-
Introduction: The relationship between smoking cessation duration and subsequent healthcare utilization, particularly exacerbation readmissions and costs, remains unclear in patients with chronic obstructive pulmonary disease (COPD).
Methods: This retrospective cohort study included 7,868 COPD patients from Beijing Chao-Yang Hospital. Patients were classified by smoking status (never smokers, current smokers, and former smokers categorized by cessation duration: ≤10 years, 11–20 years, >20 years). We analyzed the association between smoking status and 3-year frequency of exacerbation readmissions and hospitalization costs.
Results: Over the three-year follow-up, 3,546 acute exacerbations of COPD (AECOPD) readmissions were documented, with an overall incidence rate of 0.15 per person-year. Compared with never smokers, the adjusted incidence rate ratios (IRRs) were 1.48 (1.05-2.07) for >20 years cessation, 2.17 (1.57–3.00) for 11–20 years, 1.77 (1.46–2.14) for ≤10 years, and 1.75 (1.44–2.13) for current smokers. Corresponding hospitalization costs were 1.35, 1.80, 1.37, and 1.28 (in 10,000 CNY), respectively, versus 0.80 in never smokers. Among patients aged <60 years, those who had quit for over 10 years had risks similar to never smokers. Restricted cubic spline analyses among former smokers indicated a nonlinear association between smoking cessation duration and AECOPD readmission risk, with risk peaking within 10 years of cessation and declining thereafter.
Conclusions: These findings reinforce the importance of early, sustained smoking cessation in COPD management. Smoking cessation may represent a cost-effective strategy to reduce healthcare expenditures.
-
Chronic obstructive pulmonary disease (COPD) is a major cause of morbidity and mortality in China, contributing significantly to healthcare burden through frequent hospitalizations for acute exacerbations of COPD (AECOPD) (1). Although smoking cessation is a well-established intervention that slows lung function decline, a substantial proportion of COPD patients remain current smokers (2). Clear evidence has demonstrated the health benefits of long-term smoking cessation (3). However, the duration of cessation required to achieve a reduction in exacerbation risk remains unclear, highlighting the need for quantitative evidence to better inform and motivate smoking cessation efforts in COPD patients. In this retrospective cohort study, we included 7,868 COPD patients and documented 3,546 AECOPD readmissions during a 3-year follow-up period. Current and former smokers had higher risks of AECOPD readmission and greater hospitalization costs than never smokers. Spline analyses revealed a nonlinear association, with risk peaking within 10 years of cessation and decreasing thereafter. These findings highlight the long-term health benefits of sustained smoking cessation in COPD patients. A sustained abstinence of over 10 years may be needed to meaningfully reduce the disease burden.
This retrospective cohort study utilized electronic medical records (EMRs) from Beijing Chao-Yang Hospital. We included COPD inpatients who were Beijing residents and hospitalized between January 2013 and December 2018. Eligible patients were required to have complete information on smoking history and a discharge International Classification of Diseases 10th Revision (ICD-10) code of J40–J44. For patients with multiple hospitalizations during the study period, only the first admission was included in the analysis.
Smoking information at the time of admission was extracted from unstructured texts in EMRs using natural language processing. Patients were classified into five groups according to smoking status: never smokers, former smokers who had quit for >20 years, former smokers who had quit for 11–20 years, former smokers who had quit for ≤10 years, and current smokers. Patients were followed up for 3 years after discharge. The outcomes were the frequency and hospitalization costs of AECOPD readmissions within the 3-year period. These outcomes were obtained through linkage with the Beijing hospital discharge database, which covers 245 secondary and tertiary hospitals in Beijing from 2013 to 2021. Negative binomial regression was used to estimate the association between smoking status and readmission frequency. To explore the exposure-response relationship between smoking cessation duration and the risk of AECOPD readmission, we fitted models with restricted cubic splines among former smokers. Generalized linear models with gamma distribution and log link were used to analyze hospitalization costs. Subgroup analyses by age explored age-related heterogeneity in effects of smoking cessation duration on outcomes. All statistical analyses were performed using Stata (version 15.1; StataCorp, College Station, TX, USA), with two-sided P<0.05 considered statistically significant.
A total of 7,868 COPD patients were included in the analysis. The mean age was 65.2±14.8 years, and 70.8% were men. Among them, 42.9% were never smokers, 34.7% were former smokers, and 22.4% were current smokers. The baseline characteristics of COPD patients are shown in Table 1. Over the three-year follow-up, 3,546 AECOPD readmissions were documented, with an overall incidence rate of 0.15 per person-year. After covariate adjustment, current and former smokers had higher risk of AECOPD readmission and greater hospitalization costs than never smokers. The incidence rate ratios (IRRs) were 1.48 (1.05–2.07) for >20 years cessation, 2.17 (1.57–3.00) for 11–20 years, 1.77 (1.46–2.14) for ≤10 years, and 1.75 (1.44–2.13) for current smokers. Corresponding hospitalization costs were 1.35, 1.80, 1.37, and 1.28 [in 10,000 Chinese Yuan (CNY)], respectively, versus 0.80 in never smokers. Among patients aged <60 years, those who had quit for over 10 years had risks similar to never smokers. In contrast, patients aged ≥60 years remained at higher risks and costs even after quitting for more than 10 years (Table 2). Restricted cubic spline analyses among former smokers indicated a nonlinear association between smoking cessation duration and AECOPD readmission risk, with risk peaking within 10 years after cessation and declining thereafter. In patients aged <60 years, readmission risk decreased linearly with increasing cessation duration (Figure 1).
Characteristics Never smoking Cessation >20 years Cessation 11–20 years Cessation ≤10 years Current smoking N 3,377 386 502 1,844 1,759 Age, mean (SD) 63.4 (17.7) 75.4 (11.0) 73.7 (8.8) 66.3 (10.4) 63.0 (12.5) Men, N (%) 1,506 (44.6) 332 (86.0) 447 (89.0) 1,694 (91.9) 1,588 (90.3) Asthma, N (%) 444 (13.1) 39 (10.1) 39 (7.8) 219 (11.9) 188 (10.7) Heart failure, N (%) 331 (9.8) 63 (16.3) 73 (14.5) 215 (11.7) 181 (10.3) Respiratory failure, N (%) 367 (10.9) 72 (18.7) 103 (20.5) 363 (19.7) 244 (13.9) Cerebrovascular disease, N (%) 385 (11.4) 65 (16.8) 82 (16.3) 194 (10.5) 199 (11.3) Cancer, N (%) 225 (6.7) 26 (6.7) 36 (7.2) 147 (8.0) 173 (9.8) Charlson Comorbidity Index, N (%) 0–1 1,763 (52.2) 154 (39.9) 190 (37.8) 927 (50.3) 787 (44.7) 2 800 (23.7) 119 (30.8) 150 (29.9) 486 (26.4) 477 (27.1) 3 414 (12.3) 58 (15.0) 69 (13.7) 217 (11.8) 290 (16.5) ≥4 400 (11.8) 55 (14.2) 93 (18.5) 214 (11.6) 205 (11.7) Emergency admission, N (%) 103 (3.1) 16 (4.1) 18 (3.6) 57 (3.1) 57 (3.2) White blood cell count, median (IQR) 6.4 (5.1, 8.1) 6.6 (5.4, 8.4) 6.7 (5.2, 8.5) 6.9 (5.5, 8.7) 7.0 (5.6, 8.8) Neutrophil percentage, median (IQR) 63.7
(55.0, 72.7)67.7
(60.2, 77.2)68.6
(60.5, 78.2)67
(58.7, 76.1)64.4
(55.8, 73.7)Lymphocyte percentage, median (IQR) 26.2
(18.0, 33.9)20.4
(13.7, 28.2)20.0
(13.0, 27.9)22.2
(15.0, 29.7)25.6
(17.3, 32.9)Eosinophil percentage, median (IQR) 1.9 (0.8, 3.5) 1.9 (0.6, 3.6) 1.8 (0.6, 3.4) 2.0 (0.6, 3.7) 1.9 (0.7, 3.3) Basophil percentage, median (IQR) 0.3 (0.2, 0.5) 0.3 (0.1, 0.4) 0.2 (0.1, 0.4) 0.3 (0.2, 0.5) 0.3 (0.2, 0.5) AECOPD hospitalization in the
previous year, N (%)200 (6.0) 38 (10.1) 52 (10.5) 188 (10.3) 87 (5.0) ICU admission, N (%) 85 (2.5) 12 (3.1) 24 (4.8) 58 (3.1) 46 (2.6) Mechanical ventilation, N (%) 95 (2.8) 15 (3.9) 30 (6.0) 87 (4.7) 73 (4.2) Length of stay, median (IQR) 10 (7,13) 10 (8,13) 10 (8,13) 10 (8,13) 10 (7,13) Abbreviation: COPD=chronic obstructive pulmonary disease; IQR=interquartile range; ICU=intensive care unit. Table 1. Baseline characteristics by smoking status in COPD patients.
Outcomes Never
smokingCessation >20
yearsCessation 11–20
yearsCessation ≤10
yearsCurrent
smokingOverall N 3,377 386 502 1,844 1,759 Incidence rate (/person-year) 0.1 0.21 0.25 0.2 0.15 Adjusted incidence rate ratio
(95% CI)1 1.48 (1.05–2.07) 2.17 (1.57–3.00) 1.77 (1.46–2.14) 1.75 (1.44–2.13) Costs (95% CI)(10,000 CNY) 0.80 (0.60–1.00) 1.35 (0.81–1.90) 1.80 (1.22–2.38) 1.37 (1.11–1.63) 1.28 (1.01–1.55) Age <60 years N 1,118 33 35 430 610 Incidence rate (/person-year) 0.1 0.04 0.02 0.05 0.09 Adjusted incidence rate ratio
(95% CI)1 0.39 (0.10–1.57) 0.94 (0.26–3.33) 1.82 (1.10–3.01) 1.70 (1.06–2.72) Costs (95% CI)(10,000 CNY) 0.46 (0.08–0.84) 0.20 (0.00–0.54) 0.39 (0.00–0.54) 1.19 (0.18–2.20) 0.86 (0.11–1.61) Age ≥60 years N 2,259 353 467 1,414 1,149 Incidence rate (/person-year) 0.13 0.25 0.27 0.19 0.19 Adjusted incidence rate ratio
(95% CI)1 1.87 (1.42–2.47) 1.95 (1.52–2.50) 1.53 (1.22–1.90) 1.66 (1.34–2.05) Costs (95% CI)(10,000 CNY) 0.86 (0.71–1.01) 1.60 (0.97–2.22) 2.20 (1.50–2.89) 1.47 (1.21–1.72) 1.56 (1.22–1.90) Note: Model adjusted for age, sex, admission year, AECOPD hospitalization in previous year, Charlson Comorbidity Index, cancer, heart failure, respiratory failure, mechanical ventilation, and ICU admission. Predictive margins for hospitalization costs were calculated.
Abbreviation: AECOPD=acute exacerbation of chronic obstructive pulmonary disease; CNY=Chinese yuan; CI=confidence interval.Table 2. The effect of smoking on the frequency and costs of AECOPD readmission in 3 years.
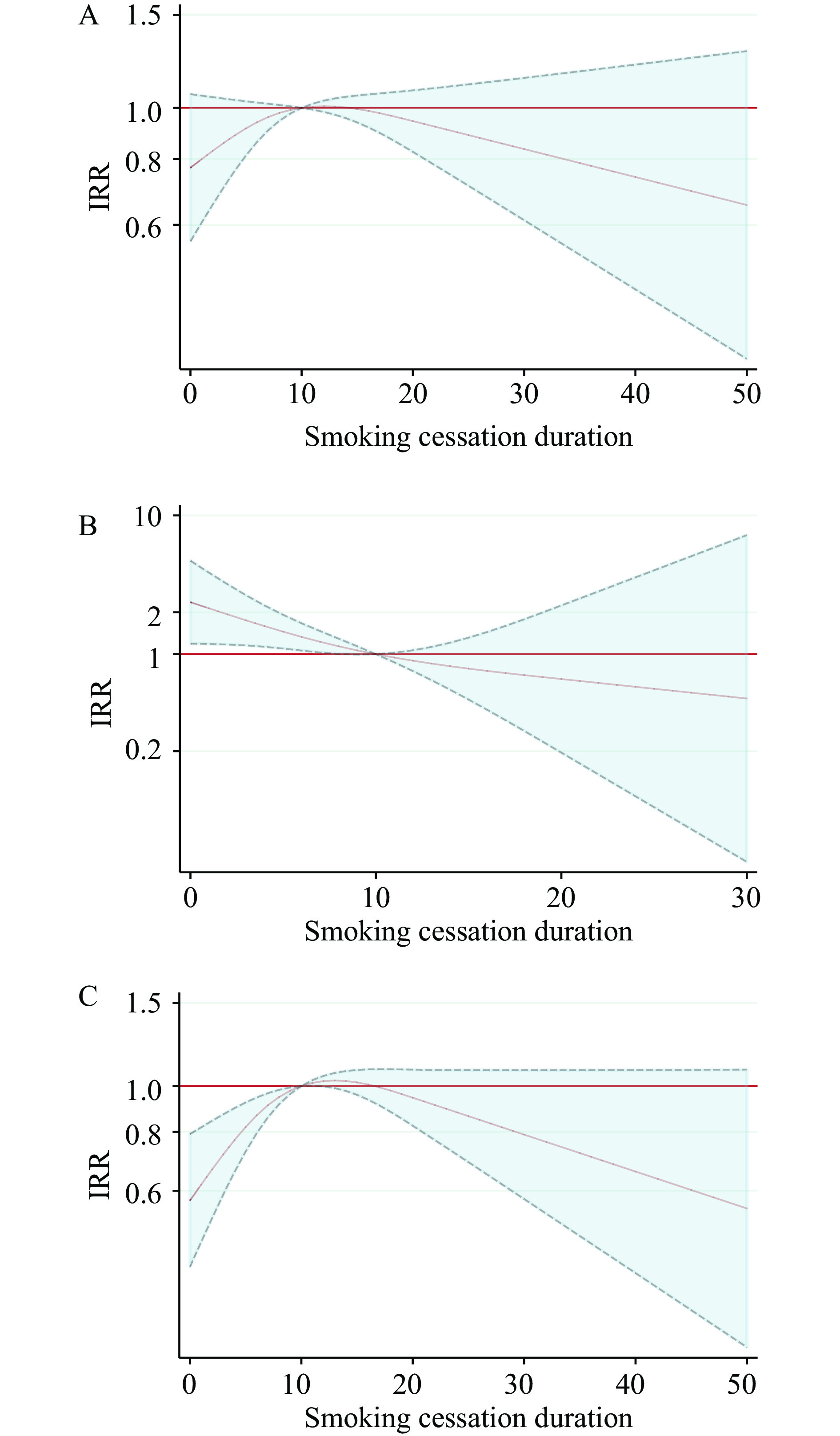 Figure 1.
Figure 1.Smoking cessation duration and AECOPD readmission frequency in 3 years among former smokers. (A) Overall; (B) Under 60 years old; (C) Aged 60 and above.
Note: Duration (years) of smoking cessation was included as restricted cubic spline terms in the negative binomial regression model, using three knots at the 25th, 50th, and 75th percentiles. Covariates included age, sex, admission year, AECOPD hospitalization in previous year, Charlson Comorbidity Index, cancer, heart failure, respiratory failure, mechanical ventilation, and ICU admission. The reference cessation duration was 10 years.
Abbreviation: AECOPD=acute exacerbation of chronic obstructive pulmonary disease; IRR=incidence rate ratio.
-
In this large, real-world cohort of hospitalized COPD patients, we found that current and former smokers had significantly higher risks of AECOPD readmissions and increased hospitalization costs compared to never smokers over a 3-year follow-up period. The incidence rate of AECOPD readmission decreased with longer cessation duration among patients who had quit smoking for over 10 years, with those under 60 years of age showing risks similar to never smokers. These findings emphasize the importance of continued smoking cessation interventions for COPD patients to reduce disease burden and healthcare costs.
Despite the well-established benefits of smoking cessation, cessation rates among COPD patients remain low (4). Previous research has demonstrated that long-term smoking cessation (>10 years) is associated with reduced risk of death and hospitalization (5). However, few studies have examined the impact of smoking cessation on the frequency of recurrent AECOPD events. Our findings contribute to the growing body of evidence on the benefits of long-term smoking cessation in reducing both the frequency and costs of AECOPD readmissions. We observed that former smokers with longer cessation durations (>10 years) experienced lower readmission risks, particularly among patients under 60 years of age. This aligns with previous studies showing that the benefits of smoking cessation accumulate over time, with substantial risk reduction after 10 years of abstinence (6).
We observed age-related differences in the association between smoking cessation duration and AECOPD readmission risk. Among patients younger than 60 years, longer cessation duration was consistently associated with lower readmission risk, suggesting that younger individuals derive more immediate and sustained benefits from quitting smoking. The health benefits of smoking cessation appear to be delayed and attenuated in older COPD patients, likely reflecting three interrelated mechanisms: extensive cumulative tobacco exposure causing irreversible airway remodeling, age-related cellular senescence limiting alveolar repair and inflammation resolution, and a higher comorbidity burden. These findings emphasize the importance of early smoking cessation in COPD patients to maximize long-term respiratory benefits.
The comparable risks observed between current smokers and recent quitters (<10 years) suggest that the deleterious effects of smoking may persist for several years after cessation. Similarly, a previous study found that patients who had quit smoking for less than 5 years experienced higher annual hospitalization rates for COPD compared to current smokers (7). We found that patients who had quit for less than 10 years still had elevated white blood cell counts, indicating persistent systemic inflammation despite smoking cessation. Compared to patients with cardiovascular diseases, COPD patients tend to experience slower and less pronounced benefits from smoking cessation due to irreversible airway damage and persistent systemic inflammation (8). Therefore, maintaining long-term smoking abstinence is crucial for COPD patients to achieve meaningful health benefits.
Frequent AECOPD hospitalizations constitute a major contributor to the economic burden of COPD. Our findings revealed that never smokers had significantly lower total hospitalization costs for AECOPD over the 3-year follow-up period compared to ever smokers, consistent with previous research (9). The elevated hospitalization costs among current and former smokers likely stem from more frequent exacerbations. Smoking cessation may therefore represent a cost-effective strategy for COPD management to reduce healthcare expenditures. From a public health perspective, our results highlight an urgent need to strengthen smoking cessation support among COPD patients. Future studies should conduct cost-effectiveness analyses to evaluate the impact of smoking cessation interventions on healthcare utilization and patient outcomes in COPD patients.
Several limitations should be acknowledged. First, this was a single-center study conducted in a tertiary hospital and a leading institution for respiratory medicine in Beijing. The benefits of long-term smoking cessation may be more pronounced in this population of severe COPD inpatients, potentially limiting generalizability to patients with milder COPD. Second, smoking status and cessation duration were based on medical records and may be subject to misclassification or recall bias. Third, residual confounding by disease severity could affect the association estimates. Additionally, the competing risk of death may bias the results, as patients who died would have no opportunity for subsequent readmissions, potentially leading to an underestimation of the benefits of smoking cessation. Nevertheless, smoking cessation duration remained significantly associated with the frequency of readmissions.
In conclusion, the 3-year AECOPD readmission rate and hospitalization costs declined with increasing duration of smoking cessation beyond 10 years, particularly among patients under 60 years of age. These findings reinforce the importance of early, sustained tobacco cessation in COPD care and suggest that cessation duration should be incorporated into clinical management and public health planning. Integrating smoking cessation interventions into the comprehensive management of COPD may help patients maintain long-term cessation and reduce the frequency and costs of exacerbation readmissions.
-
Approved by the Research Ethics Board of the Beijing Chao-Yang Hospital (2022-ke-473).
HTML
| Citation: |



 Download:
Download:




