-
Chronic obstructive pulmonary disease (COPD) is a leading cause of death globally, resulting in severe economic and public health consequences (1-2). As a heterogeneous condition, COPD is caused primarily by exposure to smoke and air pollution, in combination with genetic and social factors, and often increases the risk of other chronic events (3-4). Older adults are the most susceptible population due to age-related decline in lung function (3). Given the accelerating pace of aging and the large number of active smokers in China (5−6), a substantial COPD burden is unsurprising (7−8).
Considering the growing burden of COPD in China, assessing the latest mortality patterns associated with this disease is crucial for refining management and prevention strategies. Additionally, because COPD frequently coexists with other chronic conditions, understanding its comorbidity patterns is essential. However, most mortality estimates rely on the underlying cause of death, which may not accurately reflect the full scope of COPD-associated mortality. Therefore, this study aimed to investigate the regional distribution and temporal trends of COPD-associated mortality in China between 2014 and 2021. We utilized nationally representative data from the National Mortality Surveillance System (NMSS), including all COPD cases on death certificates listed on the chain of events.
-
This study was a retrospective analysis based on the NMSS, a system initiated in 1978 that gradually expanded nationwide. The NMSS finally covered 605 surveillance points in 31 provincial-level administrative divisions (PLADs), including in-hospital and outside-hospital deaths. It encompasses 323.8 million people, accounting for 24.3% of China’s population (9), with national and provincial representativeness. With a standardized workflow and strict quality control procedures, the NMSS ensures the completeness and accuracy of death records, forming the basis for official mortality statistics. Detailed information on the NMSS is provided elsewhere (9).
COPD-associated mortality was defined as deaths with COPD certified as a cause of death anywhere on the chain of events in parts 1 and 2. COPD was defined using codes J40–J44 from the International Classification of Diseases, 10th edition (ICD-10). In addition to COPD, other major causes of death, including other respiratory events and cardiovascular diseases (CVDs), were included in the analysis.
COPD-associated deaths, stratified by sex, region, and residence, were derived from the NMSS from 2014 to 2021. The proportion of the underlying cause of death in COPD-associated mortality and the contributory cause of death with COPD as the underlying cause of death were calculated. The under-reporting adjustment was applied to estimate COPD-associated mortality (10). The ASMR was calculated using the direct standardization method using the 2020 China census as the reference population (10). The temporal trend of COPD-associated mortality from 2014 to 2021 was described by the AAPC with a 95% confidence interval (CI), estimated by a joinpoint regression model (Joinpoint Regression Program, version 5.0.2; National Cancer Institute, Rockville, MD, USA). Statistical analyses were performed using SAS version 9.4 (SAS Institute; Cary, NC, USA) and R (version 4.1.3; R Foundation for Statistical Computing, Vienna, Austria). All tests were two-sided, and P<0.05 was considered statistically significant.
-
From 2014 to 2021, there was a general downward trend in COPD-related mortality (Table 1 and Figure 1). The absolute number of deaths decreased from 180,330 to 149,612, and the ASMR associated with COPD decreased from 91.85 to 45.90 per 100,000 population, with an AAPC of −9.4% (95% CI: −10.3 to −8.4%). Males had higher COPD-associated mortality and a milder decrease than females, corresponding to AAPCs of −8.0% (95% CI: −9.2 to −6.8%) and −11.2% (95% CI: −11.9 to −10.4%), respectively. The Eastern region, with the lowest COPD burden, showed a sharp decline during our study period (AAPC: −10.7%, 95% CI: −11.5 to −9.9%), followed by the Central (AAPC: −9.9%, 95% CI: −10.9 to −8.9%) and Western (AAPC: −7.7%, 95% CI: −10.6 to −4.7%) regions. COPD-associated mortality was higher in rural areas (ASMR: 54.83 per 100,000) than in urban areas (ASMR: 33.75 per 100,000). However, compared to rural areas (AAPC: −8.3%, 95% CI: −9.1 to −7.4%), urban areas presented a more substantial drop (AAPC: −10.9%, 95% CI: −12.3 to −9.5%).
Category 2014 2021 AAPC of age-standardized mortality rate from 2014 to 2021 (95% CI) Number Crude mortality rate (1/100,000) Age-standardized mortality rate (1/100,000) Number Crude mortality rate (1/100,000) Age-standardized mortality rate (1/100,000) Total 180,330 69.68 91.85 149,612 47.09 45.90 −9.4% (−10.3, −8.4%)* Sex Females 75,964 60.16 71.27 56,518 36.34 31.09 −11.2% (−11.9, −10.4%)* Males 104,366 78.76 115.41 93,094 57.41 63.62 −8% (−9.2, −6.8%)* Residence Urban 55,372 53.77 75.27 46,576 32.84 33.75 −10.9% (−12.3, −9.5%)* Rural 124,958 80.20 101.95 103,036 58.58 54.83 −8.3% (−9.1, −7.4%)* Region Eastern 63,912 56.25 68.87 48,430 32.84 31.21 −10.7% (−11.5, −9.9%)* Central 50,877 65.13 89.36 40,680 45.22 42.86 −9.9% (−10.9, −8.9%)* Western 65,541 97.75 139.84 60,502 75.37 78.96 −7.7% (−10.6, −4.7%)* Abbreviation: COPD=Chronic obstructive pulmonary disease; AAPC=average annual percentage change; CI=confidence interval.
* P<0.001.Table 1. Number of deaths, crude and age-standardized mortality rates associated with COPD, and temporal trends from 2014 to 2021.
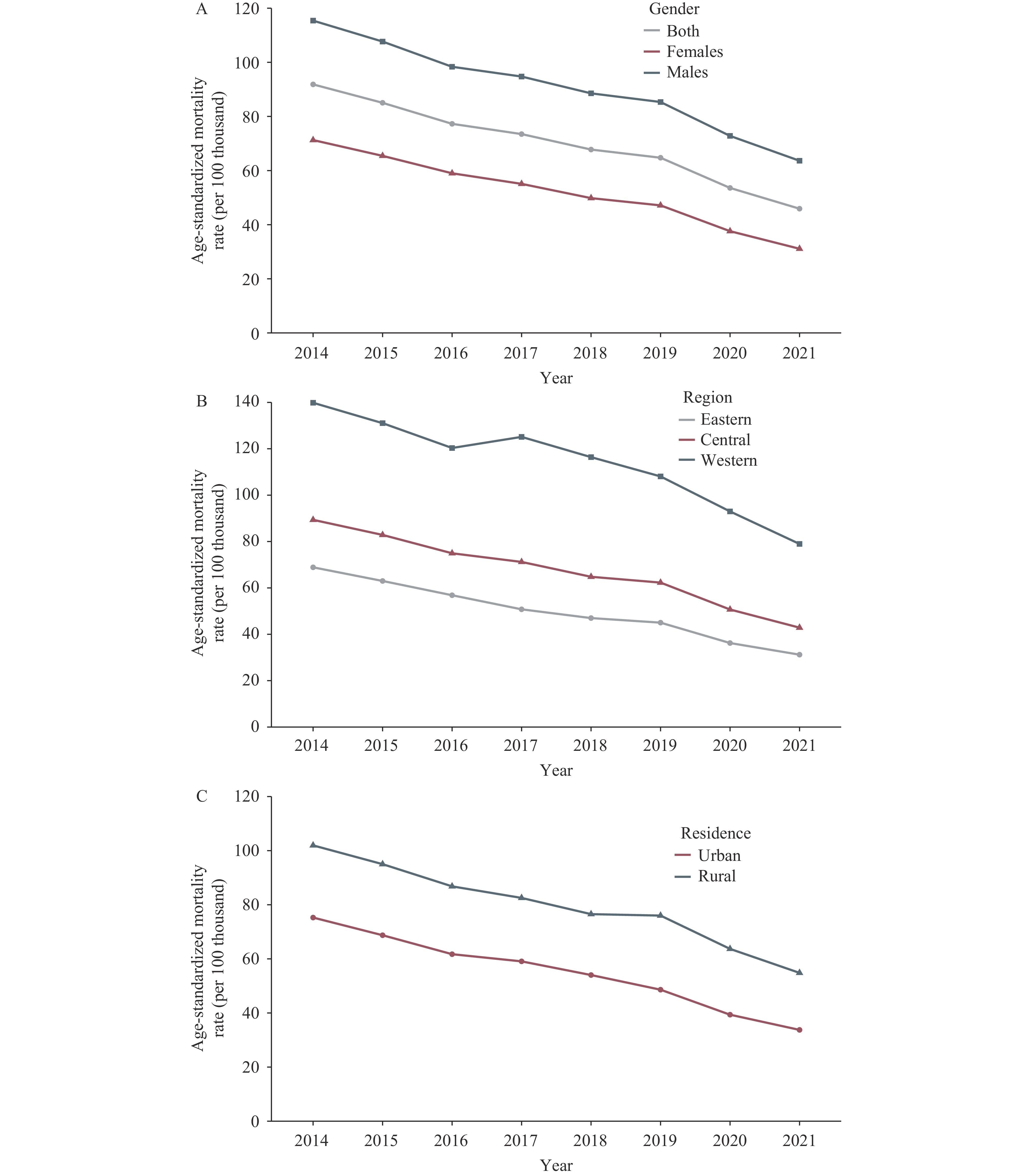 Figure 1.
Figure 1.Temporal trend in age-standardized mortality rate related to COPD by (A) sex, (B) region, and (C) residence in China from 2014 to 2021.
Abbreviation: COPD=chronic obstructive pulmonary disease.COPD was the most common underlying cause of death across years, accounting for 92.87% of all deaths (Figure 2A). Aside from COPD, lung cancer, cardiovascular disease, and other chronic respiratory diseases were the major underlying causes of death. Malignant neoplasm of the trachea, bronchus, and lung ranked second with a proportion of 2.81%, followed by pulmonary heart disease and diseases of pulmonary circulation (1.00%) and ischemic heart disease (0.69%). Cerebrovascular diseases and asthma ranked seventh and eighth, corresponding to 0.41% and 0.33% of COPD-associated deaths, respectively.
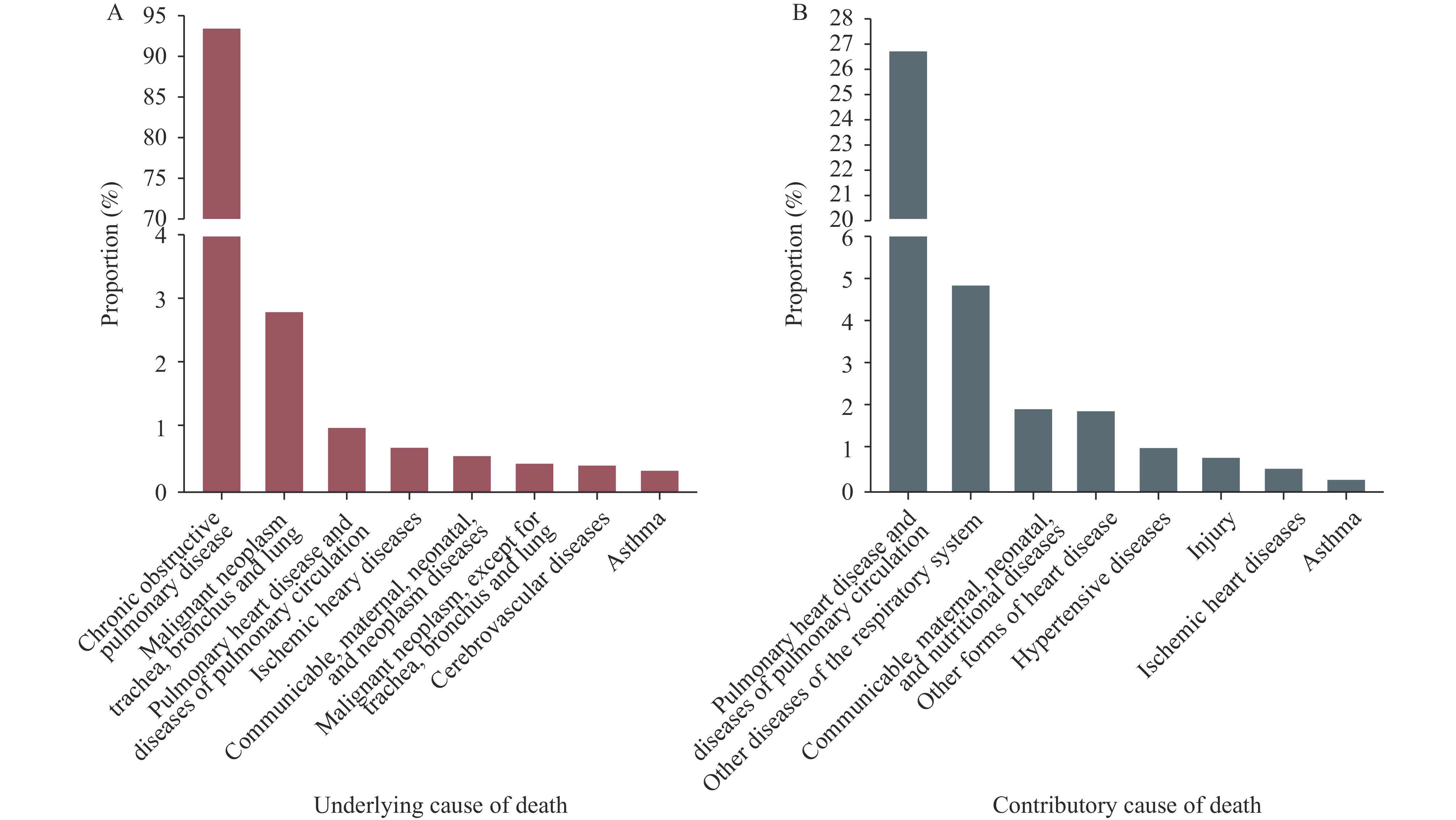 Figure 2.
Figure 2.Major underlying and contributing causes of death among decedents with COPD in China during 2014–2021. (A) The major underlying causes of death in all deaths related to COPD. (B) The common contributing causes of death in decedents with COPD as the underlying cause of death.
Abbreviation: COPD=Chronic obstructive pulmonary disease.Among all deaths with COPD as the underlying cause of death, the leading contributory cause of death was pulmonary heart disease and diseases of pulmonary circulation, with 0.9 million deaths (26.79% of all COPD deaths) (Figure 2B). Other diseases of the respiratory system ranked second, with a proportion of 4.87%. Other forms of heart disease (1.9%), hypertensive diseases (1.03%), and ischemic heart disease (0.54%) ranked fourth, fifth, and seventh, respectively. Asthma, with a proportion of 0.28%, was the eighth most common contributory cause of death in decedents whose underlying cause was COPD.
-
Aside from COPD, cardiovascular diseases and respiratory conditions were the major underlying and leading contributory causes of COPD-associated mortality. From 2014 to 2021, significant downward trends in COPD-associated mortality were observed across genders, regions, and residential areas. Regions and residential areas with advanced economies generally had lower ASMRs and steeper declines in ASMR.
Consistent with other major studies, COPD was found to coexist with a broad set of diseases (comorbidities), with CVDs and respiratory events being the two leading ones. Comorbidities were common at any severity of COPD, and about 97.7% of COPD patients experienced at least one comorbid disease, while 53.5% had four or more (11). Some of these comorbidities originated independently from COPD, while others may be causally related to some extent by either sharing common risk factors or mutually exacerbating each other (12). For example, COPD and lung cancer were confirmed to share common origins, with tobacco smoking, second-hand smoke, household and outdoor air pollution, and occupational exposures as their common risk factors (2–3,12). Additionally, according to the Global Strategy for Prevention, Diagnosis, and Management of COPD: 2024 Report, COPD patients with no preexisting CVDs generally had a 25% higher risk of adverse cardiac events (12). However, even though systemic inflammation, the major characteristic of COPD, was documented as one of the potential determinants linking COPD to its main comorbidities, the detailed interaction mechanism is still under-researched (2,13).
Complex health conditions, unclear mechanisms, and comorbidities pose significant challenges, particularly in less developed areas. Uneven socioeconomic development substantially contributes to disparities in COPD management and outcomes (1,3). Limited healthcare resources, reduced social support, inadequate health awareness, and greater exposure to risk factors like biomass fuels and coal are strongly associated with underdeveloped economies. Notably, even in developed areas, individuals with low socioeconomic status may lack access to healthcare services (14). The WHO reports that approximately 90% of COPD deaths before the age of 70 occur in low- and middle-income countries (4). Yin et al. identified similar disparities, observing higher COPD ASMRs in provinces with low socioeconomic indices, typically located in western China (1). Moreover, rural areas in China (15), as well as the United States (3), experience higher COPD-attributable ASMRs compared to urban areas.
As a heterogeneous condition, COPD requires personalized pharmacological treatment with thorough consideration of comorbidities, symptom severity, exacerbation risk, and side effects (12). The emergence of advanced imaging tools, such as computed tomography (CT) and magnetic resonance imaging (MRI), has made in vivo studies of structure-function associations possible and formed the basis for individualized COPD management (3). Additionally, with the promotion of clean energy since the 1990s, solid fuel has been gradually replaced by electricity and natural gas in China, attenuating exposure to household air pollution (1). Smoking cessation, vaccination, and protection against occupational exposures were highly encouraged, some even required by specific rules or regulations. These measures likely mitigated COPD outcomes and contributed to a general decrease in ASMR over time. However, regions did not benefit evenly, particularly less developed areas. A national cross-sectional survey of rural areas in seven PLADs in China showed that the diagnosis rate of COPD was only 30% (15). Moreover, only 7.9% of COPD patients at stage II or above received pharmacological treatment, and 0.3% used regular inhalers and oxygen therapy (15). According to the survey, the penetration rate of clean energy remained low, and the smoking cessation rate among COPD patients was 25.5%, indicating low disease awareness and poor self-management (15). Therefore, despite a downward trend, ASMR has experienced a relatively mild decline in underdeveloped regions.
To prevent and manage COPD, policymakers should implement stricter actions, particularly in western regions and rural areas. Given that COPD frequently presents with comorbidities and often acts as a severe comorbidity for other disorders, clinicians and patients should pay special attention to potential or existing comorbidities. Individuals diagnosed with CVDs and other respiratory events, such as lung cancer, should be cautious about the development of COPD. Reducing COPD-associated mortality requires controlling common risk factors for COPD and other major adverse health events. For example, avoiding direct or indirect exposure to smoking is a top priority. Therefore, legislative smoking bans and counseling are strongly encouraged nationwide. Additionally, due to the disparities in COPD management and outcomes, more detailed health guidance is needed, especially in underdeveloped regions. Personalized and multidimensional treatment should also be more accessible in the future to mitigate the burden of COPD.
This study estimated recent COPD-associated mortality using data from the NMSS, the most comprehensive source of mortality information in China. This approach provides the most accurate description of the burden and temporal trends in COPD-associated mortality from 2014 to 2021. Additionally, this study included COPD cases based on the chain of events on death certificates rather than solely considering COPD as the underlying cause, capturing comorbidities among decedents with COPD.
However, this study has some inherent limitations. First, death certificates only list diseases, injuries, and complications directly causing death and thus do not provide a complete picture of decedents' pre-existing conditions. Our analysis may not capture individuals with COPD that did not directly result in death. Additionally, underreporting in western regions and low diagnosis rates in rural areas may underestimate COPD-associated mortality. Finally, because data were extracted from death certificates, which do not document lifetime risk factor exposure, our research did not include a risk factor analysis, which is highly warranted in future research.
In conclusion, COPD is a complex, multicomponent condition frequently accompanied by other diseases. Its comorbidities are crucial determinants of outcomes, and COPD itself is an important comorbidity of other disorders. In China, even though COPD-associated mortality presented a substantial decreasing trend from 2014 to 2021, the COPD burden remained high in underdeveloped regions. This indicates that COPD is still a severe public health issue in China, and healthcare resources may not be evenly distributed. Therefore, public health officials should prioritize a region-specific strategy for the management and prevention of COPD to alleviate the burden of disease.
HTML
| Citation: |



 Download:
Download:




