2025 Vol. 7, No. 26
Scrub typhus, also known as jungle typhus, is a vector-borne disease transmitted to humans through the bite of infected chiggers carrying Orientia tsutsugamushi. In recent years, it has reemerged as a significant public health concern in China, with cases being identified in an increasing number of previously unaffected regions.
Data were obtained from the China Information System for Disease Control and Prevention (CISDCP). We employed Joinpoint 5.1.0 for trend analysis and RStudio 4.4.1 for statistical analyses, including Mann-Whitney U tests (non-parametric), Cochran-Armitage tests, and binary logistic regression. SaTScan 9.1.1 and ArcGIS 10.7 were utilized to identify high-risk spatial clusters.
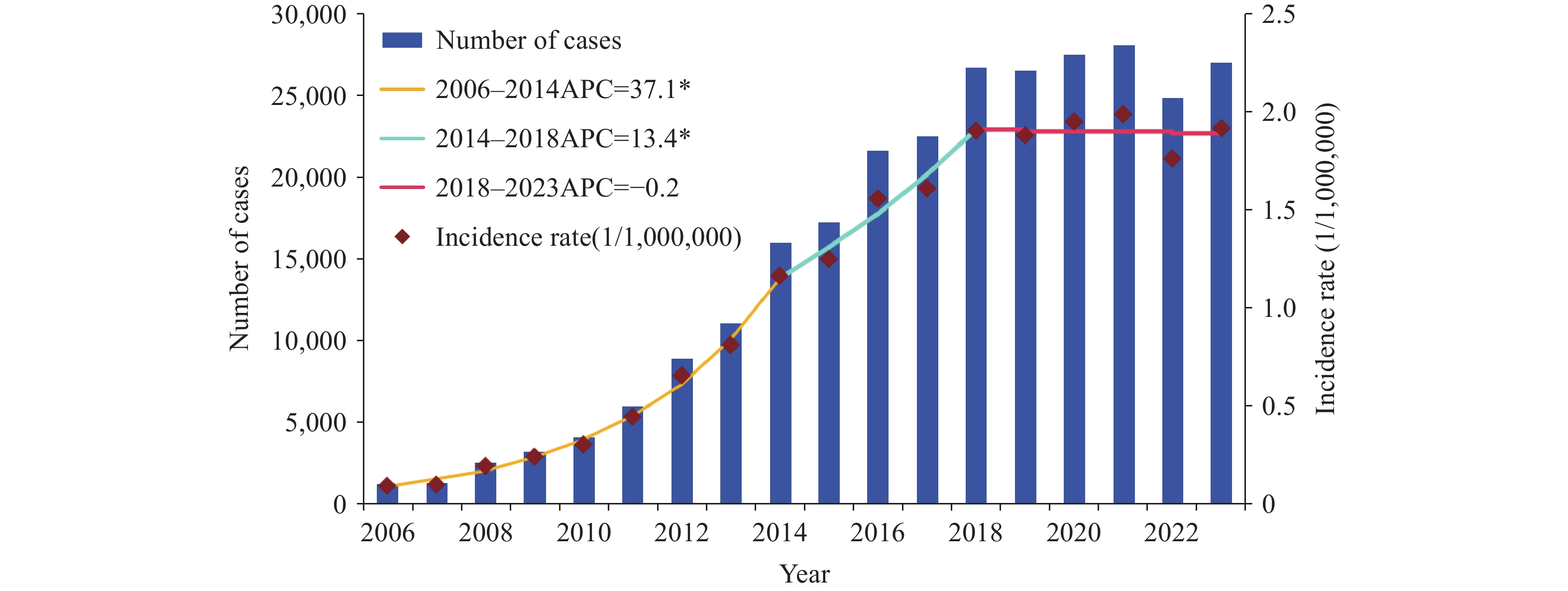
Scrub typhus incidence in China increased dramatically from 0.095/100,000 to 2.357/100,000 between 2006 and 2023. The epidemic trend was categorized into 3 distinct phases: a rapid increase period [APC2006-2013=37.1%, 95% confidence interval (CI): 31.4%, 43.0%], a slow increase period (APC2014-2018=13.4%, 95% CI: 4.6%, 23.0%), and a peak-plateau period (APC2019–2023=−0.2%, 95% CI: 3.2%, 3.0%), with annual cases ranging from 24,870 to 33,229. The proportion of individuals aged ≥45 years demonstrated an increasing trend (AAPC=2.0%). We identified 3 distinct seasonal patterns across China: summer, autumn, and summer-autumn patterns. This study revealed distinct spatiotemporal characteristics of scrub typhus in China, with the primary cluster concentrated in Yunnan Province and geographic expansion from southwestern, southern, and eastern regions toward central and northern China.
Scrub typhus incidence in China has increased substantially and has reached a peak plateau phase. The disease exhibits distinct spatiotemporal distribution patterns, necessitating targeted control measures in affected regions.
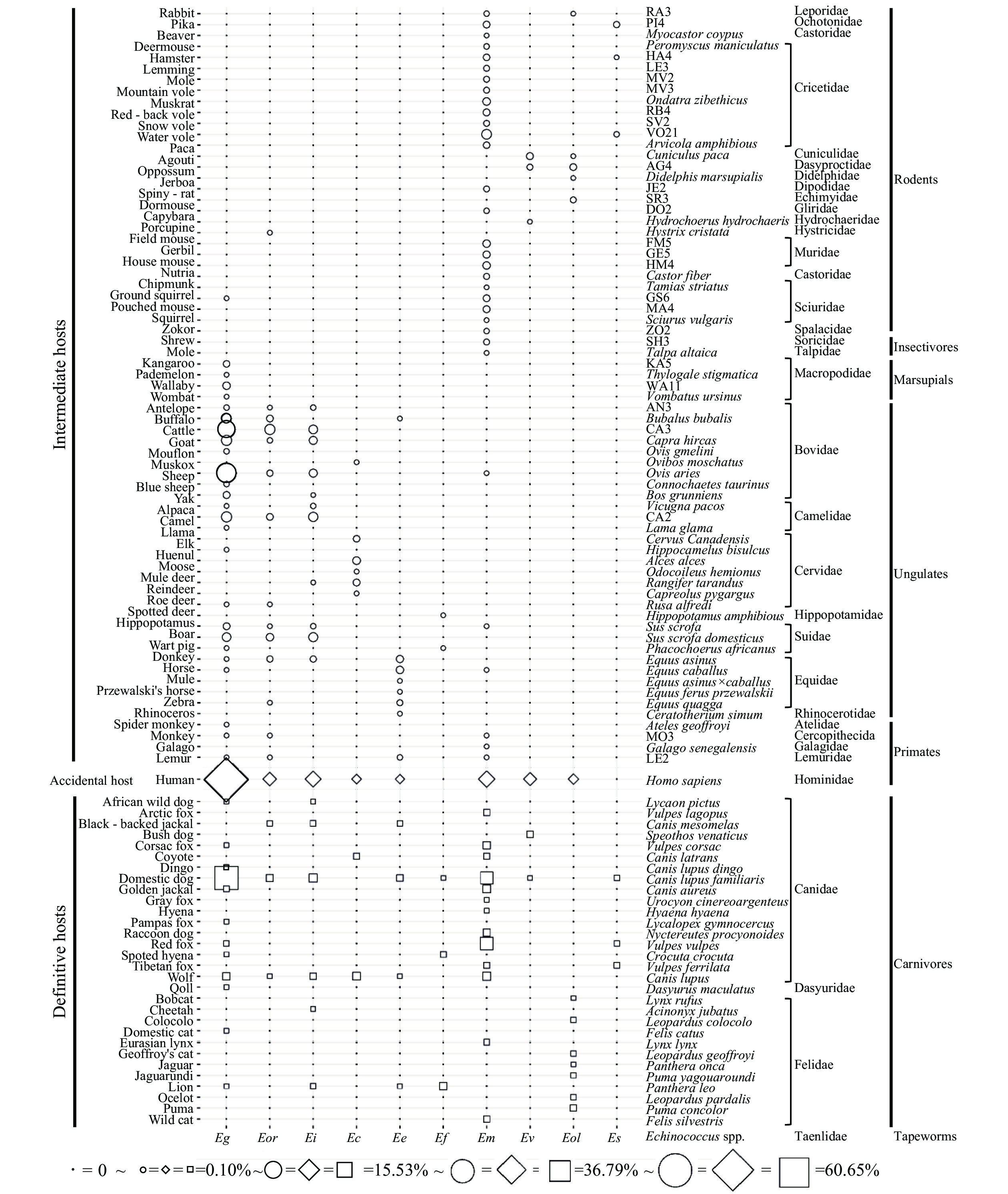
Echinococcosis is a serious public health concern caused by Echinococcus larvae. To date, 10 Echinococcus species have been identified globally, each with potential variations in geographic distribution and host selection.
This study presented the provincial-level distribution of all Echinococcus species globally and constructed a host frequency matrix for them. By quantifying both spatial and host niches, it provides comprehensive data for understanding the ecological adaptability of Echinococcus species and the transmission patterns of echinococcosis.
This study’s results highlight the interspecific heterogeneity and associations among different Echinococcus species, suggesting the need for targeted approaches in epidemiological investigations, source tracing, and risk surveillance to effectively control echinococcosis.
Artemisinin-based combination therapies (ACTs) remain the first-line treatment for uncomplicated malaria caused by P. falciparum, while chloroquine (CQ) serves as the primary treatment for P. vivax. However, the global spread of antimalarial drug resistance has become an increasing concern over time.
The integrated drug efficacy studies (iDES) demonstrated that artesunate (AS) plus dihydroartemisinin-piperaquine (DHA-PPQ) and chloroquine (CQ) remain effective first-line treatments for P. falciparum and P. vivax malaria, respectively. However, the occurrence of late treatment failure (LTF) and day 3 (D3) parasite positivity following treatment, suggests decreasing therapeutic efficacy. Molecular surveillance of P. falciparum resistance revealed novel mutation sites in pfK13 (S459T, N499T, A578S, and V692L) in addition to the previously reported F446I, P574L, and C580Y mutations. Concurrently, the difference in mutation patterns between pfcrt and pfmdr1 was significant (P<0.01), with the Y184F locus of the multidrug resistance gene pfmdr1 showing the highest mutation frequency at 40.5% of cases.
The iDES and molecular surveillance of antimalarial drug resistance indicated decreasing sensitivity to current first-line treatments. Continued surveillance of antimalarial drug resistance is vital for early warning and appropriate response to the spread of resistant parasites.
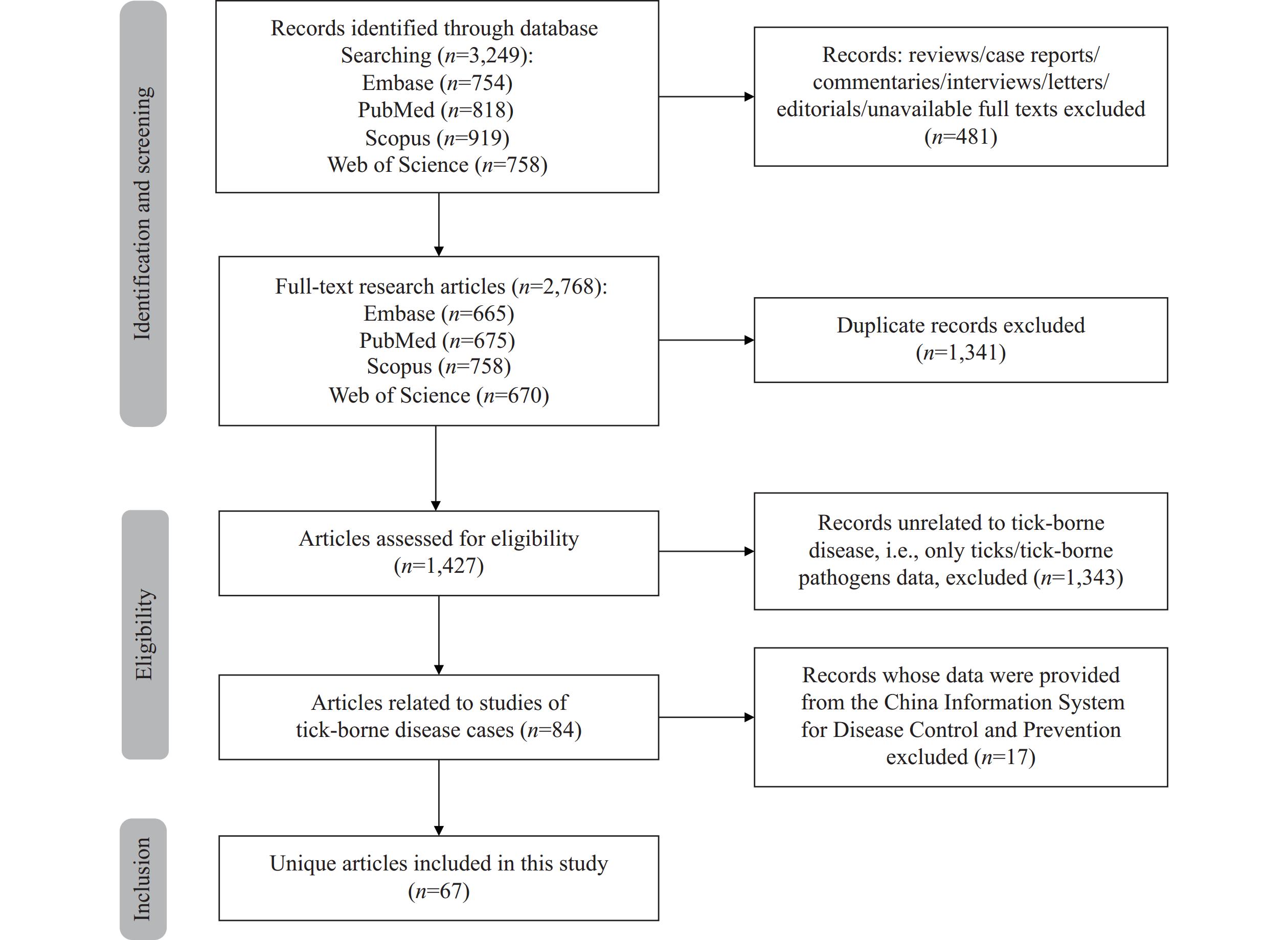
Tick-borne diseases (TBDs) pose a substantial threat to global public health, including China. This article systematically reviews the epidemiology of TBDs in Chinese mainland between 2003 and 2023. We retrieved and analyzed the incidence and distribution of notable bacterial, viral, and parasitic TBDs in China, and discussed their clinical characteristics, diagnostic approaches, and vectors. Severe fever with thrombocytopenia syndrome is the leading TBD in China, with cases rapidly increasing since its first report in 2009, and a high case fatality rate of 5%–33% in patients with severe disease. Other TBDs reported in China include spotted fever group rickettsiosis, human granulocytic anaplasmosis, Lyme borreliosis, babesiosis, and tick-borne encephalitis. Infections with emerging tick-borne pathogens, such as Yezo virus and Beiji nairovirus, have appeared very recently. Although evidence of human infection with Crimean-Congo hemorrhagic fever virus, Francisella tularensis, and Bartonella is currently unavailable, continuous monitoring of these pathogens remains necessary. This study enhances our understanding of TBDs, provides guidance for public health decision-making regarding important bacterial, viral, and parasitic TBDs, and offers new opportunities for TBD research in China.



 Subscribe for E-mail Alerts
Subscribe for E-mail Alerts CCDC Weekly RSS Feed
CCDC Weekly RSS Feed