-
Seasonal influenza activity declines globally during the coronavirus disease 2019 (COVID-19) pandemic (1-4). For instance, in China, influenza activity, as measured by percentage of submitted specimens testing positive, dropped from 11.8% to 2.0% in 2020–2021 influenza season, compared to the past 5 years (5). The long-period of low-exposure to influenza viruses adds great uncertainty on preparedness for the incoming 2021–2022 influenza season. Influenza vaccination is one of the most effective measures in seasonal influenza prevention and control, but with only a few influenza viruses circulating, it could be difficult to determine the targeted strains for vaccination.
In this context, it is of primary importance to identify alternative mitigation measures for the incoming 2021–2022 influenza season, the first season after long periods of virtually no influenza outbreaks worldwide. Using data from China, the United Kingdom, and the United States, we forecasted the influenza activity in the incoming 2021–2022 influenza season under hypothetical scenarios without non-pharmaceutical interventions (NPIs) and with different assumptions on mask-wearing and mobility levels.
-
Our approach relied on the long-term surveillance of influenza activity, measured as weekly percent positivity, long-term mobility changes, the widespread implementation of mobility mitigations and mask-wearing interventions during the COVID-19 period. We noted that the change of international mobility during the COVID-19 period could capture international travel mitigation; the change of domestic mobility patterns during the COVID-19 period closely coincided with mobility related to NPIs and may have reflected several highly correlated mobility related NPIs including domestic movement restriction and physical distancing.
The virological surveillance data in 2011–2021 were obtained from the corresponding government surveillance systems: National Influenza Surveillance Network in China, Respiratory DataMart System in Public Health England, and the United States (US) CDC.The National Influenza Surveillance Network system monitors influenza viruses circulating in China and consists of 554 sentinel hospitals and 407 network laboratories located in over 300 cities in mainland China. The Respiratory DataMart System serves for systematically monitoring influenza and other respiratory viruses circulating in England, with weekly viral test results reported from 14 laboratories representing all nine regions of England. Surveillance of influenza virus in the U.S. is monitored through the U.S. influenza surveillance system and collated by CDC and over 400 public health and clinical laboratories located throughout all 50 states, Puerto Rico, Guam, and the District of Columbia.We considered Northern China and Southern China separately, due to the sharp difference in the patterns of seasonal influenza. For the United Kingdom, since only virological data in England were collected, we considered England only.
International mobility was measured by inbound travel. Inbound travel in 2011–2021 in Northern China and Southern China was represented by the monthly inbound travel in Shanghai released by the Shanghai Bureau of Statistics. Inbound travel data in England and the US were collected from the Department for Transport and US Department of Transportation, respectively. We estimated the weekly international mobility using the moving average within the past 2–4 weeks to account for the delay between mobility changes and laboratory testing and reporting. The domestic mobility was estimated by relying on human mobility data and public transportation statistics. Weekly domestic mobility in Northern China and Southern China in 2019–2021 was estimated by aggregating the daily relative inflow data collected from Gaode Map API; the inflow data in 2019–2020 were further projected into the year 2011–2018. Weekly domestic mobility in England was estimated from monthly released domestic transportation data from Office for National Statistics in the United Kingdom using the same moving average method as above; in the US, it was estimated using the monthly domestic transportation data from US Department of Transportation.
The mask-wearing intervention in China was imposed starting from Week 4 of 2020 until Week 28 of 2021; in England, the mask regulation was in place from Week 30 of 2020 until Week 28 of 2021, according to the Health Protection Regulations 2020. For these countries, we denoted the mask-wearing index with 1 during the implementation period and 0 otherwise. Since the US state governments did not simultaneously comply with the order imposed by US CDC, we estimate the degree of mask-wearing indexes in the US as a proportion of the number of states that imposed the mask-wearing order during the period of US CDC mask-wearing recommendation (i.e., Week 14 of 2020 until the last week of the study, which was Week 28 of 2021). Theses indexes were further adjusted with COVID-19 vaccination coverage, the percentage of daily administered doses in the total population, to estimate the weekly mask-wearing interventions.
To forecast influenza activity under different NPIs, we explored a self-correcting regularized multiple regression. The approach used time series data to predict future points in the series and has been widely used to forecast influenza activity (6-7). Unlike the conventional autoregressive integrated moving average method, it allowed for self-selection of multiple lags of past observations as model inputs. As such, it was capable of automatically incorporating the seasonality and stationarity in influenza epidemics as well as changes in other time-serial inputs (e.g., mobility levels and mask-wearing interventions).
Two self-correcting regularized multiple regression models were dynamically trained and regularized with the least absolute shrinkage and selection operator (LASSO) method. First, a linear combination of multiple lags of influenza activity, the current weekly domestic mobility, and the current weekly international mobility was used to fit the weekly percent positivity under the mobility change only. Second, we fitted the observed influenza percent positivity under combined NPIs using the current weekly mask-wearing intervention as well as the predicted influenza activity under the mobility mitigation alone. A separate model was fitted for each of the four regions. The fitted models were then projected into the 2021–2022 season to forecast the influenza activity under different NPIs.
In the analysis, we assumed that there was no substantial difference in climate conditions, sociodemographic features, influenza transmissibility as well as influenza vaccination coverages in 2020–2021 compared with the previous years. We also assumed that the impacts of these external factors in influenza were consistent and could be captured by past influenza activity. We further considered alternative assumptions on the NPIs, including differential assumptions on timing of mask-wearing, magnitude of mobility mitigation, intensity of mask-wearing, and coordination of mask-wearing with vaccination. The model was implemented in scikit-learn 0.24.2 with Python (version 3.6.13, Python Software Foundation, Fredericksburg, VA, US).
-
Under the scenario without COVID-19 mitigation measures, we predicted that influenza percent positivity would be 18.6 [95% confidence interval (CI): 13.1, 24.2] and 16.9 (95% CI: 12.7, 21.6) for Northern China and Southern China, and 10.5 (95% CI: 6.4, 14.1) and 13.4 (95% CI: 9.3, 17.4) for England and the US, respectively. In Southern China, the rebound could continue until the summer with a secondary peak, a pattern more similar to that in the years before 2018 than in recent years (Figure 1B).
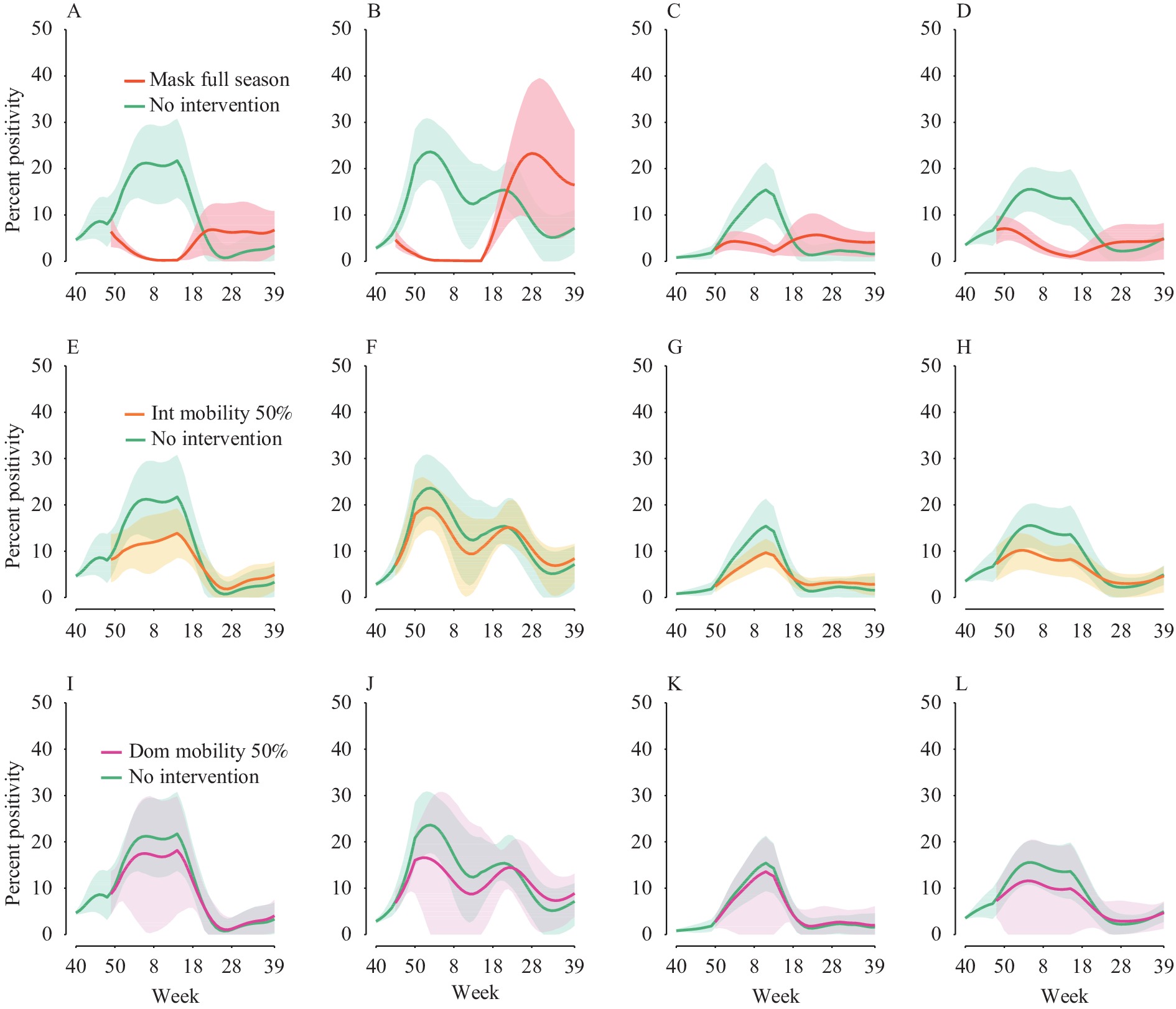 Figure 1.
Figure 1.Predicted influenza activities in 2021–2022 season under no NPI and varying NPIs. Weekly percent positivity under mask-wearing intervention for (A) Northern China, (B) Southern China, (C) England and (D) the US. Weekly percent positivity under international mobility mitigation being reduced by 50% for (E) Northern China, (F) Southern China, (G) England and (H) the US. Weekly percent positivity under domestic mobility mitigation being reduced by 50% for (I) Northern China, (J) Southern China, (K) England and (L) the US. Shaded area refer to 95% CI.
Abbreviations: NPIs=non pharmaceutical interventions; CI=confidence intervals.Influenza activity was projected to stay at a low level with percent positivity below 10.0 if the mask-wearing could continue throughout the 2021–2022 season. Late-season rebounds were observed in Southern China if the mask intervention were relaxed. For all regions, if the intervention were relaxed in the mid of influenza season, a sharper rebound could occur (Figure 2). When implemented in the full 2021–2022 season, mask-wearing alone could reduce 7.0–16.8 influenza activity in the four regions (Table 1).
 Figure 2.
Figure 2.Predicted influenza activities in 2021–2022 season under NPIs with alternative assumptions. Weekly percent positivity under no interventions and three timings of mask-wearing intervention, implemented during the full influenza season, the first half of the season the second half of the season, for (A) Northern China, (B) Southern China, (C) England and (D) the US. Weekly percent positivity under international mobility mitigation measures, assuming the international mobility reduced by 30%, 50% or 70%, for (E) Northern China, (F) Southern China, (G) England and (H) the US.
Note: Weekly percent positivity under domestic mobility mitigation measures, assuming domestic mobility reduced by 30%, 50% or 70%, for (A) Northern China, (B) Southern China, (C) England and (D) the US. Abbreviation: NPIs=non pharmaceutical interventions.NPIs Northern China Southern China England United States Mean 95% CI Mean 95% CI Mean 95% CI Mean 95% CI Mask-wearing alone 16.8 (11.5, 22.2) 15.9 (11.8, 20.6) 7.0 (4.2, 9.5) 9.3 (6.2, 12.4) International mobility alone (Reduced by 50%) 7.2 (3.8, 10.7) 3.2 (1.0, 5.4) 3.7 (1.5, 5.7) 4.6 (1.9, 7.3) Domestic mobility alone (Reduced by 50%) 3.0 (−2.6, 11.9) 4.7 (−4.2, 12.9) 1.2 (0, 8.9) 3.3 (0, 14.1) Abbreviation: NPIs=non pharmaceutical interventions. Table 1. Predicted reductions on percent positivity under alternative NPIs (relative to no NPIs) in 2021–2022 season.
Our projected estimates for the mask-wearing intervention relied on the actual acceptance of mask-wearing measures during the COVID-19 period. Should a mask-wearing measure with a magnitude 70% less than that during the COVID-19 period be implemented, the incoming winter could still have a modestly large influenza outbreak (Figure 3E–H). Nevertheless, when coordinated with an appropriate vaccination program, a much less stringent mask-wearing measure was capable of keeping the influenza activity at low levels. For example, if an extra of 20% population were vaccinated with influenza vaccines [considering 60% efficacy at all age groups (8)] before the influenza season starts, a winter mask-wearing intervention with only 30% magnitude of that in the COVID-19 period for about two months, was able to reduce influenza activity to low levels (Figure 3I–L).
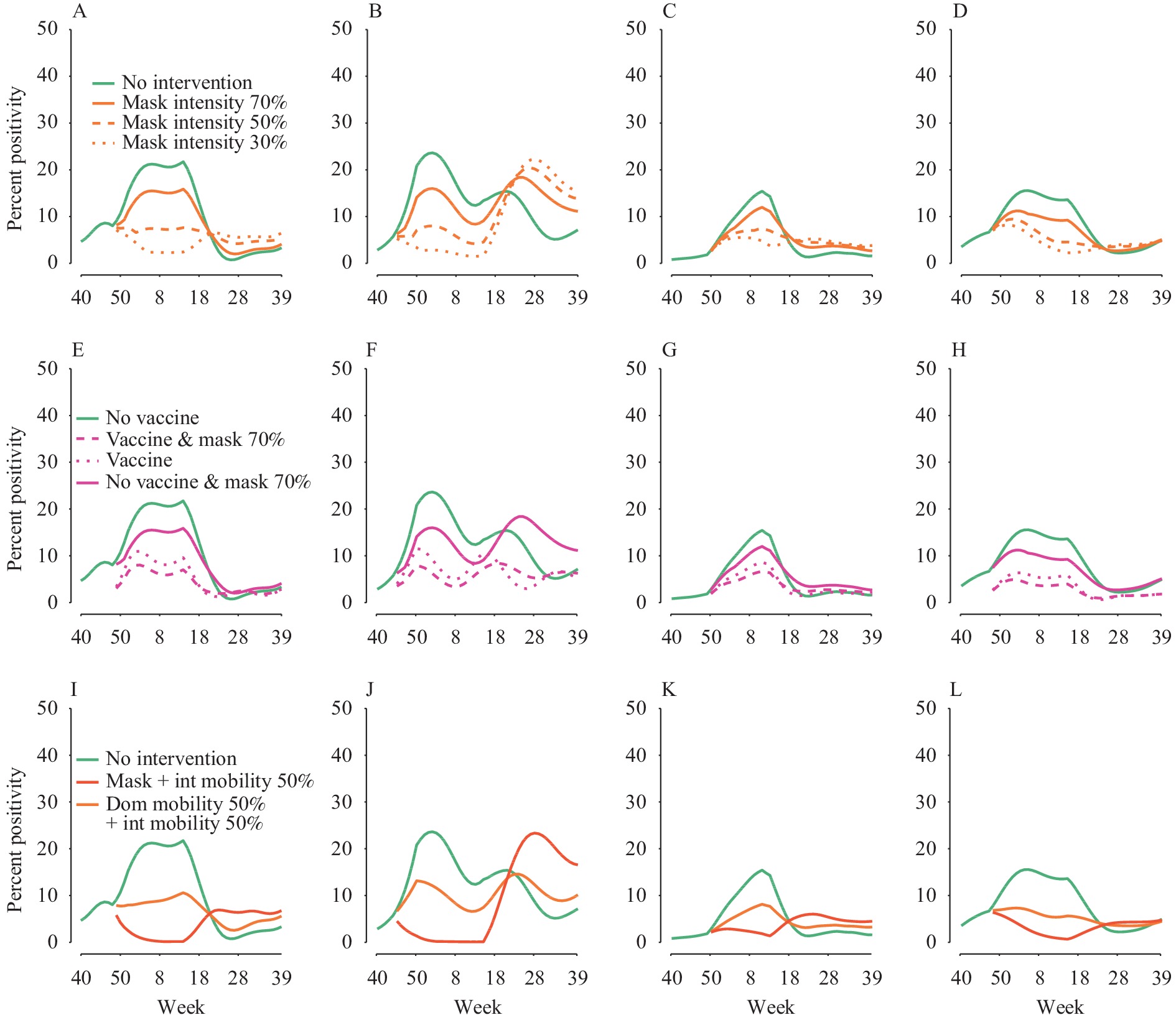 Figure 3.
Figure 3.Predicted influenza activities in 2021–2022 season under alternative mask-wearing interventions and combined NPIs. Weekly percent positivity under no intervention and the differential magnitude of mask-wearing intervention, for (A) Northern China, (B) Southern China, (C) England and (D) the US. Weekly percent positivity under alternative scenarios considering a mask-wearing intervention with intensity 70% less than (i.e., 30% of) that during the COVID-19 period coordinated with a vaccination program where an extra 20% population vaccinated at 60% vaccine efficacy, for (E) Northern China, (F) Southern China, (G) England and (H) the US. Weekly percent positivity under combined NPIs, mask-wearing and 50% reduction on international mobility as well as 50% reduction on both domestic and international mobility for (I) Northern China, (J) Southern China, (K) England and (L) the US.
Abbreviations: NPIs=non pharmaceutical interventions; COVID-19=coronavirus disease 2019.Finally, the rebound would also be smaller if international mobility mitigation measures continued only, but the decline depended on the magnitude of the mitigation as well as the past seasonal patterns. Only in regions with the influenza profile exhibiting a single winter-peak outbreak, e.g., Northern China, England, and the US, and with mobility reduced by 50% or higher from normal levels, influenza activity could be deflected substantially (Figures 1 and 2). As expected, simultaneously mitigating both international mobility and domestic mobility could flatten the influenza activity (Figure 3I–L). We estimated that reducing 50% of the international mobility, relative to normal mobility prior to the COVID-19 pandemic, could reduce 3.2–7.2 positivity in the 4 study regions. Domestic mobility mitigation was likely to have a smaller impact than international mobility except in Southern China, where reducing domestic mobility during the influenza season by half could maintain influenza activity at markedly lower levels (Figure 1J and Figure 2). We estimated that reducing 50% of the domestic mobility could reduce 4.7 (95% CI: –4.2, 12.9) influenza activity in Southern China and 1.2–3.3 in the other three regions (Table 1).
-
Influenza activity in the 4 regions was projected to rebound in the incoming 2021–2022 season and the season could be longer and blunter compared to the recent influenza epidemics in 2017–2019, if all the current community mitigation measures are eased. Similar rebounds have been found in severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2) circulation when the NPIs were lifted (9). Notably, the pattern of influenza activity in Southern China would be more similar to that before the year 2018 than that in the recent years, i.e., having a secondary summer peak. Given these new findings, it is important to plan for a longer influenza circulation season this winter and spring.
This study identified sharp rebounds after lifting the mask-wearing intervention in the middle of influenza season. Our findings support the relevance of immunity debt where low viral exposure may spur a growing proportions of susceptible people due to a lack of immune stimulation (10). However, we also found that the long period of low exposure to influenza virus — i.e., the plummeting of influenza throughout the year 2020, instead could induce a blunter 2021–2022 season as compared to recent epidemics in 2017–2019 in all 4 regions. The difference could be due to the short duration of protective immunity against influenza virus (8,11) or the naturally small susceptible population in interannual seasons, where in either case the size of susceptible population in the long term is only loosely related to the infection history. Further work is needed to better understand how the immunity debt varies at the timing and period of low exposure to influenza virus.
The study was subject to some limitations. First, the change of domestic mobility patterns during the COVID-19 period closely coincided with several domestic mobility related NPIs, our analysis on domestic mobility thus cannot further distinguish the highly correlated mobility-related NPIs such as movement restriction and physical distancing. Second, our estimated effectiveness of the mask-wearing order may depend on the type of mask in use (12), and the presence of other personal protection behaviour (e.g., hand hygiene and respiratory etiquette), a detailed knowledge of these NPIs could help to depict a more complete picture of the dynamics of influenza under different NPIs. Finally, the analysis for the United Kingdom was limited to England.
Our results are highly timely in this context where there is a high uncertainty on the upcoming strains, due to the long period of low-exposure to influenza viruses; and with respect to the high interannual variation in circulating strains and subtypes as well as the complication of antigenic immunity changes in response to vaccines (13-14), our findings could also have a far-reaching impact for preventing influenza pandemics. Vaccination is one of the most effective measures in influenza control. Identifying and developing universal vaccines, as well as increasing the vaccination capacity (15) are of primary importance after influenza’s long-term disruptions to seasonal patterns. However, as the influenza season is approaching and a large part of a population has not been protected by vaccines, there is an increasing call for coordinated mitigation measures. We found that wearing mask for a short period could be highly beneficial in reducing influenza transmission in these contexts. In light of the relatively low negative impacts on society, in the future, mask-wearing could be implemented during influenza epidemics to reduce transmission, particularly in populations at highest risk for developing severe disease or complications or when targeted vaccines are not available.
-
The authors declared no competing interests.
HTML
| Citation: |



 Download:
Download:




