2023 Vol. 5, No. 36
The primary causes of early miscarriage and stillbirth are chromosomal abnormalities (CAs) whose prevalence has been observed to increase in recent years.
According to data received from a hospital-based birth-defect surveillance system in the Haidian District, Beijing, there was a significant increase in the prevalence of CAs along with most subtypes from 2013 to 2022. This noted increase in the reported prevalence is potentially attributable to factors such as a rise in maternal age, alongside the enhanced detection efficacy resulting from the utilization of noninvasive prenatal testing.
The escalating prevalence of sex CAs and other previously rare CAs pose novel challenges for genetic counseling and healthcare practitioners. These professionals are tasked with the accurate evaluation and interpretation of detection data, which must then be conveyed appropriately to patients. Furthermore, it is imperative to intensify health education efforts to assist women in making informed treatment decisions, considering the diverse prognoses associated with different CAs.
The Shanxi Province, located in northern China, holds the highest prevalence of birth defects (BDs) across the country. Following the implementation of a nationwide folic acid supplementation program in 2009, a significant reduction of 53.89% in the prevalence of neural tube defects (NTDs) was observed in Shanxi from 2012 to 2017. However, despite this decrease, the prevalence rate for congenital heart defects (CHDs) in 2017 was over four times that of the 2012 rate. Since 2014, CHDs have emerged as the most predominant BD in Shanxi.
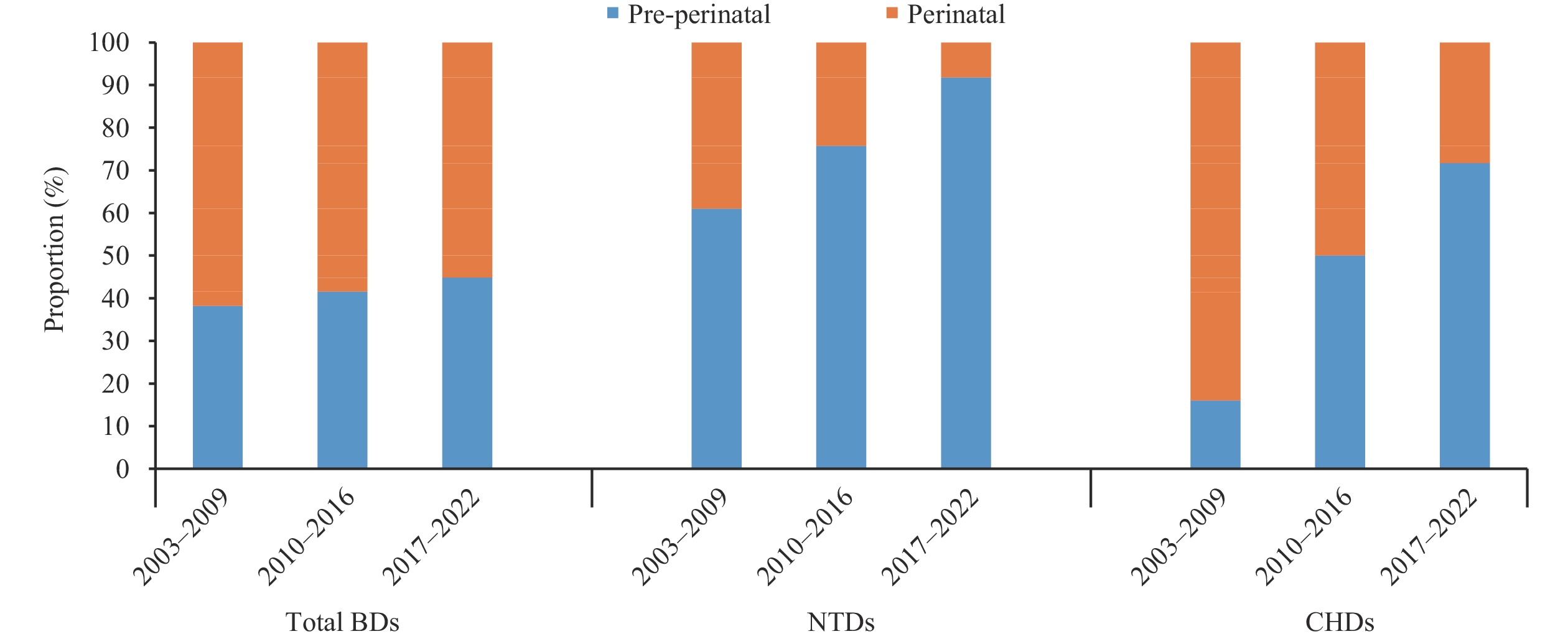
The present study has identified a marked reduction in the prevalence of both total BDs and NTDs in five counties within Shanxi over the past two decades. As of 2017–2022, NTDs continue to be the most prevalent BDs recorded in this region. Contrarily, there has been a noteworthy increase in the prevalence of CHDs, ranking them among the top five most common BDs in the region between 2017 and 2022, though their rate remains below the national average. Additionally, the proportion of external anomalies remains high. Nevertheless, due to constrained access to primary healthcare services and diagnostic facilities, the early detection rate for internal anomalies, particularly CHDs, may be underestimated in the region.
The results of this study underscore the necessity for augmented efforts in promoting folic acid supplementation as a preventive measure for NTDs. Moreover, improvements in the distribution of medical resources within this region are recommended, particularly the introduction and enforcement of local training programs aimed at enhancing CHD screening and diagnostic processes in these respective counties.
Robust evidence indicates that supplementing with folic acid periconceptionally may decrease the risk of neural tube defects (NTDs) in fetuses.
Over half of the mothers in both the NTD case group and the control group utilized folic acid supplements during the periconceptional period, showing no notable variations between the two groups. However, there was a significantly higher percentage of mothers with NTD cases who exhibited poor compliance in folic acid use compared to control mothers. A significantly lowered compliance with folic acid intake was observed among women facing unintended pregnancies and those with lower education levels.
Universal education regarding folic acid action for women of childbearing age should be strengthened to improve compliance with folic acid supplementation in the periconceptional period and further reduce the prevalence of NTDs.
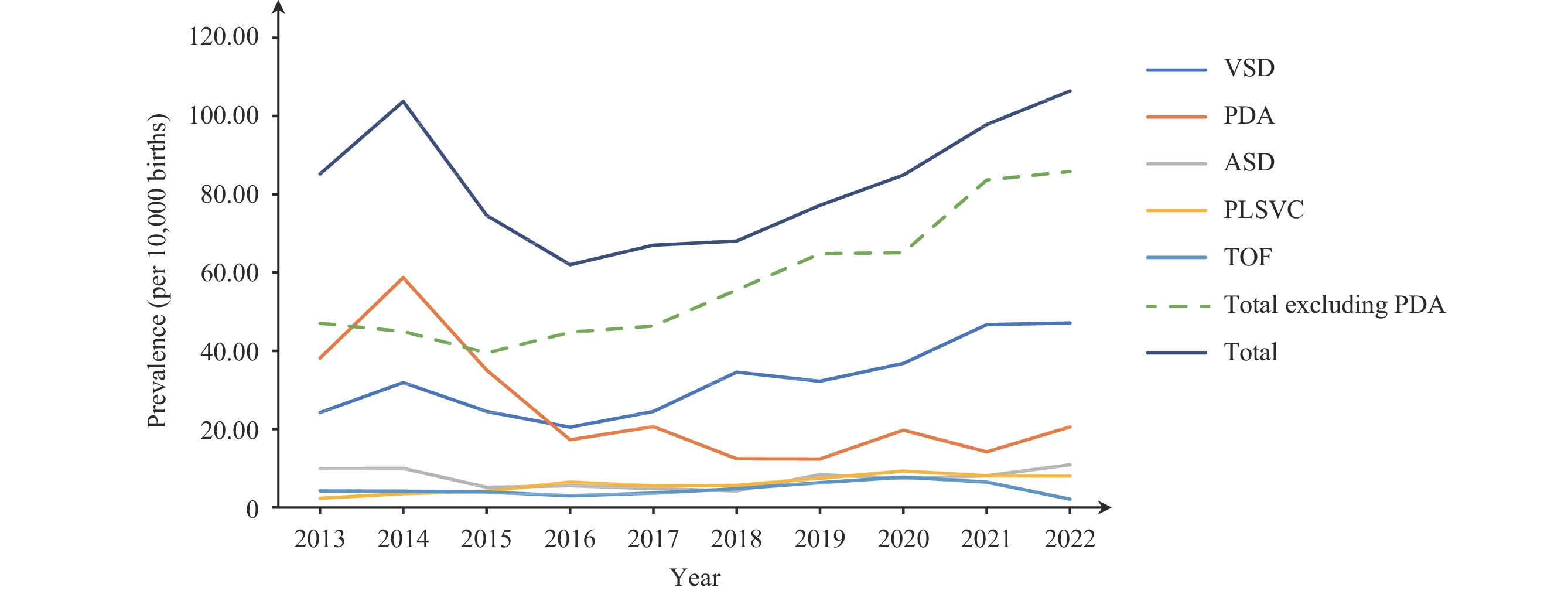
Congenital heart defects (CHDs) represent the most prevalent birth defects in China, exhibiting significant mortality and morbidity rates. Recent years have witnessed a steady increase in the occurrence of CHDs, highlighting a crucial need for rigorous research focus.
The cumulative birth prevalence of CHDs in Haidian District from 2013 to 2022 was 80.77 per 10,000 births, reflective of an upward trend primarily influenced by the diagnosis of minor, non-critical congenital defects (non-CCHDs). This increase can be attributed to advancements in diagnostic methodologies. Despite the progress in detection, the survival rate for CHDs did not correspondingly improve.
Policies need to be formulated to promote the graded management of CHDs. There should be timely updates to the diagnostic criteria to align with advancements in diagnostic techniques. Moreover, in instances where therapeutic abortion is not required, the provision of appropriate medical consultation post-diagnosis should be enhanced.



 Subscribe for E-mail Alerts
Subscribe for E-mail Alerts CCDC Weekly RSS Feed
CCDC Weekly RSS Feed