2024 Vol. 6, No. 41
The global incidence of dengue fever has increased significantly over the past two decades, and China faces a significant upward trend in dengue control challenges.
Data were obtained from China’s NNDRS from 2005 to 2023. Joinpoint regression software was used to analyze temporal trends, while SaTScan software was used to analyze spatial, seasonal, and spatiotemporal distributions. ArcGIS software was used to visualize clusters.
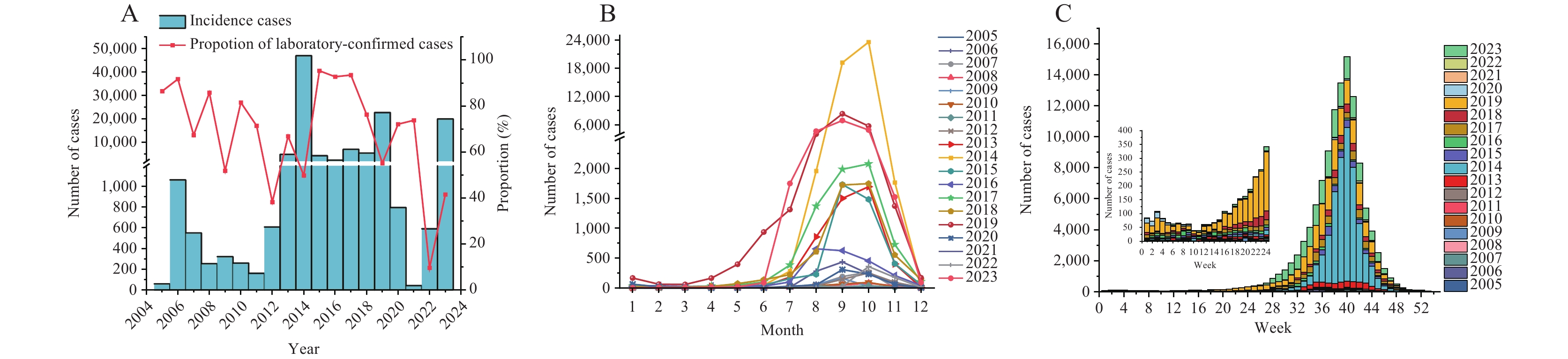
A total of 117,892 dengue cases were reported from 2005 to 2023, with significant fluctuation in annual reported cases. Dengue was not endemic in China. Autochthonous outbreaks most likely occurred in the southwestern, southeastern coastal, and inland areas of China. These outbreaks have occurred between June and November, generally peaking in September or October, around epidemiological week (EW) 40.
Dengue challenges in China are increasing. Timely case monitoring, proactive control interventions, and staff mobilization should be implemented before June to ensure a timely response to autochthonous outbreaks.
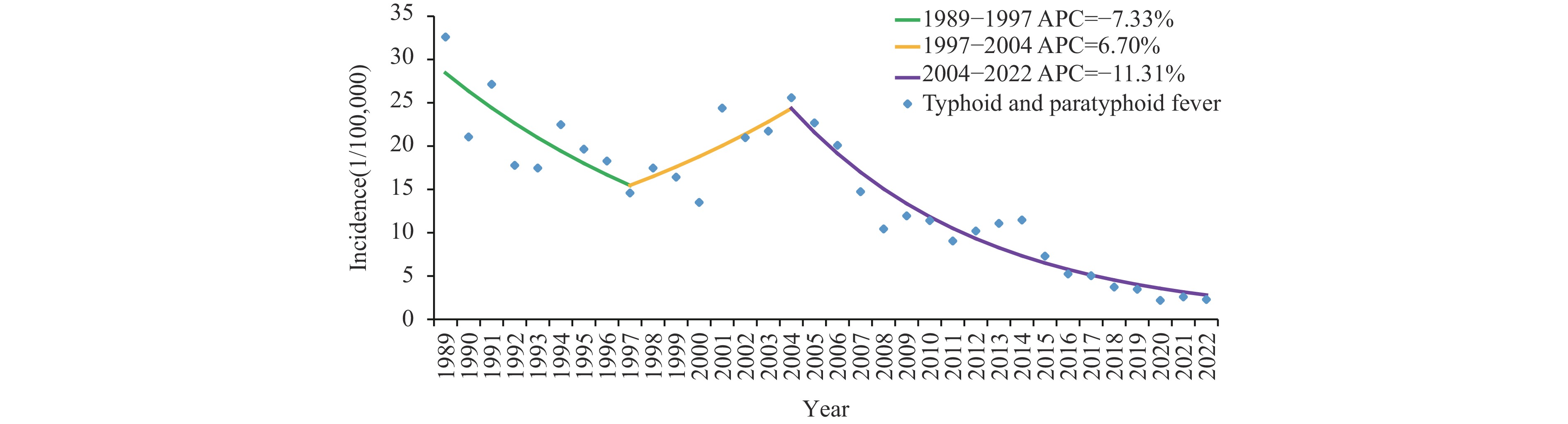
This study explored the incidence trends and spatial clustering of typhoid and paratyphoid fever (TPF) in Yunnan Province to provide scientific evidence for developing and improving prevention and control strategies.
Temporal trends were investigated by calculating the annual percent change (APC) and average annual percent change (AAPC), along with their 95% confidence intervals (CIs). The spatial clustering of TPF across Yunnan Province was examined using global Moran’s I and local indicators of spatial association (LISA) statistics.
A total of 206,066 TPF cases were reported in Yunnan Province from 1989 to 2022, with an average annual incidence of 13.98 per 100,000 population and a case fatality rate of 2.5 per 1,000. The greatest number of cases was reported during July and August. The 25–34-year age group had the highest incidence, and farmers were prominently represented. TPF incidence in Yunnan Province showed a significant decrease and spatial clustering. From 2005 to 2022, 13 county-level cities/counties/municipal districts in 5 prefectures (cities) in Yunnan Province were identified as statistically significant H-H spatial clusters of TPF incidence. A total of 24 TPF outbreaks were reported in Yunnan Province from 2005 to 2022.
The incidence of TPF in Yunnan Province showed a significant decrease and spatial clustering. Control strategies should focus on high-incidence areas, seasons, and populations to reduce the incidence of TPF.
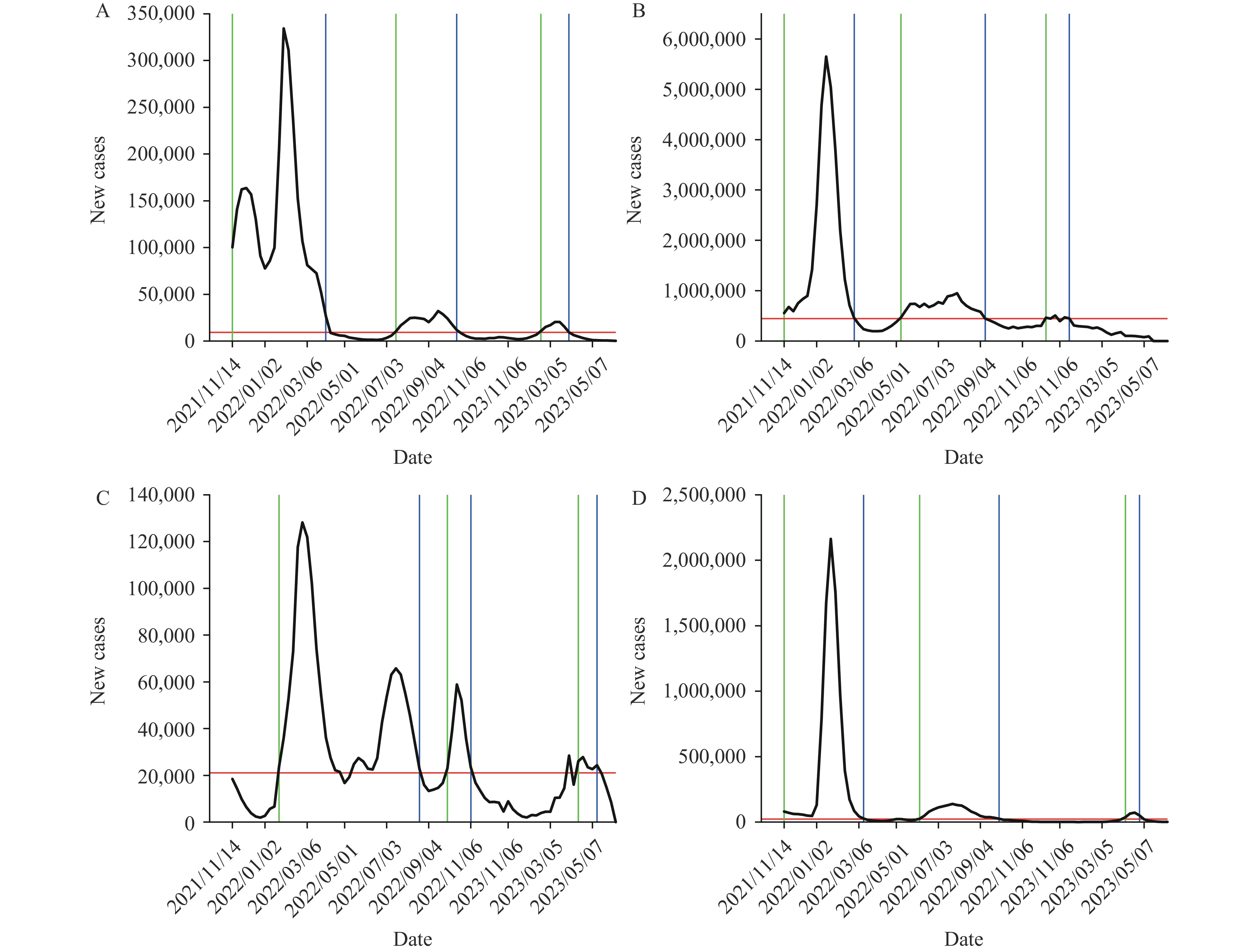
Analyzing the characteristics of epidemic development after the emergence of the severe acute respiratory syndrome virus 2 Omicron variants with its subvariants and the impact of income level inequalities on the coronavirus disease 2019 (COVID-19) case-fatality ratio helps to better understand the spread of novel coronavirus infections.
The median time interval between the first and second waves of Omicron sub-variants was 70 days (interquartile spacing: 43.75–91), and between the second and third waves was 87.5 days (interquartile spacing: 49–119), which obeyed a lognormal distribution. The case-fatality ratio of the first wave was significantly higher than that of the second and third waves. During the initial epidemic period, there was no significant geographic differences in the case-fatality ratio of the first wave, while the case-fatality ratio in countries with high income levels was significantly lower than in countries with other income levels.
We still need to pay attention to the COVID-19 pandemic, as inequalities in income levels have an impact on the case-fatality ratio during the early stages of Omicron epidemics. In most countries, strains of the virus are likely to move from low to high population prevalence after 2–4 months.
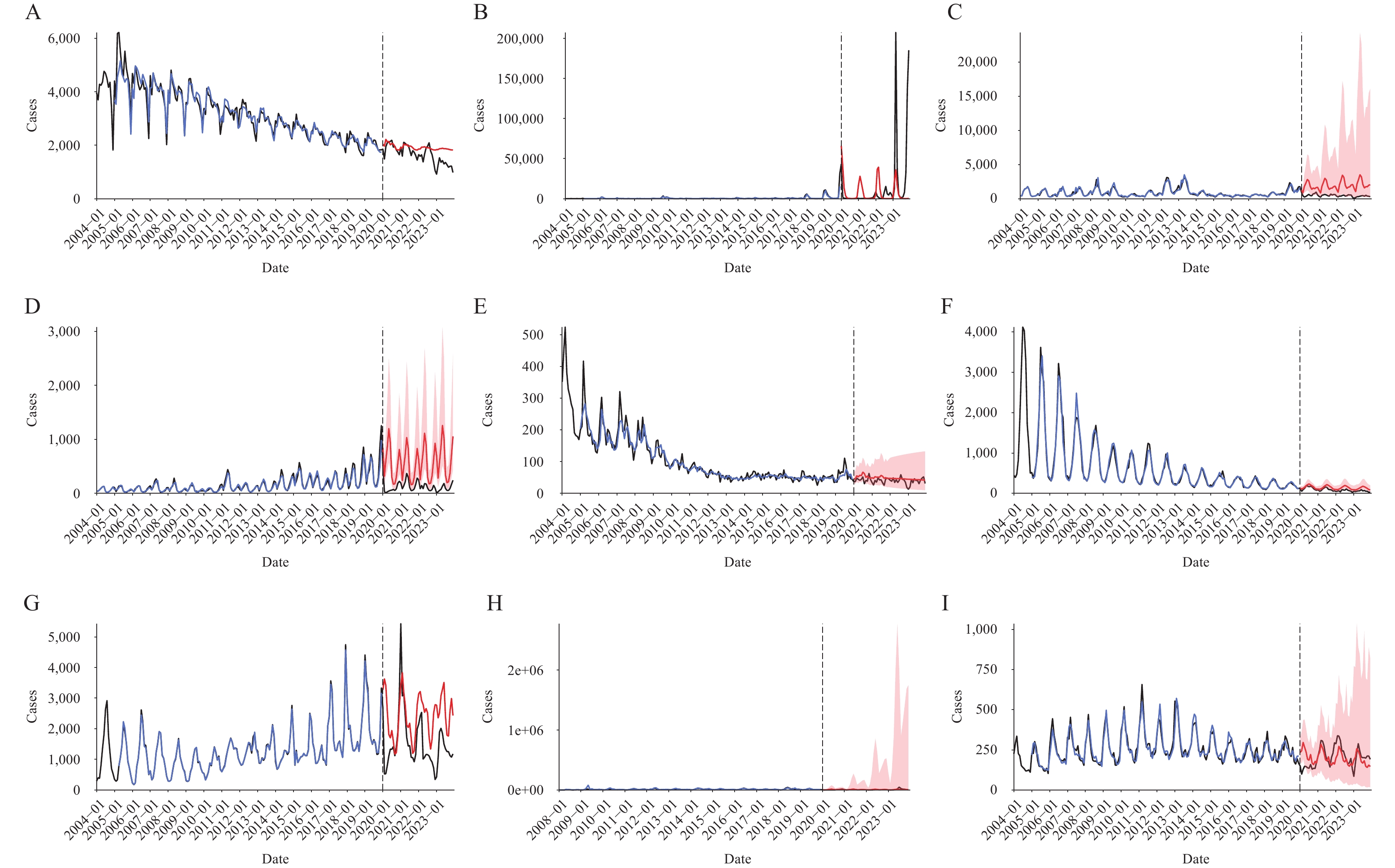
Many measures implemented to control the coronavirus disease 2019 (COVID-19) pandemic have reshaped the epidemic patterns of other infectious diseases. This study estimated the impact of the COVID-19 pandemic on respiratory and intestinal infectious diseases and potential changes following reopening.
The optimal intervention and counterfactual models were selected from the seasonal autoregressive integrated moving average (SARIMA), neural network autoregression (NNAR), and hybrid models based on the minimum mean absolute percentage error (MAPE) in the test set. The relative change rate between the actual notification rate and that predicted by the optimal model was calculated for the entire COVID-19 epidemic prevention period and the “reopening” period.
Compared with the predicted notification rate based on the counterfactual model, the total relative change rates for the 9 infectious diseases were −44.24%, respiratory infections (−55.41%), and intestinal infections (−26.59%) during 2020–2022. Compared with the predicted notification rate based on the intervention model, the total relative change rates were +247.98%, respiratory infections (+389.59%), and intestinal infections (+50.46%) in 2023. Among them, the relative increases in influenza (+499.98%) and hand-foot-mouth disease (HFMD) (+70.97%) were significant.
Measures taken in Jiangsu Province in response to COVID-19 effectively constrained the spread of respiratory and intestinal infectious diseases. Influenza and HFMD rebounded significantly after the lifting of COVID-19 intervention restrictions.
High-quality infectious disease surveillance systems are foundational to infectious disease prevention and control. Current major infectious disease surveillance systems globally can be categorized as either indicator-based, which are more specific, or event-based, which are more timely. Modern surveillance systems commonly utilize multi-source data, strengthened information sharing, advanced technology, and improved early warning accuracy and sensitivity. International experience may provide valuable insights for China. China’s existing infectious disease surveillance systems require urgent enhancements to monitor emerging infectious diseases and improve the integration and learning capabilities of early warning models. Methods such as establishing multi-stage surveillance systems, promoting cross-sectoral and cross-provincial data sharing, applying advanced technologies like artificial intelligence, and cultivating professional talent should be adopted to enhance the development of intelligent and multipoint-triggered infectious disease surveillance systems in China.



 Subscribe for E-mail Alerts
Subscribe for E-mail Alerts CCDC Weekly RSS Feed
CCDC Weekly RSS Feed