2021 Vol. 3, No. 45
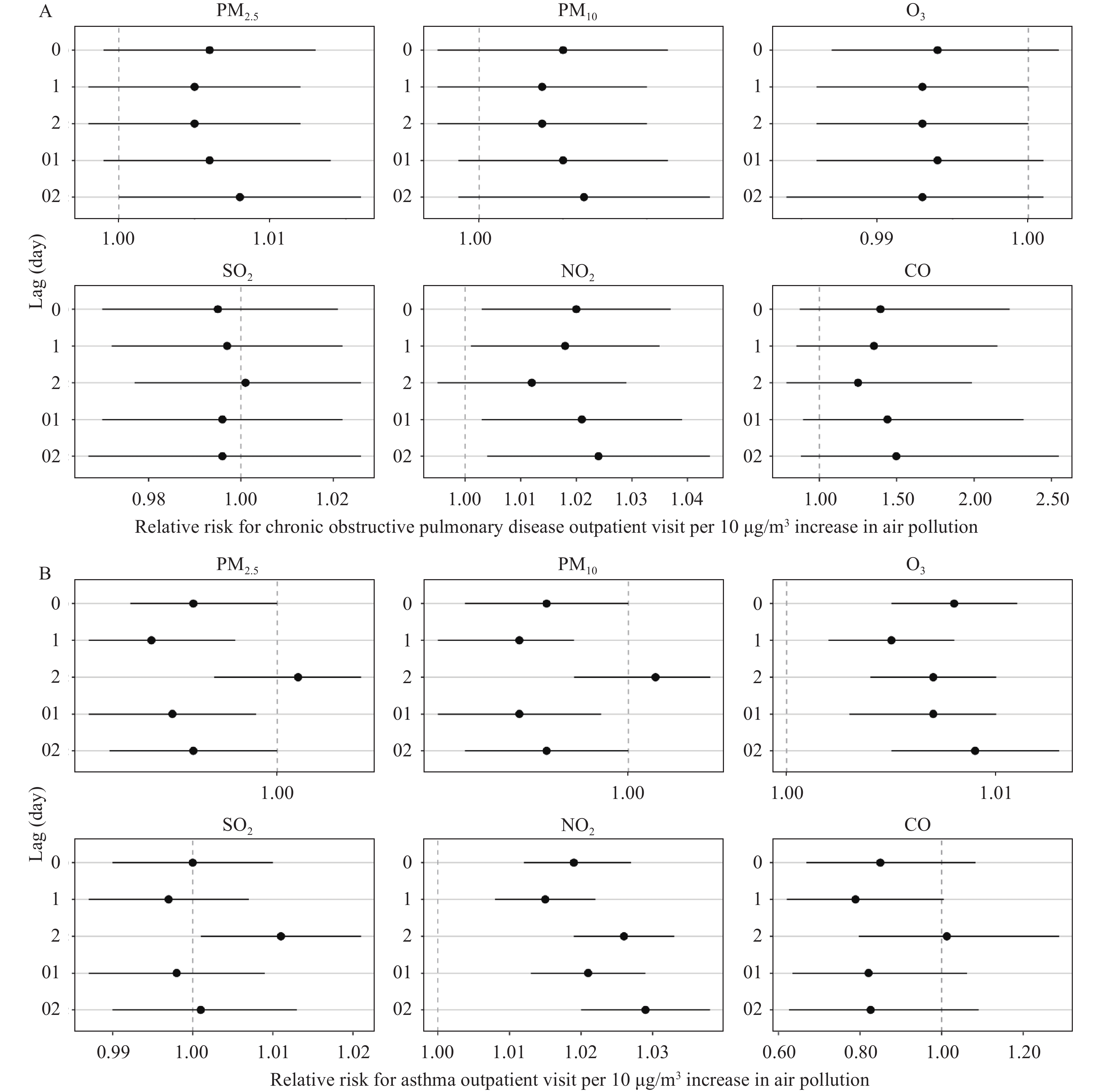
Short-term exposure to air pollutants has been associated with chronic obstructive pulmonary disease (COPD) and asthma, which needs continuous observation.
This study uses the longest time series data so far from 2013 to 2018 and adds additional data analysis for ozone (O3) to existing studies.
This study suggests that air pollutants have certain acute effects on outpatient and hospital admission of patients with COPD and asthma, which can be combined with the disease diagnosis and treatment guidelines to guide clinical practice.
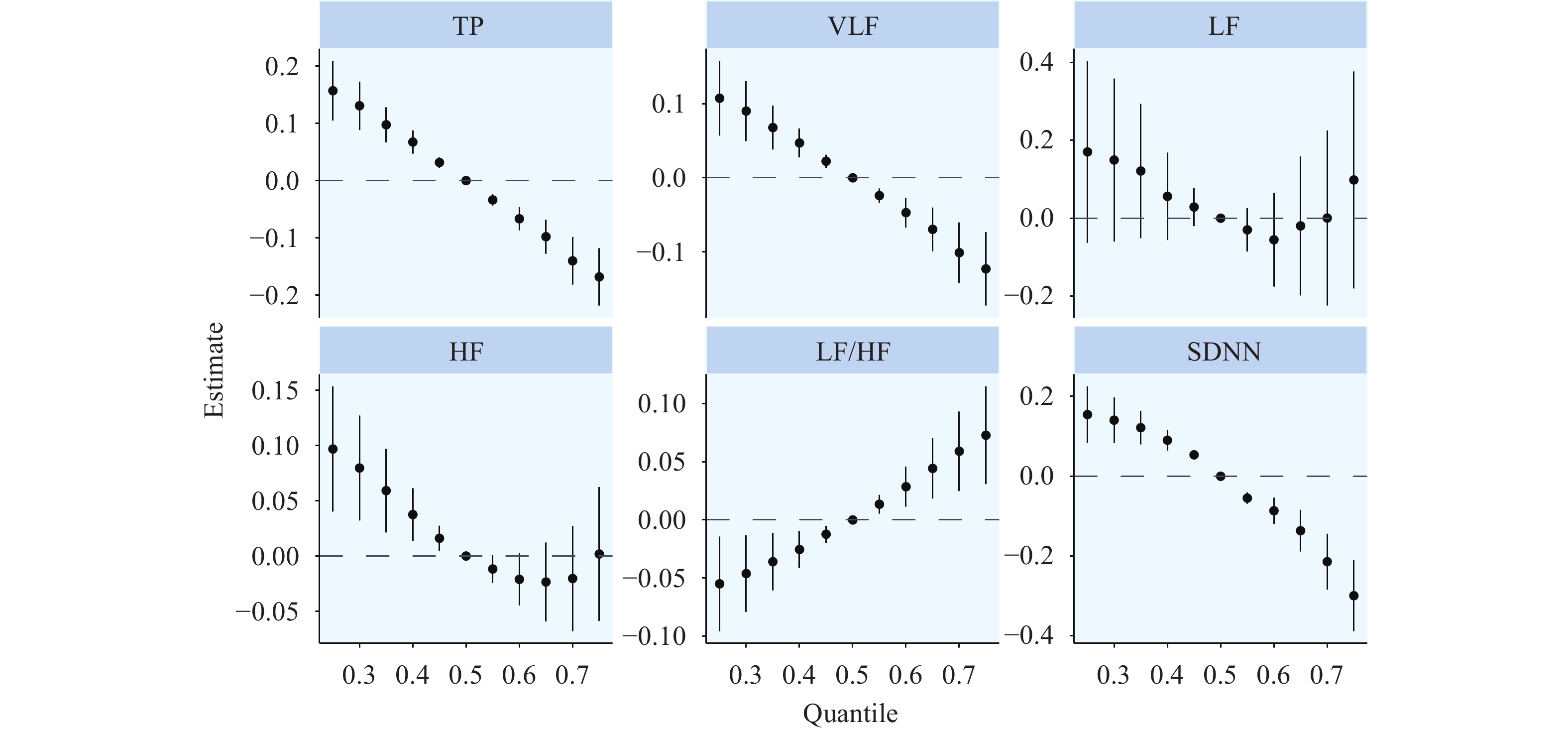
Short-term PM2.5 exposure has been associated with hourly, 24-hour, daytime, and nighttime blood pressure (BP) levels, and further studies focusing whether and how the associations with other ambulatory BP monitoring indicators are warranted.
This study observed that short-term PM2.5 exposure was associated with BP elevations and was the first to report the associations of short-term PM2.5 exposure with BP variability. Circadian rhythm of BP and BP load among hypertensive patients were found to be modified by controlled BP status or taking angiotensin receptor blockers (ARBs).
This study suggested that antihypertensive therapy, especially with well-controlled BP status may be potential measurements to attenuate adverse impacts of PM2.5 for hypertensive patients with intermediate-to-high risk of cardiovascular disease (CVD).
It remains inconclusive whether short-term ozone exposure can cause an inflammatory response and oxidative damage in the circulatory system, particularly at low concentrations.
This study made an accurate exposure assessment by conducting personal ozone monitoring, thus minimizing the exposure misclassification commonly found in previous environmental epidemiological studies. Our study found that even short-term exposure to low concentrations of ozone was associated with inflammation, lipid peroxidation, and mitochondrial oxidative damage.
Short-term exposure to low concentrations of ozone can still lead to subclinical cardiovascular effects, suggesting the current air quality standards for ozone need to be further tightened in China.
With rapid urbanization, traffic-related air pollution has become a global concern. However, its association with cardiovascular health has not been fully elucidated.
This study provided novel evidence of the joint cardiovascular effect of multiple pollutants in subway cabins, further identified two pollutants that played dominant roles, and validated the effectiveness of targeted interventions.
The findings were helpful to guide the formulation and development of prevention and control strategies for key traffic-related pollutants that endanger the cardiovascular health of commuters.
Ozone (O3) is a weather-driven photochemical ambient pollutant, and its harm to human health may be affected by meteorological factors such as temperature. However, there is conflicting evidence regarding whether temperature can modify the effects of ozone on health.
Short-term exposure to O3 in the Beijing Municipality, Tianjin Municipality, Hebei Province, and surrounding areas was associated with an increased risk of human mortality and that association was positive modified by relatively higher (>75th 24 h-average temperature) or extreme cold temperature (<10th 24 h-average temperature). Under extreme temperatures (>90th 24 h-average temperature) modification, the associations were further increased. Cardiopulmonary diseases, as vulnerable diseases of air pollution, their mortality risks associated with O3 were markedly strengthened by uncomfortable temperatures.
This study suggests that policymakers should pay attention to the synergistic effect between ozone and heat or extreme cold on human health, as well as provide evidence for establishing an integrated early-warning system to protect the public against both uncomfortable temperature and air pollution.



 Subscribe for E-mail Alerts
Subscribe for E-mail Alerts CCDC Weekly RSS Feed
CCDC Weekly RSS Feed