2024 Vol. 6, No. 43
China faces a growing burden of chronic obstructive pulmonary disease (COPD). Previous mortality estimations were primarily based on the underlying cause of death. This study analyzed COPD-associated death and its comorbidities using all COPD cases listed on the chain of events on death certificates.
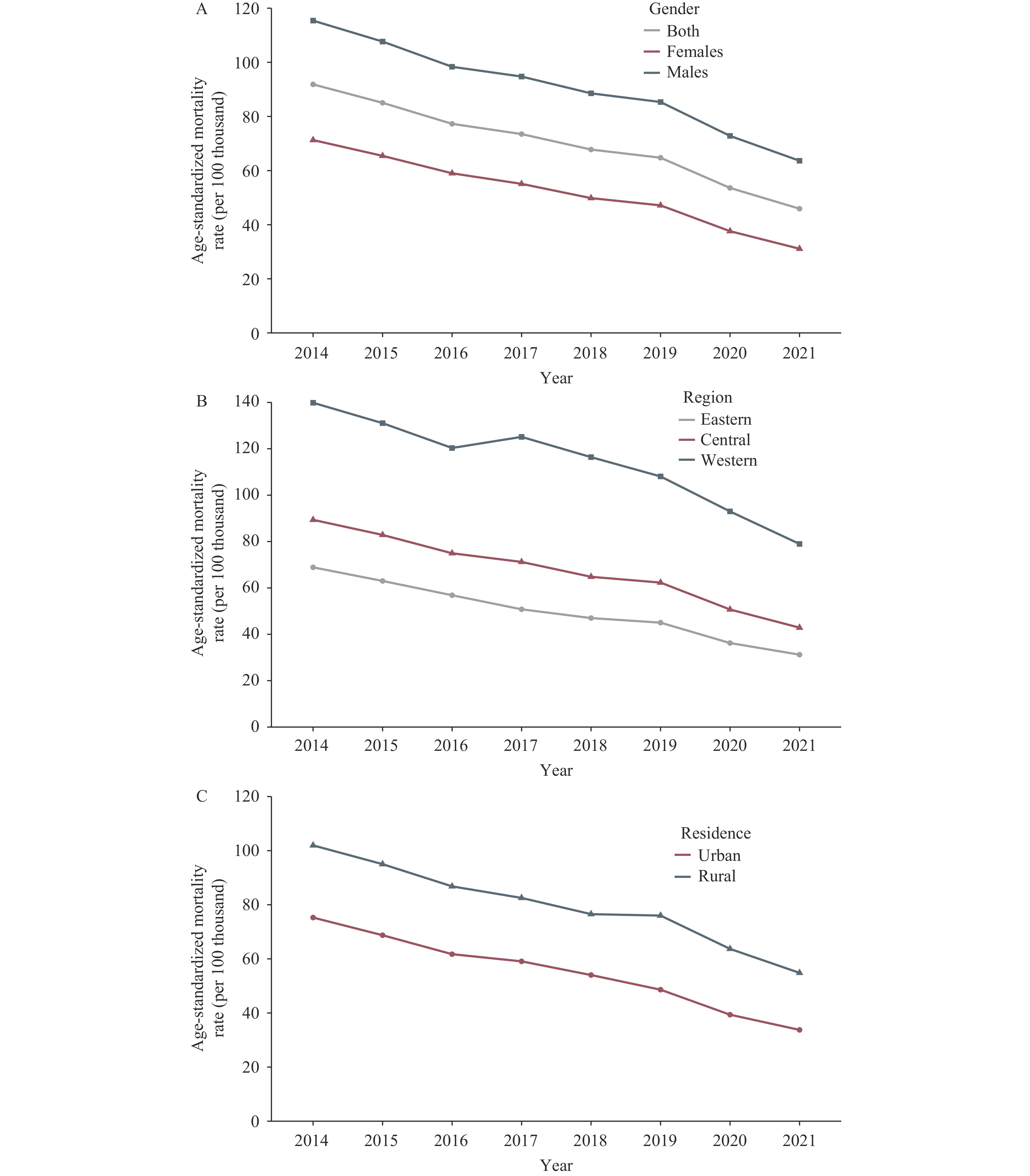
A retrospective analysis of the National Mortality Surveillance System (NMSS) was conducted to estimate COPD-associated mortality from 2014 to 2021. Age-standardized mortality rates (ASMRs) were calculated stratified by sex, region, and residence. Joinpoint regression was used to estimate the average annual percentage change (AAPC) during the study period.
From 2014 to 2021, the ASMR of COPD decreased from 91.85 to 45.90 per 100,000 population. Significant but uneven decreases in COPD mortality were observed across gender [females: AAPC: −11.2%, 95% confidence interval (CI): −11.9 to −10.4%; males: AAPC: −8.0%, 95% CI: −9.2 to −6.8%], regions (eastern: AAPC: −10.7%, 95% CI: −11.5 to −9.9%; central: AAPC: −9.9%, 95% CI: −10.9 to −8.9%; western: AAPC: −7.7%, 95% CI: −10.6 to −4.7%), and residential areas (urban: AAPC: −10.9%, 95% CI: −12.3 to −9.5%; rural: AAPC: −8.3%, 95% CI: −9.1 to −7.4%). Other than COPD, cardiovascular diseases and respiratory conditions were the major underlying causes of death in COPD-associated mortality.
COPD is a significant comorbidity of other disorders in China. Although COPD-associated mortality substantially decreased from 2014 to 2021, the burden remained high in underdeveloped regions.
Solid fuel combustion is a significant source of household air pollution and an important risk factor for chronic obstructive pulmonary disease (COPD). This study presents the rates and change in the use of solid fuels for cooking and heating in China.
Based on data from the Chinese Chronic Obstructive Pulmonary Disease Surveillance, the research estimated the rates and change of solid fuels usage for cooking and heating from 2014–2015 to 2019–2020 and the rate of primary cooking solid fuels usage in 2019–2020, and analyzed the association between solid fuels usage and COPD.
The rates of solid fuels usage for cooking and heating significantly decreased, dropping from 45.3% to 28.0% and from 33.5% to 23.2%, respectively. Usage rates were higher among rural residents, with 47.2% using it for cooking and 37.7% for heating in 2019-2020. The usage of solid fuels for cooking is associated with increased risk of COPD. Among rural residents, combined usage of biomass and coal for cooking (OR=1.29, 95% CI: 1.12, 1.48) and using coal as primary fuel for cooking (OR=1.18, 95% CI: 1.00, 1.38) are associated with higher risk of COPD. The usage of biomass for cooking is associated with an increased risk of COPD in urban residents (OR=1.17, 95% CI: 1.03, 1.32).
The study demonstrates a significant decline in the use of household solid fuels. Nevertheless, high utilization rates persist among individuals in rural settings and those from lower socioeconomic backgrounds. It is of great public health importance to propose targeted fuel substitution measures for various solid fuels in different regions to reduce the risk of COPD.
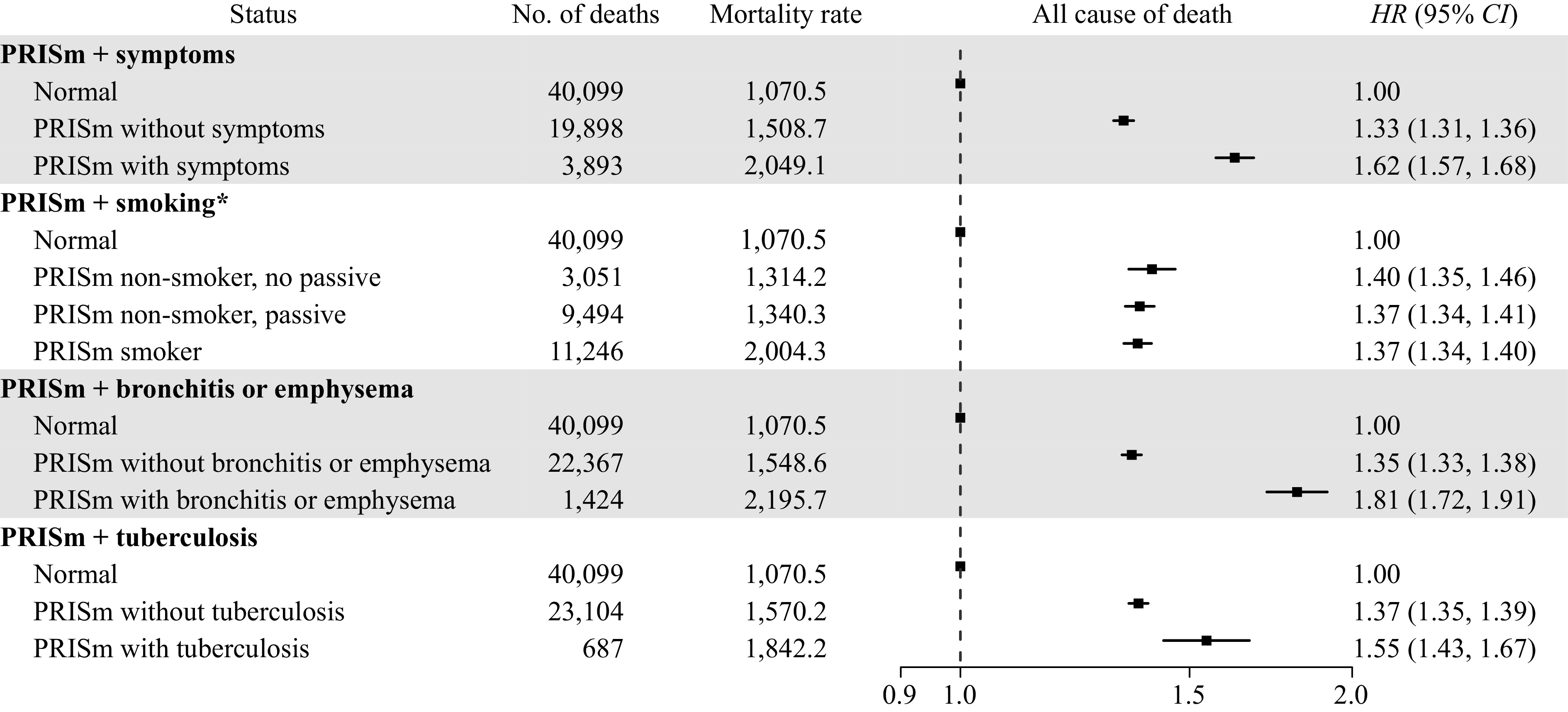
China has the world’s most significant public health and economic burden of chronic respiratory disease. However, the association between preserved ratio impaired spirometry (PRISm) and mortality risk is unknown.
The PRISm group exhibited a 37% higher risk of all-cause mortality than the normal group, and the risks of death from cardiovascular diseases, neoplasms, respiratory diseases, and infectious and parasitic diseases were also increased in PRISm. Moreover, the presence of respiratory symptoms or disease was associated with an increased risk of mortality in PRISm.
It is imperative to enhance public awareness of PRISm and to implement measures to facilitate the regression of PRISm toward normal lung function.
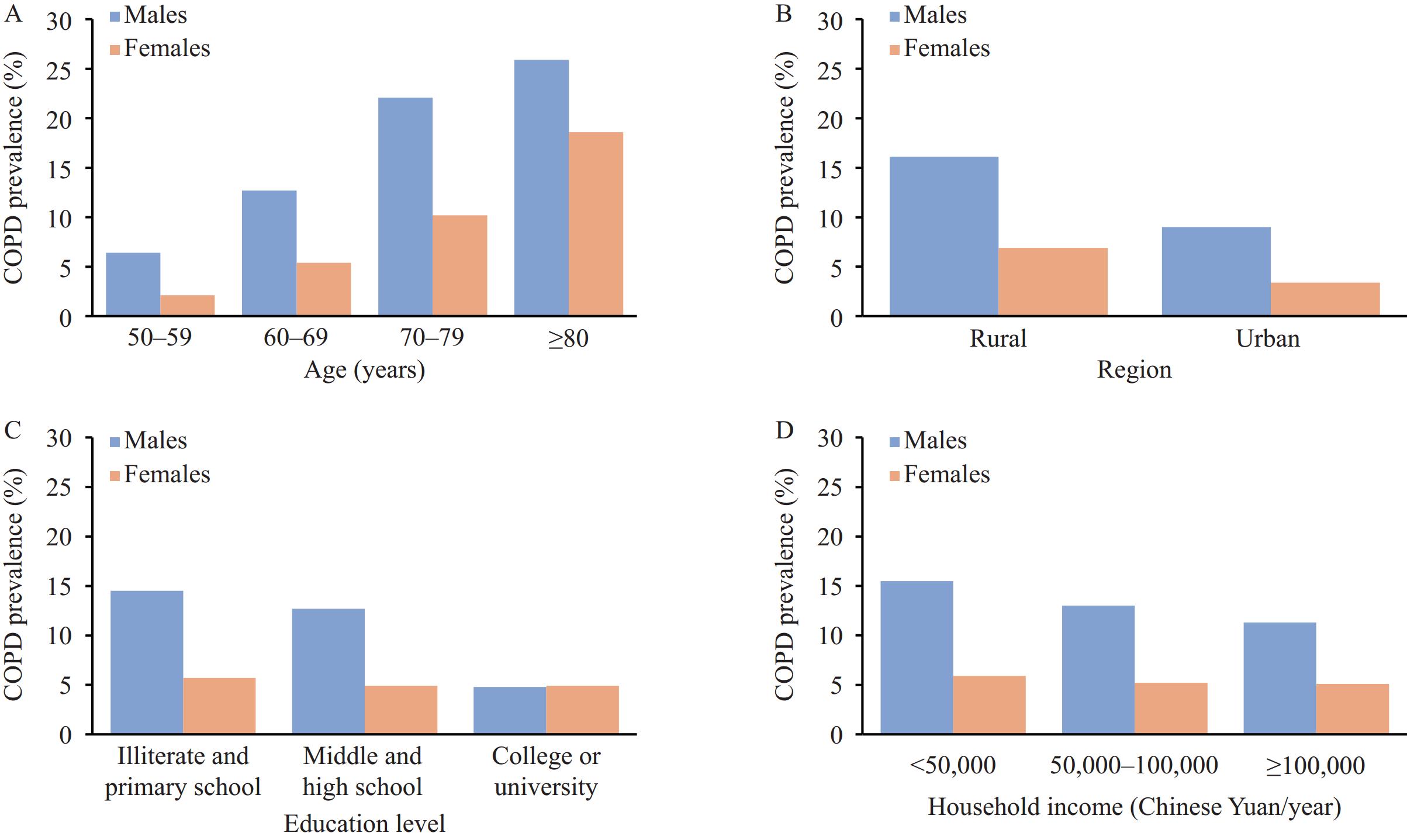
The prevalence of COPD in Chinese individuals aged 50 years and above was obviously higher than that in younger adults, but the risk factors for this age group were unclear.
The prevalence was estimated at 12.8% and 5.7% for males and females over 50 in 2020–2021, with confirmed risk factors of cigarette smoking, a family history of respiratory diseases, respiratory symptoms, and a history of cough or respiratory diseases during childhood.
The findings may help clinicians and the public identify individuals at high risk of COPD and take targeted measures in a timely manner.



 Subscribe for E-mail Alerts
Subscribe for E-mail Alerts CCDC Weekly RSS Feed
CCDC Weekly RSS Feed