-
On July 3, 2019, Zhangping City reported an outbreak of brucellosis in a family cluster. The patients were a mother and a daughter (Patients I and II). Except for drinking goat milk produced and bottled from a local farmer, there was no other suspected exposure, so foodborne infection was highly likely. The city only reported 1 case of human brucellosis in 2011 (Yongfu County) and 1 case in 2017 (Heping County). Livestock were not routinely vaccinated against brucellosis. After the second reported case in 2017, the municipal-level agricultural department carried out a general investigation of brucellosis among livestock. The targeted prevention and control recommendations were put forward to determine the source of the epidemic and risk factors, and onsite investigations were carried out.
HTML
-
The suspected case definition was as follows: onset of patient illness occurred during the period from January 1 to July 3, 2019; residents of Zhangping City with fever, hyperhidrosis, muscle or joint pain, or fatigue; patient symptoms might be accompanied by liver, spleen, lymph nodes, testicular swelling, and other manifestations; and the rose Bengal test (RBT) result was positive. The confirmed case definition was as follows: a serum (tube) agglutination test (SAT) of titer ≥1∶100; or a suspected case with isolated Brucella from the patient’s blood, bone marrow, other body fluids, and excrement by bacterial isolation and culture. The recessive infection definition: RBT was positive but no clinical manifestations were detected.
Case searching was performed by acquiring case records, laboratory test reports, and interviews in local hospitals. Blood samples were taken from the dairy farmer (Mr. C) suspected of producing the goat milk that led to this outbreak, Mr. C’s family members, and those who had drunk goat milk from Mr. C’s farm between January 1 and July 3, 2019. In addition, further investigations were conducted into the hygiene habits of goat milk consumers; the breeding and quarantine of pigs, cattle, and goats in Zhangping City; the processing and supply of dairy products in Heping County; and sampling and quarantining the milk goats in Heping County.
If a RBT-positive person was found during the case search, the detailed demographic data, clinical data, eating habits, occupational history, preventive measures, and exposure history would be collected. If a patient had other suspected exposures, blood samples were tested to identify the source of infection.
A total of 146 persons were sampled during the case search, and 6 confirmed cases were found. One of the blood specimens was cultured as Brucella ovis. All patients had symptoms of fatigue, 5 cases (83%) were accompanied by fever, 2 cases (33%) had hyperhidrosis and muscle aches, and 1 case (17%) had vomiting, chills, and headache. There were no severe deaths or recessive infections. The male-to-female ratio was 1∶5, including 3 workers, 2 unemployed houseworkers, and 1 student. The cases were from 4 households, all within the delivery scope of goat milk of Mr. C, and no other epidemiological association was found. Only one patient experienced onset of symptoms in April, and the remaining patients experienced onset from May 27 to June 12.
Except for Patient V who was engaged in pig offal processing, the other patients’ only suspected exposure was the raw goat milk (Table 1). The RBT test was negative for Patient V’s coworkers and blood samples from the pig offal, which reduced the likelihood of transmission through pig offal processing. A total of 2 private farms in Zhangping City supplied fresh goat milk. Mr. C’s dairy farm was a family workshop that did not abide by adequate sanitation measures, and 3 sampling specimens of Mr. C’s dairy goats were positive for RBT (++++) while samples from the other dairy farm tested negative, confirming that the source of the infection was the dairy goats from Mr. C’s dairy farm.
Case number Suspected exposure Drinking method Onset date Main symptoms Lab results RBT SAT* I (index case) Goat milk Warm bath* or direct consumption June 1 Fever, sweating, fatigue Positive 1:400 II Goat milk Warm bath or direct consumption June 3 Fever, fatigue Positive 1:400 III Goat milk Warm bath or direct consumption June 12 Fever, vomiting, fatigue Positive 1:400 IV Goat milk Direct consumption April 3 Muscle aches, fatigue Positive 1:100 V Goat milk and processing pork Direct consumption May 27 Fever, muscle aches, sweating, fatigue Positive 1:200 VI Goat milk Warm bath or Direct consumption June 10 Headache, fever, chills, fatigue Positive 1:800 Abbreviations: RBT=rose Bengal test; SAT=Serum agglutination test.
* Warm bath: warming up the milk to a suitable temperature by bathing it into warm water.Table 1. Summary of cases in a brucellosis outbreak in Zhangping City, Fujian Province in 2019.
This epidemic was the first outbreak of brucellosis among livestock in Zhangping City, and further investigations were needed to find the source of the infected dairy goat. The environmental investigation found that Mr. C’s dairy farm was a closed iron goat pen so that the goat could not contact other animals. Because Mr. C’s goats did not have a quarantine certificate, the infected dairy goat was likely purchased by Mr. C as the last quarantine record of a dairy goat he possessed was in 2014. Mr. C brought dairy goats twice: in 2016, 60 goats were purchased from a neighboring village in Zhangping City; and in 2017, an additional 2 dairy goats were purchased in Zhangping City from Mr. Y, one of which was likely the infected goat. The goats had been slaughtered and sold, and the relevant personnel’s serum RBTs were all negative. The dairy goats were still maintained when the outbreak occurred. Mr. C stated that the goats had “slow growth and low milk production.” One of the goats gave birth to lambs in early March 2019. The peak of infected milk lamb chops was after lambing (1) and combined with the case’s onset date and the incubation period of brucellosis. It was speculated that Y’s milk goat was the source of infection for this outbreak (Figure 1).
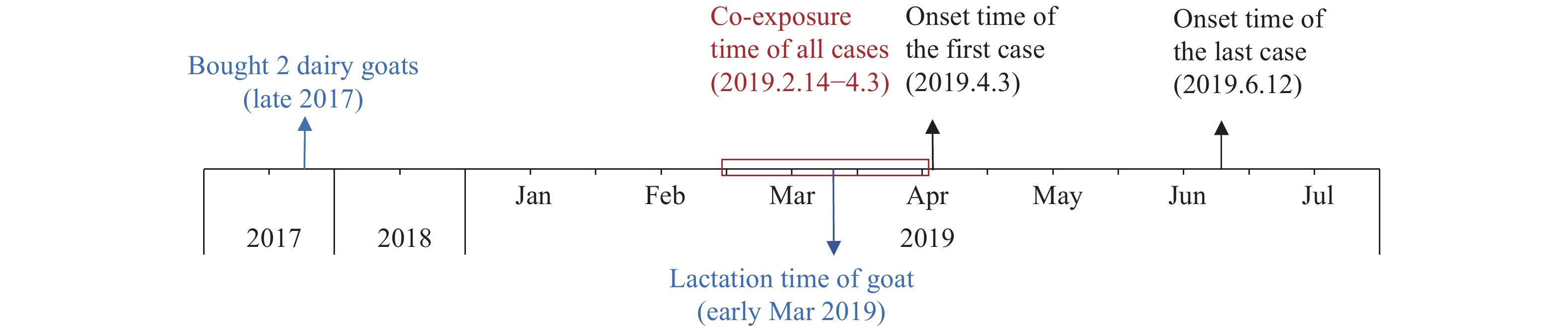 Figure 1.
Figure 1.Timeline of the dairy farmer, Mr. C, purchasing the brucellosis-infected goats and the incidence of cases in the outbreak in Fujian Province, April–June, 2019.
A retrospective epidemiological investigation into the goat producer Mr. Y showed that Mr. Y’s goats had their first brucellosis case in Heping City on August 29, 2017. On August 1, 2017, Mr. Y bought 15 goats from a northern region (the specific source is unclear) and contracted brucellosis after slaughtering the goat with his bare hands with palms that had ruptured skin. During the local animal epidemic control department’s investigation, Mr. Y had killed or sold most of the goats, and no brucellosis was detected in the remaining 3 dairy goats. During this investigation, Mr. Y admitted that he sold 2 goats to Mr. C before culling by the animal husbandry department to reduce losses. Although the agricultural department carried out a general survey of brucellosis among livestock, his goat farm was not quarantined because Mr. C left the same day. The infected dairy goats were not found.
-
All dairy goats in Mr. C’s farm were culled and buried, and disinfection was conducted for the buildings. Medical institutions at all levels in Zhangping City were trained to strengthen diagnostic capabilities and brucellosis treatment. All goat breeders received health and hygiene education, and local farmers were trained on use of personal protection and the need for goat quarantine, especially to reduce incidence of brucellosis. Residents who consumed goat milk were recommended to monitor symptoms closely for an extended period after the outbreak.
-
In this outbreak investigation, importing an infected goat was the core link that likely caused the local brucellosis outbreak. In recent years, China’s brucellosis disease burden had gradually spread from northern pastoral and semi-pastoral areas to southern non-pastoral regions (2-4). The main reason could be the increase in livestock trading between the north and south and increased private free-range livestock in the south. But the involved stakeholders’ awareness and use of quarantine measures were relatively weak, causing an influx of infected animals and products from north to south (4). The investigation found that individual traders did not have compulsory quarantine measures in all aspects of purchasing, breeding, selling, and slaughtering livestock and their biological products. Practitioners had no incentive to submit them for inspection. Therefore, for non-endemic areas, preventing the import of infected animals and strengthening practitioners’ and the general public’s awareness for disease prevention has significant public health significance. The government should enhance the quarantine of transregional livestock transportation and local disease screening.
Because brucellosis symptoms in livestock are relatively hidden, outbreak control depends more on practitioners’ active cooperation. The survey showed that the basic-level goat breeders’ main paths for brucellosis prevention were veterinarians, traditional health education materials, and relatives and friends (5). Therefore, veterinary departments are encouraged to use their contact with goat breeders to strengthen practitioners’ awareness of the effectiveness of quarantine measures for their livestock.
In recent years, food-borne brucellosis had repeatedly occurred in southern China (6-9). Contaminated dairy products were an important route of transmission of brucellosis (9-10). The interview found that residents in Zhangping City generally believed that raw milk products were more nutritious and were not aware of the possible health risks of raw milk products. As people’s awareness of brucellosis was low, governments in low-risk areas should strengthen food safety inspections and management and raise the people’s awareness of food safety.
This investigation was subject to some limitations. The local animal epidemic control department did not number when sampling and culling the dairy goat. During this investigation, the disease control agency could not obtain a quality sample from Mr. C’s dairy goat. The quality of the blood sample available was poor, and the blood culture did not grow, so the animal disease control department could not obtain etiological evidence of infected dairy goat.
| Citation: |



 Download:
Download:




