HTML
-
Introduction: Secondhand smoke (SHS) exposure remains a significant public health threat to human health. Understanding the spatial distribution characteristics of SHS exposure is essential for developing targeted, region-specific tobacco control strategies and interventions. This study analyzed the spatial clustering of SHS exposure and its influencing factors in China in 2022.
Methods: This study utilized data from the 2022 China National Adult Tobacco Survey (NATS). Descriptive statistical analyses were performed using Stata (version 17.0; StataCorp LLC, College Station, Texas, USA). Spatial analyses were conducted using GeoDa (version 1.22; Dr. Luc Anselin’s team, Arizona State, USA) to examine global spatial autocorrelation, local spatial autocorrelation and ordinary least squares (OLS) spatial regression. Provincial-level figures of SHS exposure rates were visualized using GraphPad Prism (version 9.5; GraphPad Software, Boston, USA).
Results: In 2022, the SHS exposure rate among non-smoking adults aged 15 years and above in China was 52.4%. The distribution of SHS exposure in China exhibited significant provincial clustering (Moran’s I=0.337, Z=4.626, P=0.001). LISA analysis identified High-High clusters of SHS exposure in Yunnan, Guizhou, Sichuan, Chongqing, Guangdong, and Hainan, while Henan emerged as a Low-Low cluster. Key factors influencing regional SHS exposure included smoking rates, tobacco control measures in homes, indoor workplaces, and healthcare institutions, population coverage of comprehensive smoke-free regulations, and cognition of SHS harm and smoking harm.
Conclusions: Although SHS exposure rates in China have decreased, they remain a significant concern. Targeted interventions should be implemented in southwestern and central southern China, with strengthened smoke-free management in key settings including homes, indoor workplaces, and medical institutions. Additionally, expanding the coverage of comprehensive smoke-free laws and regulations is recommended.
-
Secondhand smoke (SHS), defined as the combination of smoke exhaled by smokers and smoke emanating from burning cigarettes (1), represents a significant public health concern. The World Health Organization reports that SHS exposure claims approximately 1.3 million lives annually through various associated diseases (2–3). While China witnessed a modest decline in SHS exposure rates from 72.4% to 68.1% between 2010 and 2018 (4), recent trends remain unclear. Furthermore, the historical data from 2010–2018, while nationally representative, lacked provincial-level granularity, precluding spatial analysis at the provincial-level administrative divisions (PLADs) scale. The present study utilizes data from the 2022 China National Adult Tobacco Survey (NATS), which offers both national and provincial representativeness, to analyze current SHS exposure rates across China. By examining spatial distribution patterns and identifying key influencing factors, this research aims to inform the development of targeted, region-specific tobacco control strategies and measures.
The 2022 NATS employed a multi-stage, stratified, cluster probability sampling design to ensure both national and provincial representativeness. The sampling process consisted of five stages: First, 10 districts (counties) were selected from each PLAD using stratified sampling and probability proportional to size (PPS) methods, encompassing 363 monitoring points nationwide. Second, three streets (townships) were selected from each district (county) using PPS. Third, two neighborhood committees (administrative villages) were selected from each street (township) using PPS. Fourth, 60 households were randomly selected from each neighborhood committee (administrative village) using simple random sampling. Fifth, utilizing electronic devices to record household member information, one respondent from each household was randomly selected to complete the individual questionnaire. Data collection was conducted through an electronic survey system. Inclusion criteria comprised: 1) age ≥15 years; 2) non-collective Chinese residents; 3) primary residence at the survey address, regardless of household registration or consanguinity. Exclusion criteria included: 1) age <15 years; 2) unavailability during the survey period due to extended business trips or studies; 3) temporary visitors for tourism or family visits; 4) collective residence as primary address. Of 201,390 completed individual questionnaires, 182,278 were included in the final analysis after quality evaluation and data cleaning.
In the 2022 NATS, SHS exposure assessment was conducted through structured questions targeting non-smokers’ exposure patterns. The primary exposure metric was determined by the frequency question: “How many days per week are you exposed to someone smoking (SHS) usually? Almost every day, average 4–6 days a week, average 1–3 days a week, or not at all?” Participants reporting exposure frequencies of almost every day, 4–6 days per week, or 1–3 days per week were classified as having SHS exposure. Location-specific exposure rates over the past 30 days were evaluated through a series of questions addressing: 1) visitation to government buildings/offices, medical and healthcare institutions, restaurants, or public transportation; 2) presence of smoking activity at these locations (including self-smoking); 3) frequency of smoking occurrences in the home environment; and 4) presence of smoking in indoor workplaces.
Statistical analyses were performed using Stata (version 17.0; StataCorp LLC, College Station, Texas, USA) for complex sampling weight calculations, incorporating sampling weights, non-response adjustment weights, and post-stratified correction weights. Statistical significance was set at P<0.05. Spatial analyses were conducted using GeoDa (version 1.22; Dr. Luc Anselin’s team, Arizona State, USA) to examine spatial data matrices, spatial autoregression, and ordinary least squares (OLS) spatial regression models for analyzing influencing factors and spatial heterogeneity of SHS exposure. Using PLADs as spatial analysis units, the global Moran’s I index was employed to assess spatial autocorrelation of SHS exposure rates across 31 PLADs. This index ranges from [−1, 1], where positive values indicate positive correlation, negative values indicate negative correlation, and 0 indicates no spatial correlation, with stronger correlations represented by larger absolute values (5). Local indicators of spatial association (LISA) were utilized to identify SHS exposure clustering patterns, categorizing regions into four distinct clustering patterns: High-High (high-value regions surrounded by high-value regions), low-high, low-low, and high-low aggregation areas (6–7). Results visualization was accomplished using GraphPad Prism (version 9.5; GraphPad Software, Boston, USA).
In 2022, the national SHS exposure rate in China was 52.4%, with substantial regional variation ranging from 34.0% in Xizang Autonomous Region to 69.4% in Yunnan Province. Analysis of exposure patterns over the preceding 30 days revealed significant variations across different settings. Home exposure was reported by 41.3% of respondents (range: 23.9% in Shanghai Municipality to 67.3% in Yunnan), while 43.0% of indoor workers reported workplace exposure (range: 19.9% in Shanghai to 83.8% in Yunnan). Institutional exposure rates varied considerably: government buildings or offices at 18.3% (range: 7.4% in Henan Province to 32.4% in Xizang), public transportation at 9.2% (range: 1.7% in Shanghai to 37.1% in Xizang), and medical and healthcare institutions at 13.6% (range: 4.3% in Shanghai to 25.8% in Jiangxi Province). Restaurants demonstrated the highest exposure rates at 55.9%, ranging from 27.6% in Shanghai to 69.8% in Sichuan Province (Figures 1-2).
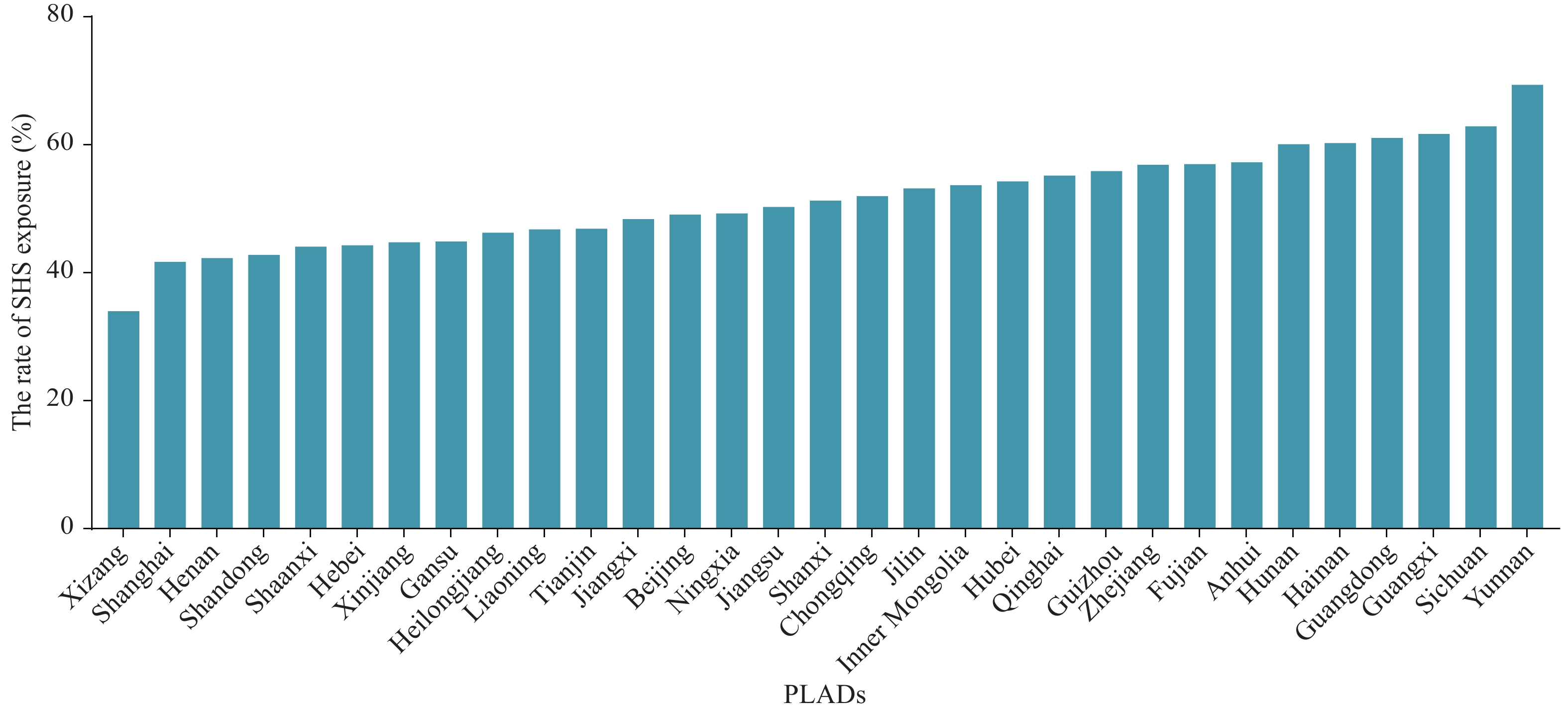 Figure 1.
Figure 1.The rate of SHS exposure in 31 PLADs in China, 2022.
Abbreviation: SHS=secondhand smoke; PLADs=provincial-level administrative divisions. Figure 2.
Figure 2.The rate of SHS exposure in various public places and indoor workplaces in 31 PLADs in China, 2022. (A) The rate of SHS exposure in home; (B) The rate of SHS exposure in indoor workplaces; (C) The rate of SHS exposure in government buildings or offices; (D) The rate of SHS exposure on public transportation; (E) The rate of SHS exposure in medical and healthcare institutions; (F) The rate of SHS exposure in restaurants.
Spatial autocorrelation analysis revealed significant positive correlation in the distribution of SHS exposure across China (Moran’s I=0.337, Z=4.626, P=0.001), indicating that areas with high SHS exposure rates tend to cluster with similarly high-exposure neighboring regions. The Local Indicators of Spatial Association (LISA) analysis identified distinct High-High clusters of SHS exposure in Yunnan, Guizhou, Sichuan, Chongqing, Guangdong, and Hainan, while Henan emerged as a significant Low-Low cluster, characterized by low SHS exposure rates both within the province and in adjacent regions. The areas with a high rate of SHS exposure are mainly concentrated in southwestern and south-central China.
OLS spatial regression analysis demonstrated several significant associations with SHS exposure rates. Regional smoking rates showed a strong positive correlation with SHS exposure (β=1.324, T=3.594, P=0.001). Conversely, stronger tobacco control measures were associated with lower SHS exposure rates across multiple settings: homes (β=−0.571, T=4.621, P<0.001), indoor workplaces (β=−0.446, T=−3.472, P=0.002), and medical and healthcare institutions (β=−0.539, T=−2.502, P=0.019). Additionally, higher population coverage by comprehensive smoke-free regulations was significantly associated with reduced SHS exposure (β=−4.002, T=−4.241, P<0.001). Regarding tobacco harm awareness, regions with higher recognition of SHS-related heart disease risks (β=−0.472, T=−2.682, P=0.012) and smoking-related risks of stroke (β=−0.438, T=−2.501, P=0.018) and heart disease (β=−0.483, T=−2.977, P=0.006) demonstrated significantly lower SHS exposure rates (Table 1).
Variable Moran’s I Coefficient β Std.Error T value R-square P Current smoking 0.170 1.324 0.368 3.594 0.332 0.001 Tobacco control strength in different places Home 0.205 −0.571 0.124 −4.621 0.451 <0.001 Indoor workplace 0.079 −0.446 0.129 −3.472 0.325 0.002 Government building 0.151 −0.359 0.214 −1.679 0.101 1.056 Medical and health care institutions 0.359 −0.539 0.215 −2.502 0.200 0.019 Restaurant 0.100 −0.207 0.128 −1.613 0.094 0.119 Public transportation 0.218 −0.323 0.243 −1.328 0.066 0.196 Proportion of the population covered by
comprehensive smoke-free regulations0.220 −4.002 0.944 −4.241 0.383 <0.001 Cognition of SHS harm Adults heart disease 0.212 −0.472 0.176 −2.682 0.199 0.012 Pediatric lung disease 0.239 −0.276 0.140 −1.971 0.118 0.058 Adult lung cancer 0.182 −0.333 0.179 −1.862 0.107 0.073 Cognition of smoking harm Stroke 0.341 −0.438 0.175 −2.501 0.177 0.018 Heart disease 0.261 −0.483 0.162 −2.977 0.234 0.006 Lung cancer 0.266 −0.341 0.190 −1.792 0.100 0.084 Erectile dysfunction 0.151 −0.243 0.190 −1.277 0.053 0.212 Abbreviation: OLS=ordinary least squares. Table 1. Regression coefficients of influencing factors based on spatial OLS model.
-
Our findings revealed substantial regional variations in SHS exposure across China. The overall SHS exposure rate decreased markedly from 68.1% in 2018 to 52.4% in 2022, indicating meaningful progress in China’s tobacco control initiatives. Notably, Yunnan Province exhibited the highest exposure rate at 69.4%, which can be attributed to its historically high smoking prevalence among both adolescents and adults, deeply entrenched smoking culture, and greater social tolerance of smoking behaviors (8-9). The absence of comprehensive tobacco control legislation and enforcement mechanisms in Yunnan further compounds this challenge.
Spatial analysis across China’s 31 PLADs revealed significant clustering patterns and spatial dependencies in SHS exposure. LISA analyses identified concentrated areas of high exposure in Yunnan, Guizhou, Sichuan, Chongqing, Guangdong, and Hainan PLADs, while Henan emerged as a notable cold spot. By the end of 2023, a total of 24 provinces had issued provincial tobacco control laws and regulations (10). However, Yunnan, Guizhou, Sichuan, Chongqing and Hainan had no provincial tobacco control laws and regulations. The geographical concentration of High-High clusters of SHS exposure in southwestern and south-central China precisely reflects the absence of provincial-level tobacco control legislation and enforcement mechanisms in these regions. The analysis results were consistent with the actual situation.
Our analysis demonstrates a direct correlation between smoking rates and SHS exposure levels across regions. Areas with more robust tobacco control measures, particularly in homes, indoor workplaces, and medical institutions, and higher proportions of populations protected by comprehensive smoke-free regulations exhibited significantly lower SHS exposure rates. This relationship is particularly notable in environments where people spend the majority of their time, such as homes and workplaces. The absence of stringent smoking restrictions in these settings substantially increases SHS exposure risks for family members, visitors, employees, and customers. Furthermore, the smoke-free status of medical and healthcare institutions serves as a key indicator of local health commissions’ commitment to tobacco control, often functioning as regional catalysts for broader tobacco control initiatives. The effectiveness of regional tobacco control measures appears to be directly linked to the leadership demonstrated by local health commissions in implementing and enforcing smoke-free policies.
Our results reveal that regions with lower SHS exposure rates consistently demonstrate higher public awareness of SHS-related cardiovascular risks and smoking’s impact on stroke and heart disease, along with greater implementation of smoke-free workplace policies. This association operates through two primary mechanisms. First, individuals with enhanced health risk awareness are more likely to adopt protective behaviors, such as avoiding SHS exposure or utilizing designated smoking areas. Second, while the link between smoking and lung cancer has been well-established through long-term public health campaigns, this awareness alone may no longer be sufficient to modify behavior. The recent emergence of cardiovascular and cerebrovascular diseases as prevalent public health concerns has made these conditions particularly salient factors in influencing regional SHS exposure patterns. To effectively reduce regional SHS exposure, a comprehensive approach is necessary, encompassing enhanced tobacco control awareness, robust monitoring systems, regular evaluations of control measures, and strengthened smoke-free legislation and environment creation.
This study has several limitations that warrant consideration. First, the reliance on self-reported SHS exposure data introduces potential measurement bias due to recall limitations among respondents. Second, the cross-sectional nature of the study precludes analysis of temporal dynamics, potentially limiting the comprehensiveness of our spatial analysis of SHS exposure patterns.
In conclusion, while China has made notable progress in tobacco control efforts, there remains a critical need for enhanced public health interventions. Future initiatives should focus on strengthening health education programs, elevating public awareness of SHS-related health risks, establishing robust SHS exposure monitoring systems, and implementing regular regional assessments. These measures will enable the development of more targeted and regionally-specific tobacco control strategies and interventions.
-
All staff members who contributed to data collection and participated in this study.
-
The 2022 China NATS received approval from the Chinese Center for Disease Control and Prevention Institutional Review Board in November 2021 (Approval Notice No. 202127).
| Citation: |



 Download:
Download:




