2025 Vol. 7, No. 22
To evaluate the effectiveness of tobacco control efforts, we conducted a comprehensive analysis of trends in smoking cessation willingness and behavior among Chinese smokers from 2010 to 2024.
Data were obtained from the 2010 Global Adult Tobacco Survey (GATS)-China Project and the National Adult Tobacco Survey (NATS) conducted in 2018, 2022, and 2024. All surveys employed multistage stratified cluster random sampling of the Chinese population aged 15 years and above. Complex sampling analysis was performed for calculations, and trend analysis was conducted using the Cochran-Armitage trend test.
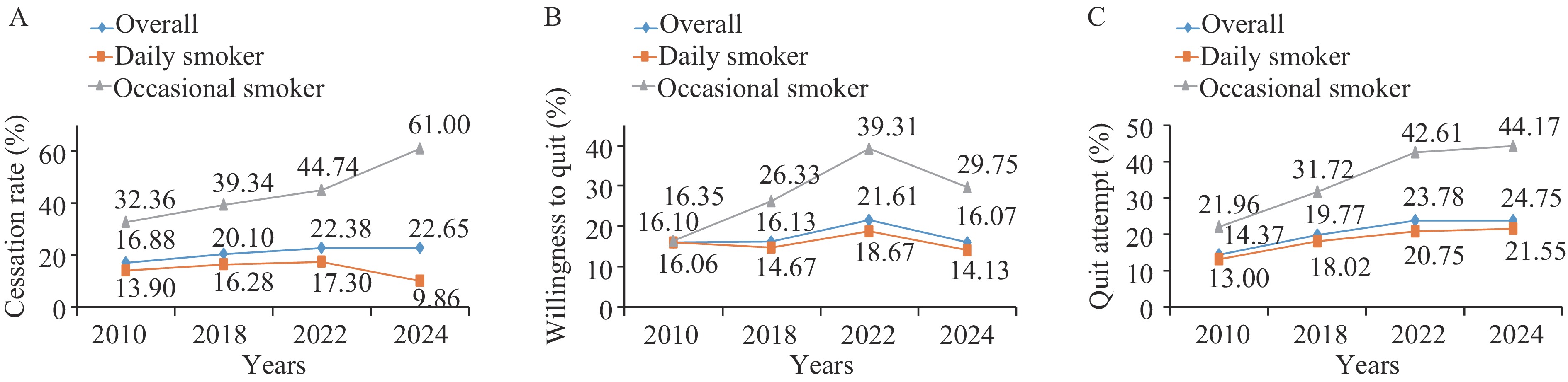
From 2010 to 2024, cessation behavior among Chinese smokers increased significantly. Cessation rates rose from 16.88% to 22.65%, and the proportion of smokers who attempted to quit in the past 12 months increased from 14.37% to 24.75%. The proportion of smokers planning to quit within 12 months increased from 16.10% to 21.61% from 2010 to 2022, but dropped to 16.07% in 2024. Over the 14-year period, cessation rates and quit attempts increased significantly across almost all demographic groups. However, from 2022 to 2024, cessation rates among daily smokers declined while the proportion of those willing to quit decreased. Occasional smokers consistently demonstrated higher cessation rates, quit attempts, and willingness to quit compared to daily smokers.
The observed increases in cessation behavior may be attributed to expanded smoking cessation services and extensive cessation campaigns implemented over the years. Enhanced cessation interventions should be targeted toward daily smokers. Pricing policies, graphic health warnings on packaging, and community-based comprehensive smoking cessation interventions can further enhance smokers’ willingness to quit and encourage more cessation attempts.
In 2018, the current and daily smoking prevalence among Chinese adults aged ≥15 years were 26.6% and 23.2%, respectively.
In 2024, China’s smoking prevalence among adults aged ≥15 years was 23.2% (current) and 20.3% (daily), with current smokers averaging 15.8 cigarettes/day and daily smokers initiating daily smoking at 22.4 years. Slim cigarette use accounted for 32.9% of current smokers.
Sustained reduction in tobacco use requires multifaceted interventions and rigorous controls on tobacco industry tactics that disseminate deceptive marketing of purported harm-reduction products.
The electronic cigarette (e-cigarette) market in China has been gradually expanding. Substantial evidence indicates that e-cigarettes pose considerable health risks to the human body.
The prevalence of e-cigarette ever use among Beijing residents aged ≥15 years ranged from 5.7% to 8.6% during 2016–2023, while current use ranged from 1.6% to 2.7%, with both metrics peaking in 2021. Current smokers who had attempted to quit within the past year showed the highest odds of e-cigarette use.
The public are not fully aware of the academic and clinical controversies regarding e-cigarettes' effectiveness for smoking cessation and may underestimate their health risks. There is an urgent need for targeted knowledge campaigns and for the provision of more accessible smoking cessation services.
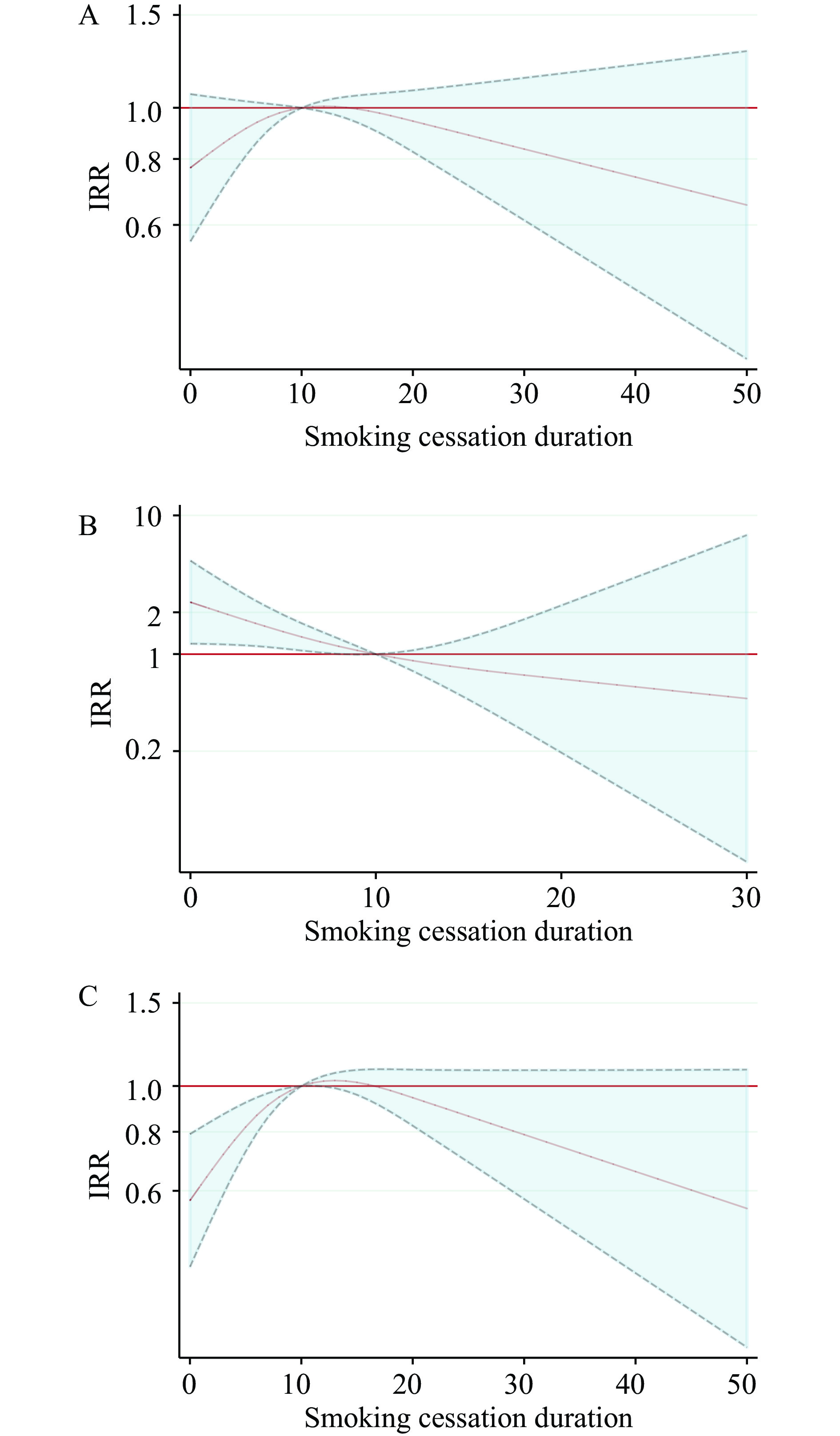
Smoking cessation can slow lung function decline and reduce exacerbation risk in patients with chronic obstructive pulmonary disease (COPD). However, the impact of smoking cessation duration on the frequency of exacerbation readmissions and associated healthcare costs remains poorly understood in real-world settings.
We conducted a retrospective cohort study that included 7,868 COPD patients from Beijing Chao-Yang Hospital. The 3-year exacerbation readmission rate and hospitalization costs declined with increasing duration of smoking cessation beyond 10 years, particularly among patients under 60 years of age.
Early smoking cessation and maintaining abstinence for more than 10 years could help reduce healthcare costs in patients with COPD, highlighting the importance of integrating smoking cessation interventions into COPD management.
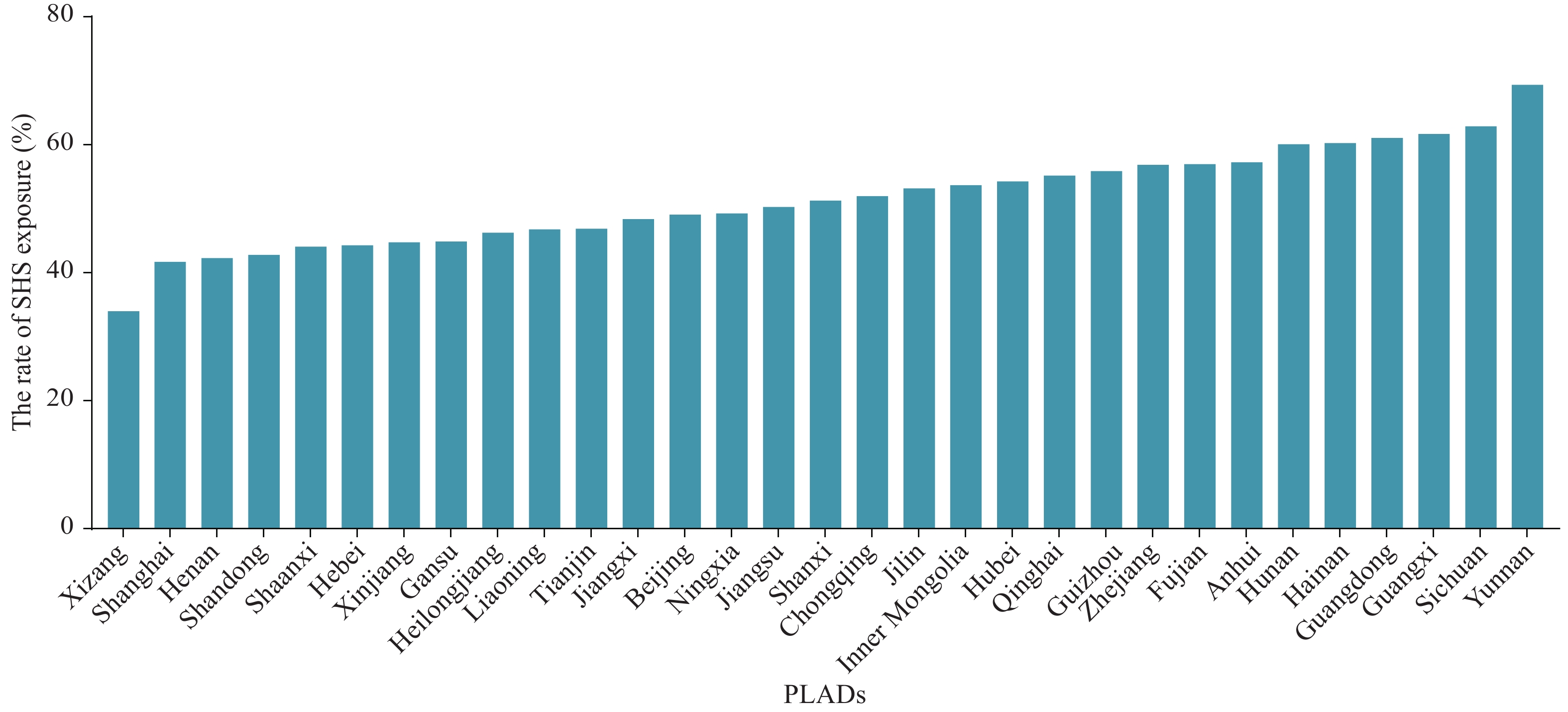
In 2018, the secondhand smoke (SHS) exposure rate among non-smoking adults aged 15 years and above in China was 68.1%.
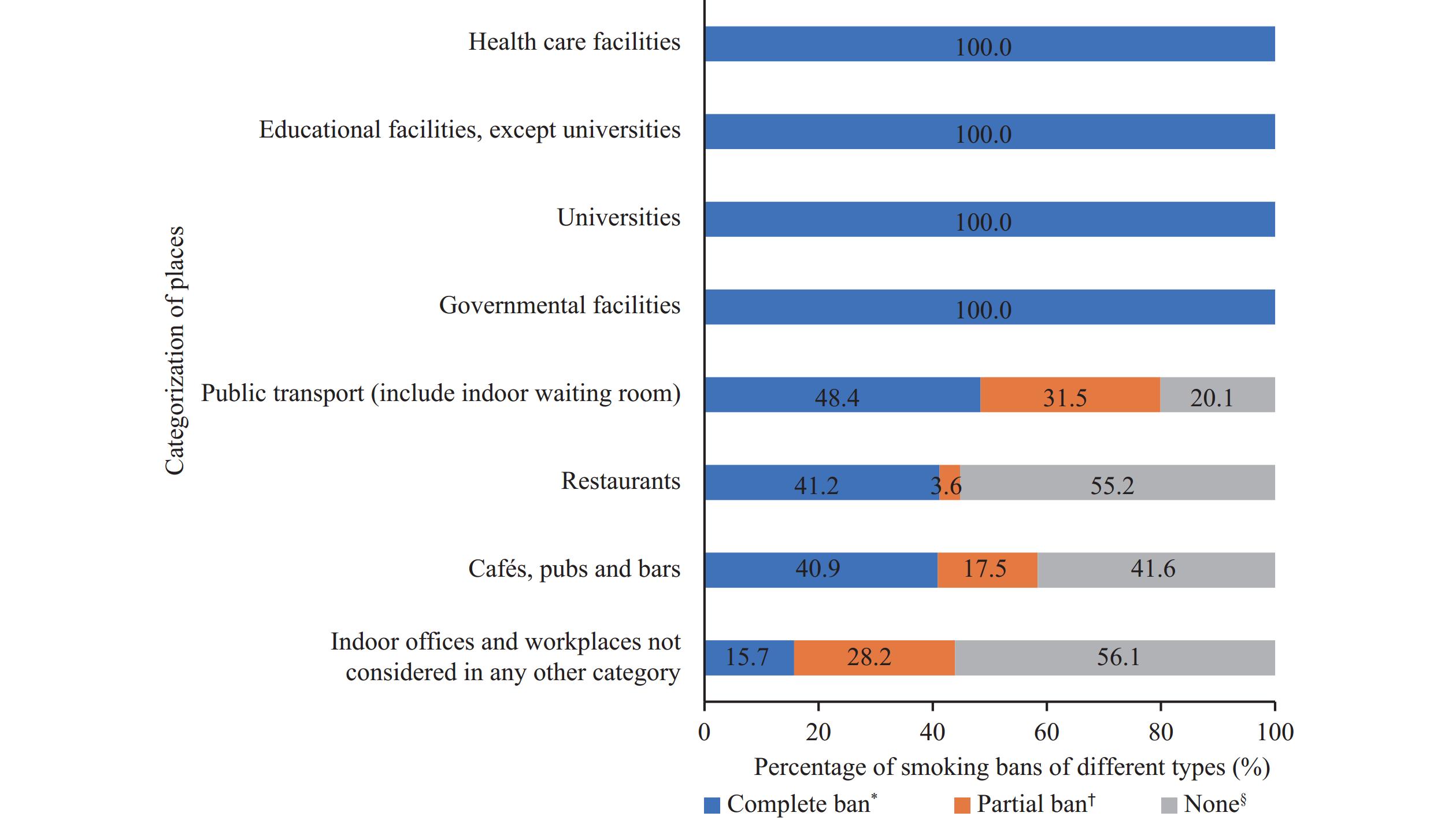
In 2022, the SHS exposure rate among non-smoking adults aged 15 years and above in China was 52.4%, with significant positive spatial correlation across regions. Key factors influencing regional SHS exposure included smoking rates, tobacco control measures in homes, indoor workplaces, and healthcare institutions, proportion of the population covered by comprehensive smoke-free regulations, and public awareness of SHS and smoking-related health risks.
Understanding the spatial heterogeneity and determinants of SHS exposure provides crucial insights for developing targeted, region-specific tobacco control strategies and interventions.



 Subscribe for E-mail Alerts
Subscribe for E-mail Alerts CCDC Weekly RSS Feed
CCDC Weekly RSS Feed