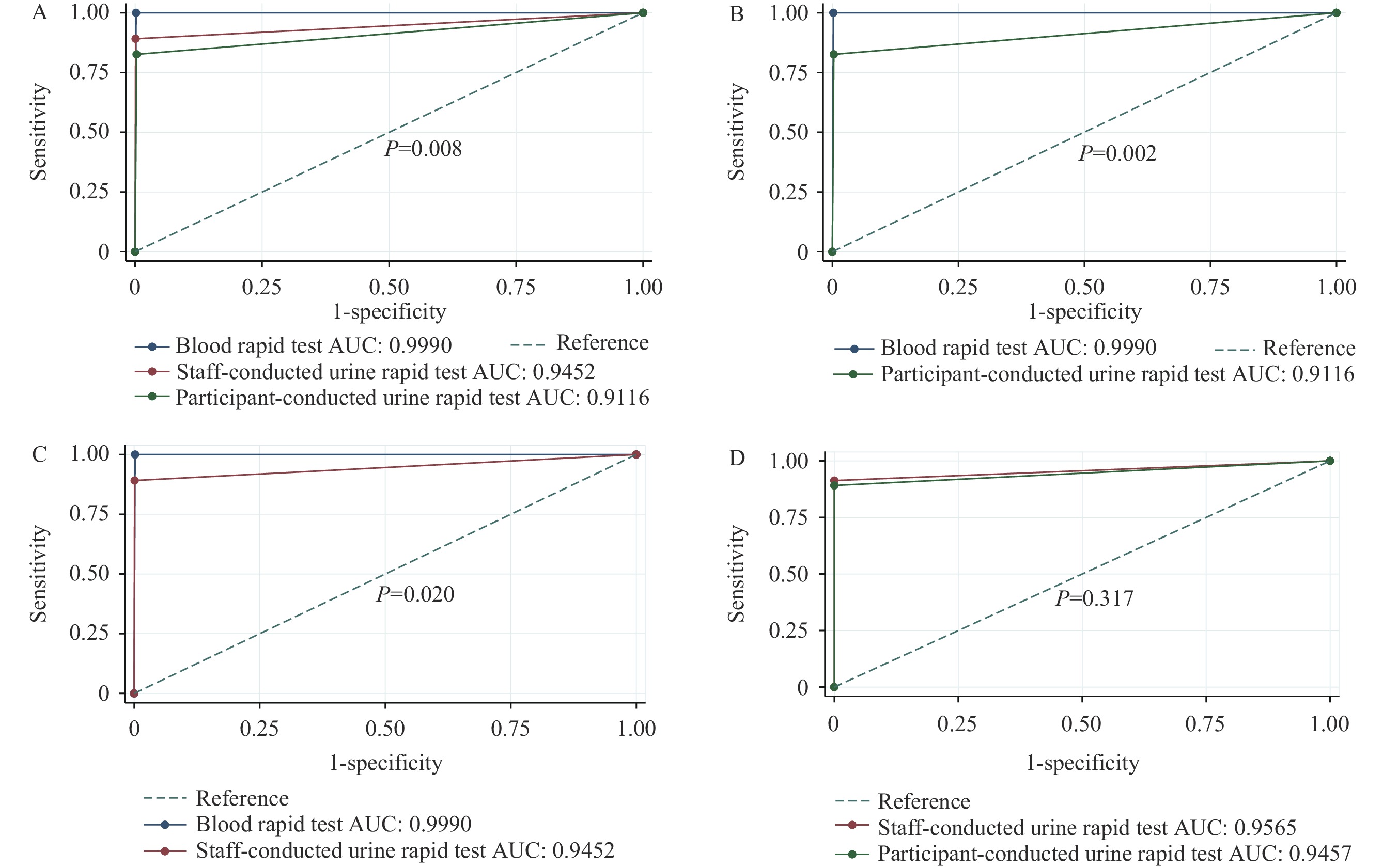
Human immunodeficiency virus (HIV) self-testing serves as a crucial strategy for overcoming testing barriers, with urine-based self-testing emerging as a potential novel approach.
In a real-world setting, this study demonstrated that the urine rapid test exhibited lower diagnostic accuracy compared to the blood rapid test. Study participants expressed stronger preferences for HIV self-testing methods utilizing finger prick samples, accompanied by standard written instructions and lower costs.
Our findings indicate that rapid urine testing requires additional validation before widespread implementation. Future development efforts should prioritize user-friendly HIV self-testing approaches to enhance testing accessibility.
China’s human immunodeficiency virus / acquired immune deficiency syndrome (HIV/AIDS) prevention and control efforts have entered a new stage, necessitating the exploration of more effective intervention strategies. HIV pre-exposure prophylaxis (PrEP) is a proven method to prevent HIV infection, but its promotion in China faces challenges such as low public acceptance and inadequate service capacity. To further promote PrEP, the “HIV PrEP Model Exploration Project” was launched, exploring three PrEP service models: PrEP clinics, Digital services and physical testing, and PrEP self-service vending machines. The project achieved certain results, establishing a PrEP service network, training professional staff, and promoting the use of PrEP. In the future, it is necessary to further expand publicity channels, enhance public awareness and acceptance, optimize follow-up management, and promote the popularization of PrEP and HIV/AIDS prevention and control efforts.



 Subscribe for E-mail Alerts
Subscribe for E-mail Alerts CCDC Weekly RSS Feed
CCDC Weekly RSS Feed