-
Introduction: On June 26, 2025, a hospital in Luoyang City reported a suspected case of Streptococcus suis infection. The local CDCs immediately initiated an epidemiological investigation upon notification.
Methods: Blood samples were collected from the patient for microbial culture. The isolated strain HN04 underwent species identification and phylogenetic analysis through matrix-assisted laser desorption/ionization time-of-flight mass spectrometry (MALDI-TOF MS), real-time quantitative polymerase chain reaction (qPCR) targeting Streptococcus suis-specific nucleic acid sequences, and whole-genome sequencing.
Results: MALDI-TOF MS initially identified strain HN04 as Streptococcus suis; however, the S. suis-specific qPCR assay produced a negative result. Average nucleotide identity (ANI) analysis definitively identified HN04 as Streptococcus parasuis. Phylogenetic analysis revealed that HN04 is distantly related to previously reported clinical isolates from China. Epidemiological investigation found no documented history of livestock contact, particularly with pigs, suggesting environmental exposure as the likely transmission route.
Conclusions: This study documents the first confirmed human case of Streptococcus parasuis infection in Henan Province, suggesting widespread environmental distribution of this pathogen and highlighting the need for surveillance beyond occupational risk groups. We recommend including S. parasuis in the differential diagnosis for patients presenting with severe traumatic infections even in the absence of livestock contact history. Enhanced environmental surveillance systems and rapid diagnostic capabilities are urgently needed. These findings provide critical insights into the epidemiological characteristics and transmission dynamics of S. parasuis.
-
On June 26, 2025, the Jinghua Campus of the First Affiliated Hospital of Henan University of Science and Technology reported a suspected case of Streptococcus suis infection. The Luoyang CDC immediately initiated an epidemiological investigation and submitted the isolated strain, designated HN04, for laboratory analysis. Through collaborative verification by the Henan Provincial CDC and the Luoyang CDC, the strain was definitively identified as Streptococcus parasuis, representing the first documented human infection with this pathogen in Henan Province.
-
On June 23, 2025, at 9∶00 AM, a 69-year-old male sanitation worker was admitted to the Jinghua Campus of The First Affiliated Hospital of Henan University of Science and Technology with a diagnosis of “a lower limb injury”. His left foot had been crushed by a garbage truck during work, resulting in significant hemorrhage. The patient reported good general health with no history of hypertension, diabetes, heart disease, or cerebrovascular disease. Upon admission, his body temperature was normal (36.8 °C). Complete blood count results revealed a white blood cell (WBC) count of 8.5×109/L, with a neutrophil percentage of 92.90% and a lymphocyte percentage of 4.40%. The C-reactive protein (CRP) concentration was 23.15 mg/L. A venous blood sample was collected for blood culture. At 13∶00, prophylactic anti-infective therapy with cefoperazone sodium and sulbactam sodium was initiated and administered every 8 hours for a total of three doses. A left below-knee amputation was performed at 19∶00, lasting 75 minutes. Postoperatively, the prophylactic anti-infective agent was changed to cefuroxime sodium, administered every 8 hours for three consecutive days. On June 26, the hospital cultured a bacterial strain designated HN04 and identified it as Streptococcus suis by matrix-assisted laser desorption/ionization time-of-flight mass spectrometry (MALDI-TOF MS). The hospital reported the case on the same day, and the HN04 strain was sent to both the Luoyang CDC and the Henan Provincial CDC for verification. No microorganisms were isolated from the blood culture on July 1. On July 10, the complete blood count showed a WBC count of 6.85×109/L, with a neutrophil percentage of 77.60% and a lymphocyte percentage of 17.40%. With active treatment, the amputation wound healed well, and the patient was discharged on July 14.
On June 26, following the hospital report, the Luoyang CDC conducted an epidemiological investigation at both the patient’s home and the hospital. The investigation revealed that the patient’s household did not raise pigs or other livestock, no pig farms existed in the vicinity of his residence, and he had no routine contact with raw pork or sick pigs. From 2023 to the present, a total of 365 Streptococcus strains have been cultured and identified at the Jinghua Campus of The First Affiliated Hospital of Henan University of Science and Technology, but no S. suis had been detected. No additional cases of S. suis infection were identified in the patient’s ward or hospital-wide.
On June 27, the Luoyang CDC tested the HN04 strain using a S. suis nucleic acid detection kit, which yielded a negative result. Subsequently, the Henan Provincial CDC successfully amplified a 679 bp fragment using S. parasuis recN-specific primers (1). Whole-genome sequencing of strain HN04 (Accession number: SRR35358561) was completed on August 13, and Average Nucleotide Identity (ANI) analysis definitively identified the isolate as S. parasuis. Phylogenetic analysis based on whole-genome single nucleotide polymorphisms (wgSNPs) revealed that strain HN04 occupied a distinct phylogenetic branch from six other human-derived S. parasuis isolates previously reported in China, with ANI values ranging from 97.69% to 97.85% (Figure 1).
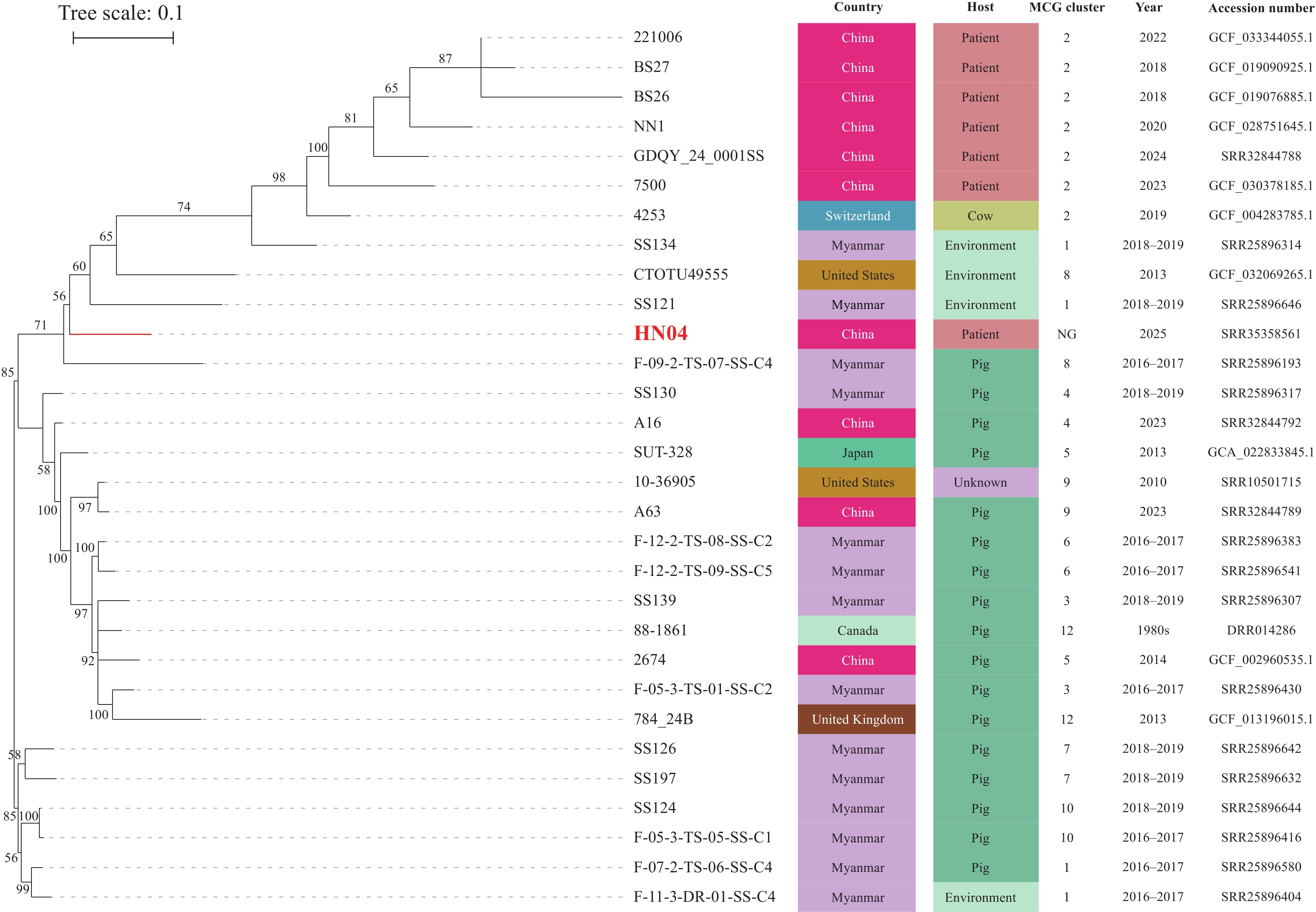 Figure 1.
Figure 1.Whole-genome single nucleotide polymorphism (wgSNP) phylogenetic analysis of strain HN04 from Henan Province, China (June 2025), constructed using the Neighbor-Joining method.
Note: Following the minimum core genome (MCG) typing strategy developed by Zhang et al. (2), we constructed a phylogenetic tree using strain SUT-286 (GCA_021654455.1) as the reference genome. The analysis incorporated two representative strains from each MCG group, with the exception of MCG2, for which all seven available strains were included. Bootstrap analysis was performed with 1,000 replicates.
“NG” designates MCG non-groupable genomes.
-
Following receipt of the hospital report, the Luoyang CDC promptly initiated comprehensive investigation and control measures. Environmental disinfection was performed at the patient’s residence and in surrounding areas, including garbage trucks, waste collection bins, and pig farms in Xiaolangdi Town. The animal disease control department was notified of the outbreak, and a coordinated joint investigation and response mechanism for zoonotic diseases was activated. The Luoyang CDC provided guidance to the hospital regarding patient isolation protocols, clinical management, and facility-wide infection prevention and control practices. Active case finding was conducted throughout the village and township where the index case resided, with no additional cases identified to date.
-
This study identified S. parasuis through whole-genome sequencing of a blood culture isolate from a patient injured in a traffic accident, representing the first documented human case of S. parasuis infection in Henan Province. Notably, the patient reported no history of contact with live pigs or pork products. Phylogenetic analysis revealed that the isolated strain was distantly related to previously reported clinical isolates from other regions of China.
Human infections with S. parasuis have been documented in Guangxi Zhuang Autonomous Region and Guangdong Province in China, with clinical presentations typically including fever accompanied by peritonitis, pneumonia, or meningitis, consistent with the pathogenic profile of S. parasuis (3-4). The index case reported here lacked these characteristic clinical manifestations, likely due to prompt initiation of prophylactic antibiotic therapy following the traumatic injury. Subsequently, two additional S. parasuis infections were identified in Luoyang City. The first involved a patient with severe burns from a liquefied gas explosion, in whom S. parasuis was detected in wound secretions; this patient’s critical condition resulted in death. The second case presented with fever and retching, with physical examination revealing extensive erythematous rashes and edema on the left leg, waist, and chest. This patient was diagnosed with sepsis, and S. parasuis was isolated from blood culture. Following targeted antibiotic therapy, the patient recovered and was discharged. Importantly, neither of these subsequent cases reported contact with pigs or other livestock. Phylogenetic analysis of strains from all three cases demonstrated genetic diversity, indicating independent sporadic infections rather than a common-source outbreak. Current research on S. parasuis remains limited, with no evidence supporting human-to-human transmission. However, the etiological findings and exposure patterns observed in these cases suggest that S. parasuis may be widely distributed in the local environment. This environmental persistence raises concern for continued sporadic human and livestock infections, with the potential for localized case clusters in the future.
Given the limited clinical reports on S. parasuis and the scarcity of reference strain data in existing MALDI-TOF MS databases, accurate differentiation from S. suis in clinical settings remains challenging (5–6). During this investigation, the hospital initially identified the pathogen as S. suis by MALDI-TOF MS, with confirmation as S. parasuis only achieved through whole-genome sequencing. This diagnostic limitation, combined with the lack of routine molecular testing, indicates that both the infection rate and public health risk of S. parasuis may be substantially underestimated (7). Although S. parasuis is phylogenetically related to S. suis, the two species differ significantly in antibiotic resistance gene profiles, pathogenic mechanisms, and the inflammatory responses they trigger in hosts. Furthermore, S. parasuis itself exhibits considerable genomic heterogeneity (3,8), complicating both identification and treatment. Accurate species-level identification is therefore essential for guiding empirical antibiotic therapy and ensuring appropriate clinical management. The transmission dynamics of S. suis are closely associated with occupational pig exposure. If S. parasuis cases are misclassified as S. suis in surveillance data, the true disease burden will be obscured, preventing public health systems from detecting emerging transmission patterns and identifying at-risk populations beyond traditional occupational groups. Moreover, given the limited current understanding of S. parasuis pathogenicity and pathophysiology, accurate differentiation and identification provide the foundation for conducting mechanistic research, developing targeted therapeutic strategies, and properly assessing its public health and clinical significance. Establishing and implementing rapid, species-specific laboratory detection systems for S. parasuis — such as PCR assays targeting unique genetic markers — represents a critical prerequisite for enhancing surveillance sensitivity and improving clinical outcomes.
Notably, none of the three cases identified in Luoyang City reported direct contact with live pigs or pork products, a finding that diverges substantially from the traditional epidemiological pattern of S. suis infection, which predominantly affects occupational groups with livestock exposure. All three patients presented with skin lesions prior to hospitalization. While this observation raises the possibility of environmental persistence of S. parasuis, the absence of environmental sampling during this investigation limits our ability to establish definitive transmission pathways. Future investigations should prioritize comprehensive environmental surveillance to identify potential contamination sources and elucidate transmission routes. These findings carry important clinical implications: clinicians should consider S. parasuis in the differential diagnosis of patients presenting with fever, neurological symptoms, or sepsis, even without documented animal contact history. Antimicrobial selection should be guided by susceptibility testing when available. From a public health perspective, these cases underscore the need for environmental sampling and targeted disinfection protocols during outbreak response. Prevention and control strategies for S. parasuis infection must extend beyond occupational health frameworks to encompass population-wide surveillance and systematic investigation of environmental transmission pathways.
This report documents the first confirmed human case of S. parasuis infection in Henan Province and provides a valuable bacterial isolate for developing rapid diagnostic assays, conducting antimicrobial susceptibility studies, and investigating virulence mechanisms. Given the emerging recognition of S. parasuis as a human pathogen, strengthening surveillance systems is essential to better characterize its epidemiological patterns and pathogenic properties.
HTML
Investigation and Results
Public Health Response
| Citation: |



 Download:
Download:




