-
Introduction: To analyze human immunodeficiency virus (HIV) prevention cascade performance and identify implementation barriers for pre-exposure prophylaxis (PrEP) and post-exposure prophylaxis (PEP) among high-risk university students in Sichuan Province, China.
Methods: A cross-sectional survey of 29,017 students across universities in Sichuan Province (November 2022–September 2023) identified 645 high-risk students. Prevention cascades were assessed using a four-stage framework spanning from awareness through service utilization. Multivariable logistic regression models identified predictors of cascade progression.
Results: Among 645 high-risk students (2.22% of surveyed population; mean age 20.36±2.47 years; 66.20% male), only 34.57% achieved high HIV knowledge scores. PEP demonstrated higher awareness than PrEP (83.72% vs. 68.37%), whereas PrEP showed superior understanding conversion (59.41% vs. 52.22%). Utilization rates were comparable (12.87% vs. 13.02%). High HIV knowledge strongly predicted awareness [PrEP: adjusted odds ratio (aOR)=5.62; PEP: aOR=3.42] and PrEP utilization (aOR=1.76). Men who have sex with men (MSM) behavior predicted utilization for both services (PrEP: aOR=2.10; PEP: aOR=1.78). Among students who understood the services, two-thirds did not access them.
Conclusions: High HIV knowledge represents the primary modifiable predictor of cascade progression, yet structural barriers prevent two-thirds of informed students from accessing services. Educational interventions alone are insufficient; comprehensive strategies that simultaneously address both knowledge deficits and systemic barriers are essential for improving service uptake.
-
Human immunodeficiency virus (HIV) incidence among Chinese university students has risen substantially in recent years, with sexual transmission emerging as the predominant route of infection, particularly through male homosexual contact (1). The crude reported rate of HIV/acquired immune deficiency syndrome (AIDS) among out-of-school youth aged 15–24 years in China escalated from 5.25/100,000 in 2010 to 13.75/100,000 in 2020, with epidemic hotspots concentrated in Southwest China, including Sichuan Province (2). Biomedical prevention tools — particularly pre-exposure prophylaxis (PrEP) and post-exposure prophylaxis (PEP) — have demonstrated high efficacy in preventing HIV acquisition, with PrEP reducing sexual transmission risk by up to 99% when taken as prescribed (3–5). However, since China began promoting PrEP and PEP services through demonstration projects in 2019, substantial implementation gaps have persisted despite the proven effectiveness of these interventions (6).
Current evidence from China reveals concerning deficits in prevention uptake among key populations. University students represent a distinct at-risk group with unique behavioral and social characteristics that influence their engagement with HIV prevention services. Understanding where and why students disengage from the prevention cascade is essential for designing effective campus-based programs. Yet, no studies have systematically characterized prevention cascade performance or identified specific barriers to service uptake in this population.
The prevention cascade framework (7-8) provides a systematic approach to identifying specific bottlenecks — from initial awareness through service utilization — that constrain intervention impact. This study addresses these critical knowledge gaps by analyzing prevention cascade performance and distribution patterns for both PrEP and PEP services, identifying modifiable predictors of cascade progression, and quantifying implementation barriers that limit service access among high-risk university students in Sichuan Province.
A cross-sectional survey was conducted across 5 universities in Sichuan Province, China, November 2022–September 2023: Chengdu Technological University, Chengdu Medical College, Chengdu Polytechnic, Sichuan Tourism University, and Southwest Petroleum University. Full-time undergraduate and graduate students were recruited through convenience sampling via peer educator networks, dormitory outreach, and classroom presentations. All participants provided written informed consent prior to enrollment.
High-risk sexual behavior was defined by concurrent fulfillment of two criteria: 1) unprotected sexual intercourse in the preceding 6 months (inconsistent or absent condom use); and 2) at least one behavioral risk factor — either men who have sex with men (MSM) behavior (biological males reporting any male sexual partners, with or without female partners) or multiple sexual partnerships (2 or more partners in the preceding 6 months, regardless of gender or sexual orientation).
Trained student volunteers from each university’s Youth Red Ribbon team administered anonymous questionnaires via secure electronic platforms. The instrument incorporated validated components from China’s National HIV Behavioral Surveillance System, assessing: 1) demographics (age, gender, academic year); 2) sexual behaviors (sexual experience, partner types and numbers, condom use frequency); 3) HIV/AIDS knowledge using a validated 8-item scale (score range 0–8, with scores ≥7 classified as high knowledge); 4) subjective HIV infection risk perception (binary yes/no); and 5) prevention service engagement for PrEP and PEP. Prevention service engagement was assessed using a four-stage cascade framework from population risk exposure through service utilization. For each service, participants were classified into one of four mutually exclusive stages: Stage 1 (unaware) — no awareness of the service; Stage 2 (aware) — aware of the service but lacking understanding of its use; Stage 3 (understand) — understand the service but have not used it; Stage 4 (utilization) — have used the service.
Descriptive statistics were calculated as frequencies with percentages or means with standard deviations. Prevention cascade performance was assessed across four mutually exclusive stages for both PrEP and PEP services, with between-service comparisons performed using χ2 tests. Multivariable logistic regression models identified predictors of PrEP and PEP awareness and utilization. To assess model reliability, we confirmed adequate sample size post-hoc [events-per-variable ratios ranged from 16.6 to 108 across all models, exceeding the recommended minimum of 10 (9)] and evaluated multicollinearity among predictors (all variance inflation factor values ranged from 1.01 to 1.50, well below the threshold of 3.0). Statistical significance was set at P<0.05. All analyses were performed using R version 4.4.2 (R Foundation for Statistical Computing, Vienna, Austria).
Among 29,017 students surveyed across five universities — Chengdu Technological University (4,327 students, 14.91%), Chengdu Medical College (4,351, 14.99%), Chengdu Polytechnic (9,630, 33.19%), Sichuan Tourism University (6,146, 21.18%), and Southwest Petroleum University (4,563, 15.73%) — 3,576 (12.32%) reported sexual experience, 1,640 (5.65%) reported unprotected sexual behavior, and 645 (2.22%) met high-risk criteria. Among these 645 high-risk students, 206 (31.94%) reported MSM behavior and 521 (80.78%) had multiple sexual partners (≥2). Analysis of risk behavior patterns revealed that 439 (68.06%) had multiple partners only, 124 (19.22%) had MSM behavior only, and 82 (12.71%) exhibited both risk behaviors. Only 223 (34.57%) demonstrated high HIV knowledge levels (≥7 points) (Table 1).
Characteristic n (%) or Mean±SD Demographics Age, years 20.36±2.47 Gender Male 427 (66.20) Female 218 (33.80) Academic year Lower year (1st–2nd) 364 (56.43) Upper year (3rd+ and graduate) 281 (43.57) Risk Behaviors MSM 206 (31.94) Multiple sexual partners (≥2) 521 (80.78) Risk behavior patterns Multiple partners only 439 (68.10) MSM behavior only 124 (19.20) Both MSM and multiple partners 82 (12.70) HIV Knowledge and Risk Perception HIV knowledge score (0–8 scale) 5.39±2.02 High HIV knowledge level (≥7 points) 223 (34.57) Perceived HIV infection risk 210 (32.56) Abbreviation: HIV=human immunodeficiency virus; MSM=men who have sex with men. Table 1. Baseline characteristics of high-risk students in universities in Sichuan Province, China, 2022–2023.
Prevention cascade analysis revealed distinct engagement patterns between PrEP and PEP services among the 645 high-risk students (Figure 1 and Table 2). Cumulative cascade metrics demonstrated that PrEP achieved 68.37% (n=441) awareness, 40.62% (n=262) understanding, and 12.87% (n=83) utilization. In comparison, PEP achieved higher rates across all stages: 83.72% (n=540) awareness, 43.72% (n=282) understanding, and 13.02% (n=84) utilization. Stepwise conversion analysis revealed differential performance across cascade stages. PEP demonstrated significantly higher population-to-awareness conversion than PrEP (83.72% vs. 68.37%, χ2=40.87, P<0.05). However, among aware participants, PrEP showed significantly better understanding conversion than PEP (59.41% vs. 52.22%, χ2=4.79, P=0.029). The understanding-to-use conversion rates showed no significant difference between services (31.68% vs. 29.79%, χ2=0.15, P=0.700), resulting in comparable final utilization rates (12.87% vs. 13.02%, χ2=0.00, P=1.000). Implementation gap analysis revealed substantial service underutilization: among participants who achieved understanding, 68.32% (179/262) for PrEP and 70.21% (198/282) for PEP did not access services, with no significant difference between the two interventions (χ2=0.15, P=0.700).
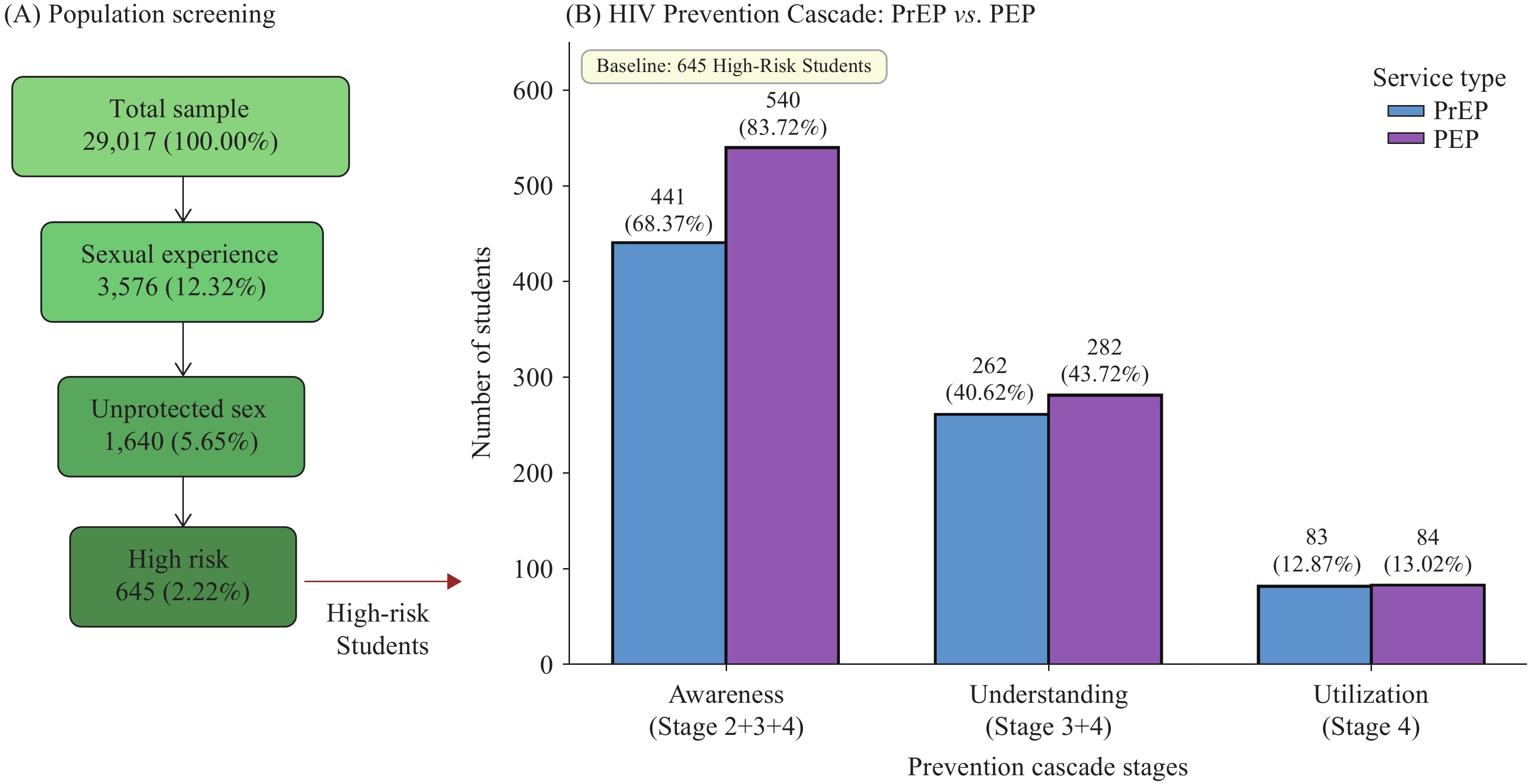 Figure 1.
Figure 1.Study Population and HIV Prevention Cascade Among University Students in Sichuan Province, China. (A) Population screening flowchart illustrating the identification of 645 high-risk students from 29,017 participants. (B) Prevention cascade comparing pre-exposure prophylaxis (PrEP) and post-exposure prophylaxis (PEP) across three cumulative stages: Awareness, Understanding, and Utilization.
Category PrEP n (%) PEP n (%) χ2 P Four-stage distribution Stage 1: Unaware 204 (31.63) 105 (16.28) Stage 2: Aware only 179 (27.75) 258 (40.00) Stage 3: Understand only 179 (27.75) 198 (30.70) Stage 4: Utilization 83 (12.87) 84 (13.02) Cumulative cascade Awareness (Stage 2+3+4) 441 (68.37) 540 (83.72) 40.87 <0.001 Understanding (Stage 3+4) 262 (40.62) 282 (43.72) 1.15 0.284 Utilization (Stage 4) 83 (12.87) 84 (13.02) <0.01 1.000 Stepwise Conversion Rates [% (n/N)] Population → Awareness 68.37 (441/645) 83.72 (540/645) 40.87 <0.001 Awareness → Understanding 59.41 (262/441) 52.22 (282/540) 4.79 0.029 Understanding → Utilization 31.68 (83/262) 29.79 (84/282) 0.15 0.700 Implementation Gap Not using among understanding 68.32 (179/262) 70.21 (198/282) 0.15 0.700 Abbreviation: PrEP=pre-exposure prophylaxis; PEP=post-exposure prophylaxis. Table 2. Prevention cascade performance and statistical comparisons for PrEP and PEP services among high-risk university students (N=645).
High HIV knowledge (≥7 points) emerged as the strongest predictor of awareness outcomes, with students demonstrating substantially increased odds of both PrEP awareness [adjusted odds ratio (aOR) 5.62, 95% confidence interval (CI): 3.90, 8.19, P<0.05] and PEP awareness (aOR=3.42, 95% CI: 2.40, 4.90, P<0.05). High HIV knowledge also significantly predicted PrEP utilization (aOR=1.76, 95% CI: 1.07, 2.87, P<0.05). MSM behavior demonstrated significant associations with service utilization, predicting both PrEP use (aOR=2.10, 95% CI: 1.19, 3.77, P<0.05) and PEP use (aOR=1.78, 95% CI: 1.01, 3.20, P<0.05), though not with awareness outcomes. Upper-year students exhibited significantly lower odds of PrEP awareness relative to lower-year students (aOR=0.59, 95% CI: 0.41, 0.85, P<0.05). Perceived HIV risk demonstrated an inverse association with PrEP awareness (aOR=0.66, 95% CI: 0.45, 0.97, P<0.05). Gender showed no significant association with any cascade outcome (Table 3).
Variable PrEP awareness
aOR (95% CI)PrEP utilization
aOR (95% CI)PEP awareness
aOR (95% CI)PEP utilization
aOR (95% CI)Demographics Male vs. female 1.27 (0.82, 1.98) 1.04 (0.55, 2.01) 0.83 (0.55, 1.25) 0.98 (0.52, 1.84) Upper vs. lower academic year 0.59 (0.41, 0.85)** 0.62 (0.37, 1.01) 0.83 (0.59, 1.15) 0.74 (0.46, 1.20) Knowledge and Risk Perception High vs. low HIV knowledge 5.62 (3.90, 8.19)*** 1.76 (1.07, 2.87)* 3.42 (2.40, 4.90)*** 1.44 (0.88, 2.35) Perceived HIV risk (yes vs. no) 0.66 (0.45, 0.97)* 1.10 (0.66, 1.83) 0.79 (0.55, 1.13) 1.36 (0.83, 2.22) Risk behavior MSM behavior (yes vs. no) 1.34 (0.86, 2.08) 2.10 (1.19, 3.77)* 1.48 (0.98, 2.25) 1.78 (1.01, 3.20)* Note: Model fit statistics: AIC range 487.20–837.27; Nagelkerke pseudo-R² range 0.033–0.246.
Abbreviation: aOR=adjusted odds ratio; CI=confidence interval; PrEP=pre-exposure prophylaxis; PEP=post-exposure prophylaxis; MSM=men who have sex with men.
* P<0.05; ** P<0.01; *** P<0.001.Table 3. Multivariable logistic regression analysis of factors associated with PrEP and PEP awareness and utilization among high-risk university students (N=645).
-
This study represents the first systematic analysis of the HIV prevention cascade among high-risk university students in Sichuan Province, which bears the heaviest HIV burden among Chinese provinces. Our findings reveal two critical gaps: only 34.57% of high-risk students demonstrated adequate HIV-related knowledge, yet among those who understood how to access PrEP and PEP services (40.62% and 43.72%, respectively), approximately 70% failed to utilize them despite engaging in unprotected sexual intercourse. This substantial implementation gap indicates that structural barriers, rather than knowledge deficits alone, constitute the primary constraint limiting prevention cascade effectiveness. The finding is particularly concerning for PEP, which represents the final emergency prevention option following potential HIV exposure. Notably, while service-specific awareness rates were relatively high (68.37% for PrEP and 83.72% for PEP), comprehensive HIV knowledge remained inadequate (only 34.57% achieved ≥7/8 correct answers). This discrepancy suggests that students may recognize these prevention tools without fully comprehending HIV transmission risks or their own vulnerability, underscoring the critical need to integrate PrEP/PEP promotion with comprehensive HIV/AIDS education that emphasizes personal risk assessment.
Recent studies among Chinese university students corroborate this pattern, documenting PrEP awareness rates of 61%–88% alongside utilization rates consistently below 8% (10–11). The 70% implementation gap among students who understand these services represents a critical failure point in the prevention cascade, demonstrating that structural barriers outweigh individual knowledge in determining service access. Systematic reviews have identified several primary barrier categories: high medication costs, confidentiality concerns coupled with fear of HIV status disclosure, multilevel stigma, limited geographic accessibility, and insufficient provider capabilities (12–14). Students who understand PrEP and PEP but fail to utilize them following unprotected sexual intercourse may lack an accurate perception of their own HIV risk, resulting in a diminished perceived need for these services. Consequently, education addressing personal risk awareness is as essential as instruction on service access procedures. The differential effect of knowledge on utilization — statistically significant for PrEP but not for PEP — likely reflects fundamental differences in decision-making processes between these interventions. PrEP requires proactive planning and sustained behavioral commitment, whereas PEP responds to discrete exposure events and may be driven primarily by immediate clinical guidance rather than pre-existing knowledge (4−5).
This study has several limitations that warrant consideration. The convenience sampling approach across five universities within a single province constrains the generalizability of findings to broader student populations. The cross-sectional design prevents establishment of causal relationships between identified factors and cascade outcomes. Additionally, unexpected findings — such as the inverse association between academic year and PrEP awareness — require validation through multi-site longitudinal investigations to determine whether these patterns reflect genuine temporal trends or sampling artifacts.
Analysis of HIV prevention cascades among high-risk university students reveals substantial implementation gaps that extend beyond individual knowledge deficits. Structural barriers — including financial costs, multilevel stigma, and geographic accessibility constraints documented in prior research — constitute the primary obstacles limiting service uptake. Effective cascade optimization requires integrated multi-level strategies that simultaneously address individual knowledge gaps through comprehensive education, interpersonal stigma through peer-led interventions, and systemic barriers through policy reforms ensuring both affordability and accessibility of prevention services.
-
Approval by the Ethics Committee of the National Center for AIDS/STD Control and Prevention, Chinese Center for Disease Control and Prevention (approval number: X221109714).
-
We extend our gratitude to all participating students and staff members from universities across Sichuan Province for their invaluable support and contributions to this research.
HTML
| Citation: |



 Download:
Download:




