2025 Vol. 7, No. 15
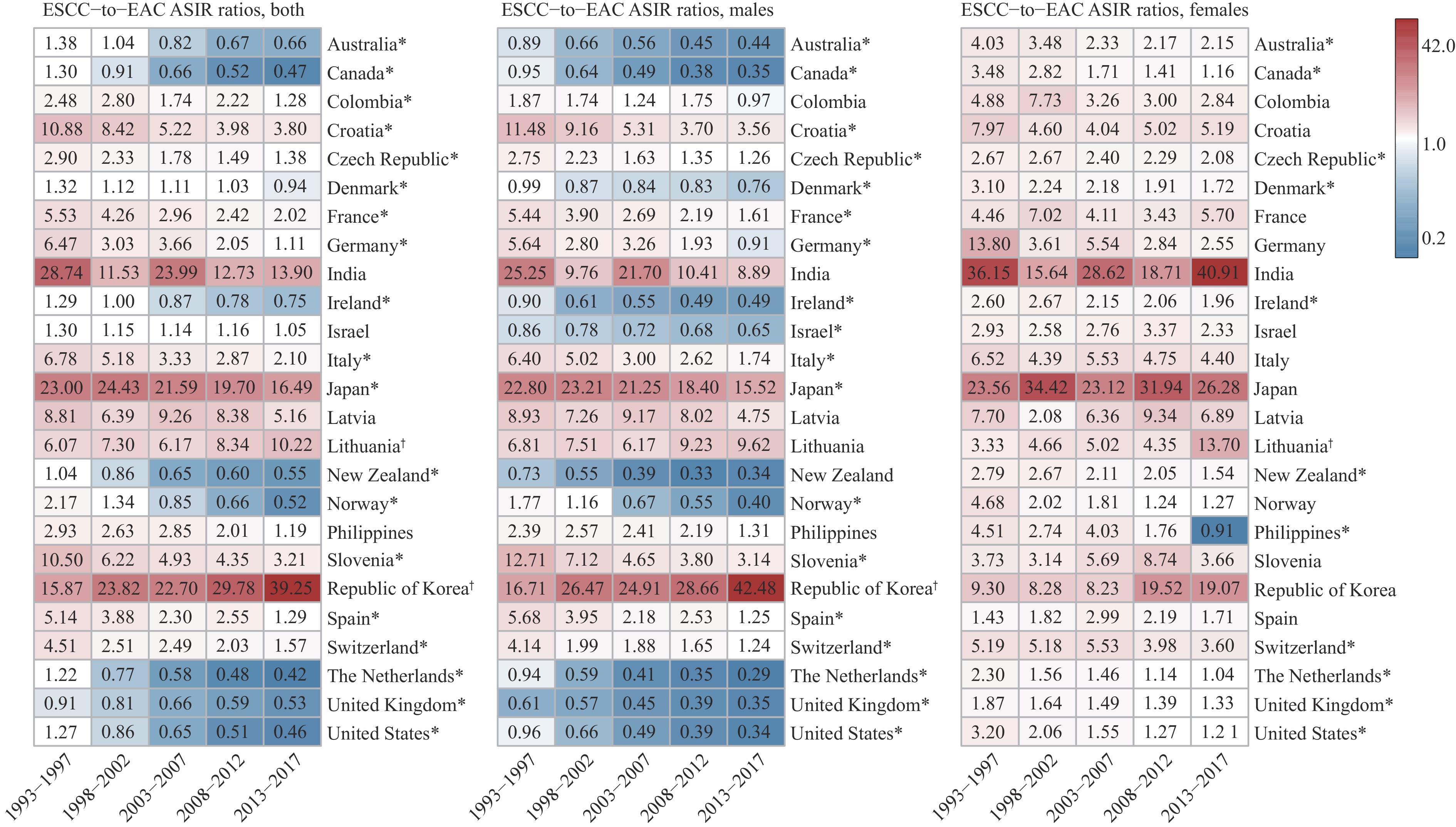
Esophageal cancer (EC) consists of two main histological subtypes: esophageal squamous cell carcinoma (ESCC) and esophageal adenocarcinoma (EAC), each with distinct epidemiological patterns. Historically, ESCC has been the dominant subtype worldwide, especially in Asian countries. However, in recent decades, the incidence of EAC has been rising rapidly, particularly in European and American countries, reflecting significant shifts in global EC epidemiology.
This study presents a comprehensive analysis of 25 years of high-quality continuous data on ESCC and EAC incidence trends across 25 countries. It highlights declining ESCC rates in most regions, rising EAC rates in Western nations, pronounced sex differences, and narrowing ESCC-to-EAC ratios. These diverse trends reveal the need to investigate region-specific risk factors and their contributions to the shifting burden of EC globally.
The distinct trends of ESCC and EAC call for tailored public health strategies based on regional and histological patterns. Countries experiencing a rising burden of EAC or ESCC can implement targeted risk factor prevention and control measures to address the increasing trends. In clinical practice, a stronger focus on EAC in high-income countries and ESCC in regions, where it remains dominant, can improve early detection and treatment outcomes. Understanding these evolving patterns will aid in designing evidence-based interventions and optimizing resource allocation to reduce the global esophageal cancer burden effectively.
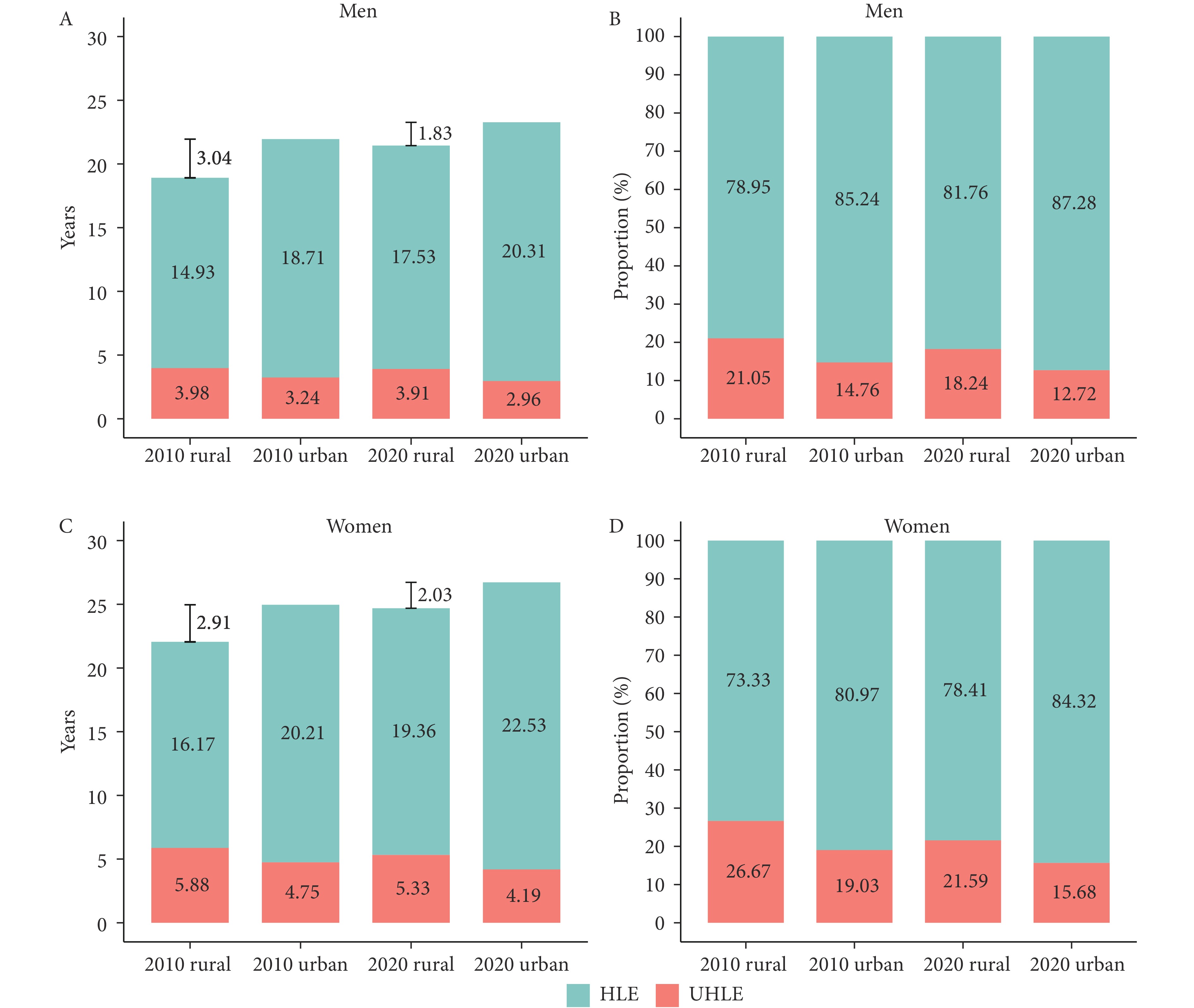
As China’s population ages rapidly, there is growing concern about whether increases in life expectancy are accompanied by improvements in healthy longevity for older adults.
From 2010 to 2020, healthy life expectancy expanded across different subgroups of the older population. Although urban-rural disparities in healthy life expectancy narrowed, morbidity has emerged as the primary contributor to these gaps, with the age groups driving these differences shifting toward older ages.
As longevity increases, health inequalities are transitioning from mortality-focused to morbidity-driven. This trend underscores the need for healthcare and elder care systems to address non-fatal health conditions affecting quality of life, particularly for women and the oldest-old.
Uncontrolled diabetes can result in severe clinical complications, significantly increasing the risk of functional limitations in instrumental activities of daily living (IADL) and activities of daily living (ADL).
This study investigates the association between the Cascade of Care (CoC) for diabetes and functional limitations, providing evidence on the critical need for strengthening diabetes care to prevent functional limitations and improve quality of life.
The findings provide critical insights to guide public health strategies and interventions aimed at enhancing diabetes management across all stages of the CoC, with the goal of reducing functional limitations and their associated burden, ultimately improving long-term health outcomes for individuals with diabetes.
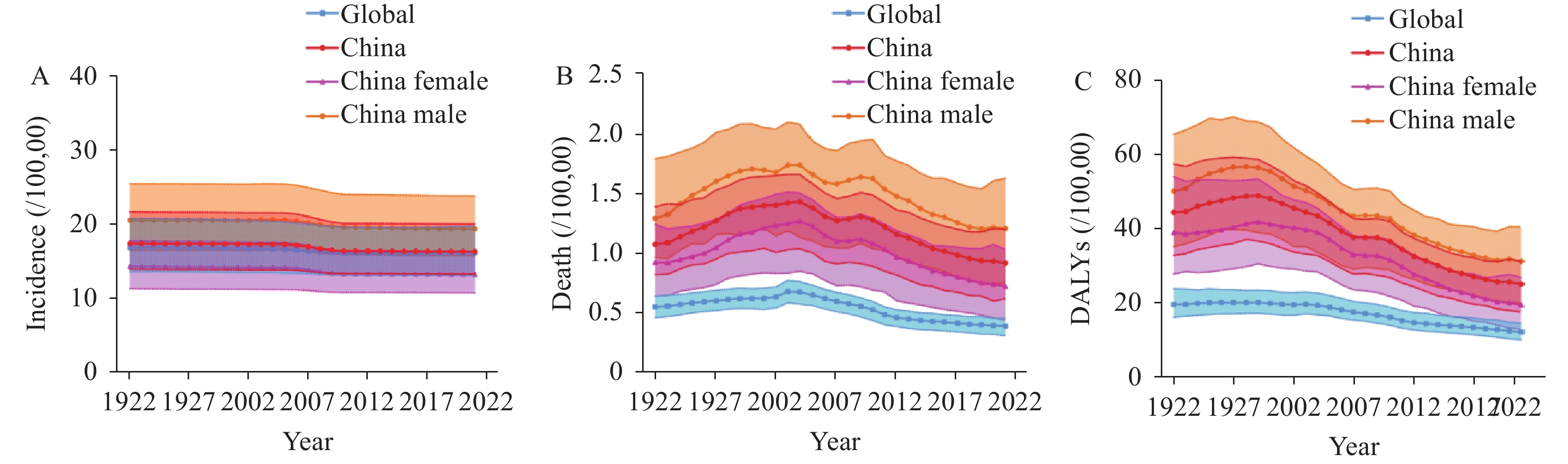
Myocarditis is a prevalent cardiovascular condition that can lead to severe complications. The number of patients with myocarditis, new cases, and deaths in China has been on an upward trend over the years, causing a certain disease burden.
The overall burden of myocarditis in China is on a downward trend; however, the age-standardized mortality rate (ASMR) and age-standardized disability-adjusted life years (DALYs) rate remain higher than the global average. The age-standardized incidence rate (ASIR), ASMR and age-standardized DALYs rate were higher in men than in women. Individuals younger than 5 years or older than 70 years, the period from 2002−2016, and birth cohort earlier than 1957 were identified as risk factors for myocarditis-related mortality.
We should still prioritize the prevention and treatment of myocarditis. It is recommended that primary and secondary prevention efforts focus on individuals younger than 5 years, older than 70 years, and males, with an emphasis on proactive health education and management.
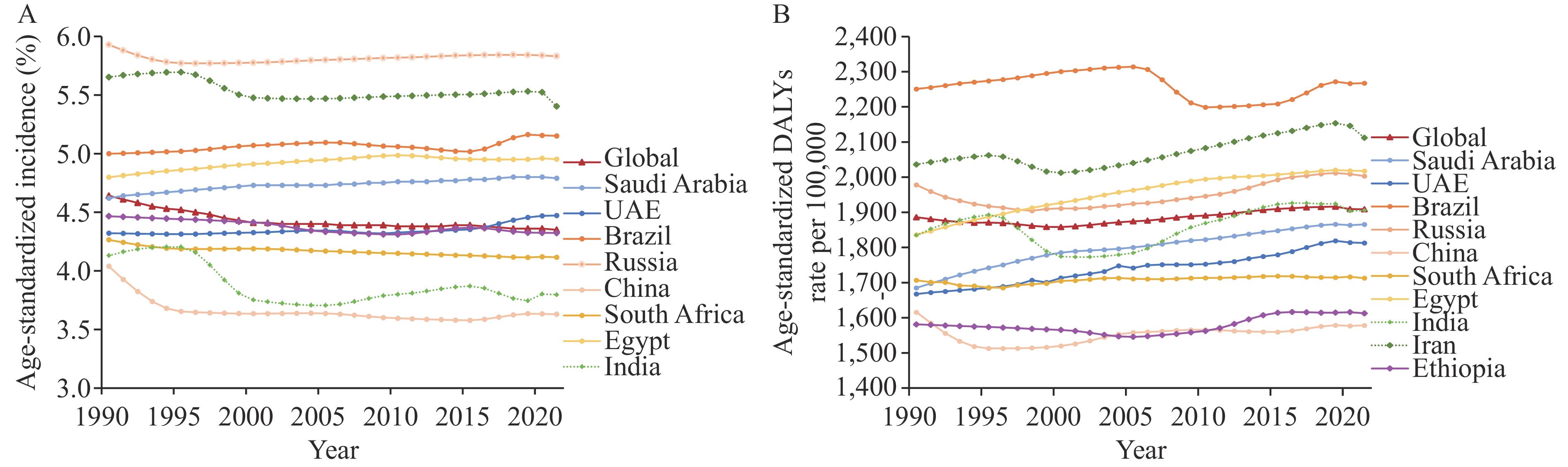
Musculoskeletal (MSK) disorders are escalating in the BRICS+ nations. The BRICS+ countries include five primary members of Brazil, Russia, India, China, and South Africa, and five new members of Saudi Arabia, Egypt, the United Arab Emirates (UAE), Iran, and Ethiopia by January 1st, 2024.
Utilizing the Global Burden of Disease (GBD) 2021 database, the study measured MSK disorders burden through incidence, prevalence, and disability-adjusted life years (DALYs), segmented by location, sex, and disease type. The average annual percentage change (AAPC) from 1990 to 2021 was evaluated to track the burden changes.
In 2021, among BRICS+ nations, Brazil (2,267) and China (1,616) presented the highest and lowest age-standardized DALYs of MSK disorders per 100,000, respectively. Females had higher DALYs than males. The largest decrease and increase in age-standardized DALYs from 1990 to 2021 occurred in China (−2.35%) and Saudi Arabia (10.74%), respectively. Among all MSK disorders in 2021, low back pain (LBP) was the leading cause of the DALYs, while gout was the least contributor in BRICS+ nations. For males, the DALYs due to LBP, rheumatoid arthritis (RA), osteoarthritis (OA), neck pain (NP), and other MSK disorders except gout were lower than those for females. From 1990 to 2021, age-standardized DALYs of MSK disorders exhibited a significant decreasing trend in China [AAPC=−0.34; 95% confidence interval (CI): −0.38, −0.30], no significant change in Brazil and South Africa, and a growth trend in other nations, with the largest increasing trend detected in Saudi Arabia (AAPC=0.33; 95% CI: 0.31, 0.34).
MSK disorders imposed a substantial burden on BRICS+ countries, particularly in Brazil and Iran, with distinct patterns requiring tailored healthcare policies and resource distribution.



 Subscribe for E-mail Alerts
Subscribe for E-mail Alerts CCDC Weekly RSS Feed
CCDC Weekly RSS Feed