-
Introduction: To evaluate the efficiency and effectiveness of Volunteer-Based Social Network human immunodeficiency virus (HIV) Testing Services (VBSNS).
Methods: Collaborating with a local non-governmental organization, we recruited eligible elderly men who have sex with men (MSM) between 2021 and 2024. Participants were assigned to either the traditional Community-Based HIV Testing Services (CBHTS) group or the VBSNS group. We conducted questionnaire surveys, HIV and syphilis antibody rapid testing.
Results: We recruited 144 volunteers, each of whom facilitated HIV testing for 9.13 participants on average. VBSNS accounted for 47.9% of all HIV tests and covered 66.6% of suburban areas. It also accounted for 67.2% of all newly reported cases, compared to only 32.8% for CBHTS. A higher proportion of testers who were under age 60, single, married, or cohabiting, with an education level of below junior college participated in VBSNS. Conversely, a smaller proportion of VBSNS participants reported identifying as homosexual, practiced HIV prevention measures beyond condom use, and had received HIV testing.
Conclusions: VBSNS effectively increased HIV testing uptake and new case identification among MSM in remote areas, successfully reaching a high-risk population. This model provides a valuable alternative for settings where traditional methods such as on-site testing and counseling are inaccessible.
-
According to estimates by the Joint United Nations Programme on human immunodeficiency virus/acquired immune deficiency syndrome (HIV/AIDS) (UNAIDS), the number of people aged 50 and above living with HIV has risen significantly over the last 10 years (1). In China, a similar upward trend has been observed, with newly diagnosed HIV cases among those aged 50 and above increasing from 32,850 in 2015 to 51,856 in 2022 (2). Of these cases, 11.04% were attributed to male-to-male sexual contact, a proportion that has been consistently increasing (3). Tianjin, the second-largest city in Northern China, serves as a key regional center for inter-provincial trade. The city’s HIV epidemic is largely driven by transmission among men who have sex with men (MSM). In Tianjin, MSM aged 50 and above had the highest prevalence of any age group: 7.29% (4). However, only 38.18% have ever been tested for HIV (5). Key barriers to testing include limited awareness, fears of confidentiality breaches, and limited accessibility of testing services (6). This low testing coverage poses several significant challenges. First, individuals in this age group who are diagnosed with HIV often present at a late stage. This late diagnosis, compounded by age-related declines in immune function, significantly increases the risk of HIV-related mortality. Second, many MSM over 50 were in heterosexual marriages, elevating the risk of HIV transmission to their female spouses (7). Since 2021, Tianjin Center for Disease Control and Prevention (CDC) has cooperated with a local non-governmental organization (NGO), the Tianjin Shen Lan Public Health Consulting Service Center (hereinafter, “Shen Lan NGO”), to implement an on-site HIV testing and counseling program targeted at the MSM community. Shen Lan NGO recruits MSM through online and offline methods and provides free HIV testing and counseling services. Nevertheless, the Community-Based HIV Testing Services (CBHTS) remain concentrated in central urban districts, with limited availability in suburban areas.
From January 2021 to December 2024, Tianjin CDC has applied the Volunteer-Based Social Network Strategy for HIV Testing Services (VBSNS) to assess its impact on HIV testing rates in MSM aged 50 and above, compared to standard CBHTS. The social network strategy (SNS) recommended by the World Health Organization (WHO) for HIV testing trains individuals living with HIV or from high-risk populations to encourage their peers to seek voluntary testing (8). Multiple studies have demonstrated the effectiveness of this strategy (9–10). Its primary strength consists in the volunteers’ use of pre-existing social networks and community trust to increase HIV testing uptake among MSM.
Volunteers were recruited through WeChat Moments posts shared by the Shen Lan NGO staff, which allowed MSM individuals to register. The inclusion criteria for volunteers were as follows: aged 18 years or older; had condomless anal sex in the past six months; had a history of new psychoactive substance (NPS) use; and had an HIV-negative result in the most recent HIV test. The training curriculum covered HIV prevention strategies, interpersonal counseling skills, instructions on the use of HIV self-testing kits, and guidelines on maintaining confidentiality. After the training, volunteers who successfully passed the assessments participated in HIV testing outreach and promotional activities. They identified potential participants within their own social networks, such as friends, relatives, or sexual partners, through both online and offline channels. The inclusion criteria for participants were as follows: biological male sex and aged 50 years or above; engagement in anal intercourse with at least one male partner in the past six months; willingness to provide informed consent, complete the study questionnaire, and undergo blood collection for HIV testing; and capacity for independent decision-making and no clinical diagnosis of a mental health disorder. For participants who consented to testing, volunteers provided assistance in conducting HIV self-testing at offsite locations chosen for their convenience, such as public parks, entertainment venues, or private vehicles. Rapid testing for both HIV and syphilis was administered using the HIV 1+2 Antibody Test Kit and the Treponema pallidum (TP) Antibody Test Kit (Zhongxin Keju Biological Pharmaceutical Co., China). Participants were not permitted to undergo repeat testing within a three-month period. Following the HIV test, volunteers administered a digital survey to collect demographic and sexual behavior information. Upon survey completion, an automatic text alert was sent to full-time staff at the Shen Lan NGO, who then reviewed the submission. The process was only finalized after staff verification. Positive screening results were confirmed by Western blot (HIV Blot 2.2, MP Diagnostics, Singapore). Participants with confirmed HIV-positive results were cross-referenced by Tianjin CDC staff via the regional HIV management system. Participants not found in the system were categorized as newly reported cases and were promptly initiated on antiretroviral therapy (ART) (Figure 1).
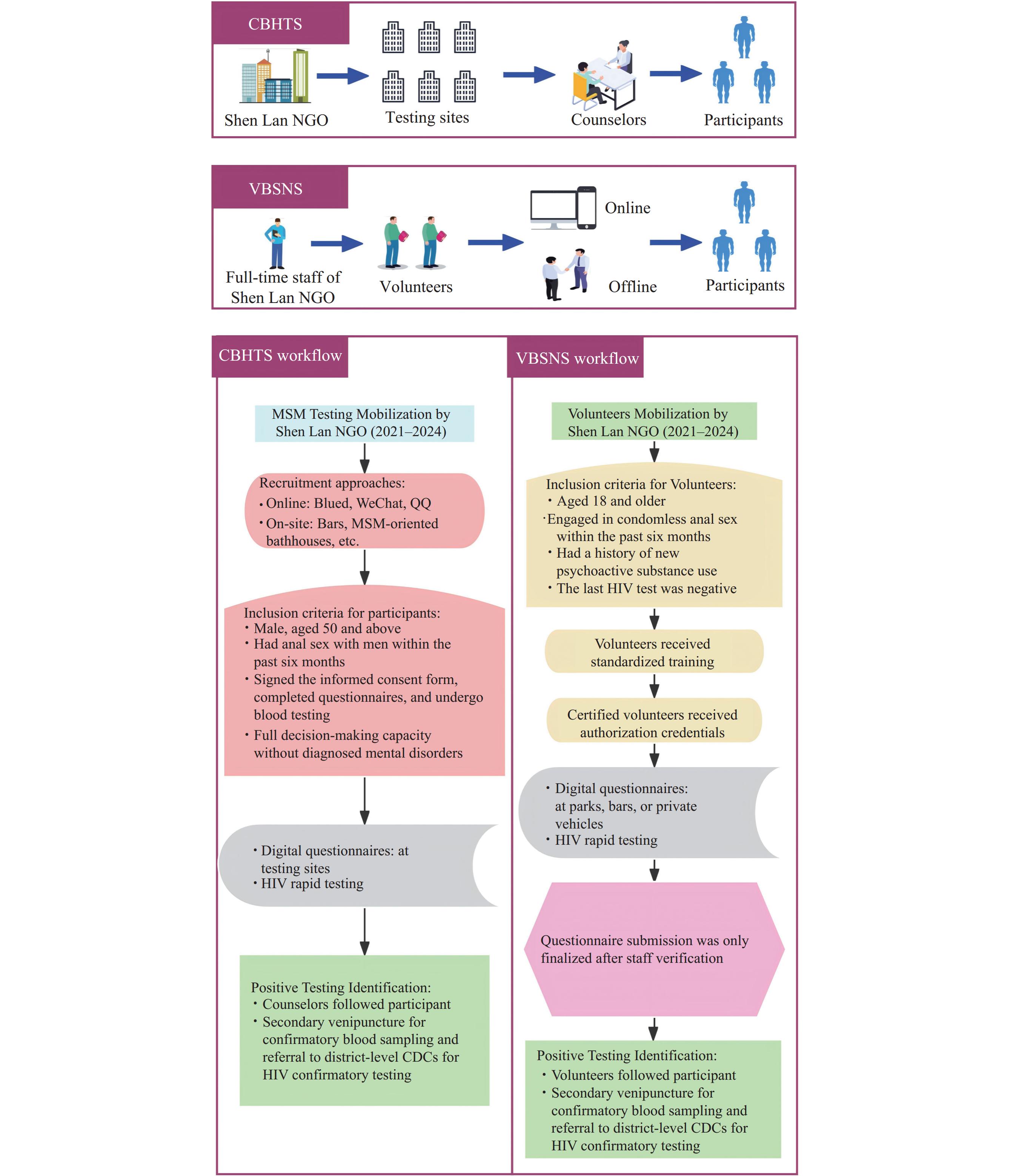 Figure 1.
Figure 1.Overview of HIV testing services via CBHTS and VBSNS.
Abbreviation: HIV=human immunodeficiency virus; CBHTS=community-based HIV testing services; VBSNS=volunteer-based social network HIV testing services.The Shen Lan NGO also established a long-term motivative system for volunteers. This system incorporated various incentives, including performance-based rewards tied to the number of participants recruited and the new HIV-positive cases identified, as well as non-financial recognition. The latter included the regular selection and awarding of “Outstanding Volunteer” certificates, opportunities for skill enhancement and professional growth, and the establishment of a volunteer community to foster a sense of belonging.
During the data statistical analysis, we only used the number of individuals, instead of the total number of tests. All statistical analyses, including two-sided tests with a significance level of P<0.05, were performed using R 4.3.3 software [an open-source software project supported by the R Foundation for Statistical Computing (Vienna, Austria)]. We generated a visual representation of VBSNS testing results from 2021 to 2024 using Gephi software (version 0.10; https://gephi.org/).
In terms of sociodemographic characteristics, most participants tested through VBSNS were under the age of 60, identified as single, married, or cohabiting, and had a college education or less. Regarding behavioral characteristics (for participants with multiple testing, only their most recent questionnaire record was used), the majority identified as homosexual, had HIV prevention methods beyond condom use, and had never been tested for HIV (Figure 2).
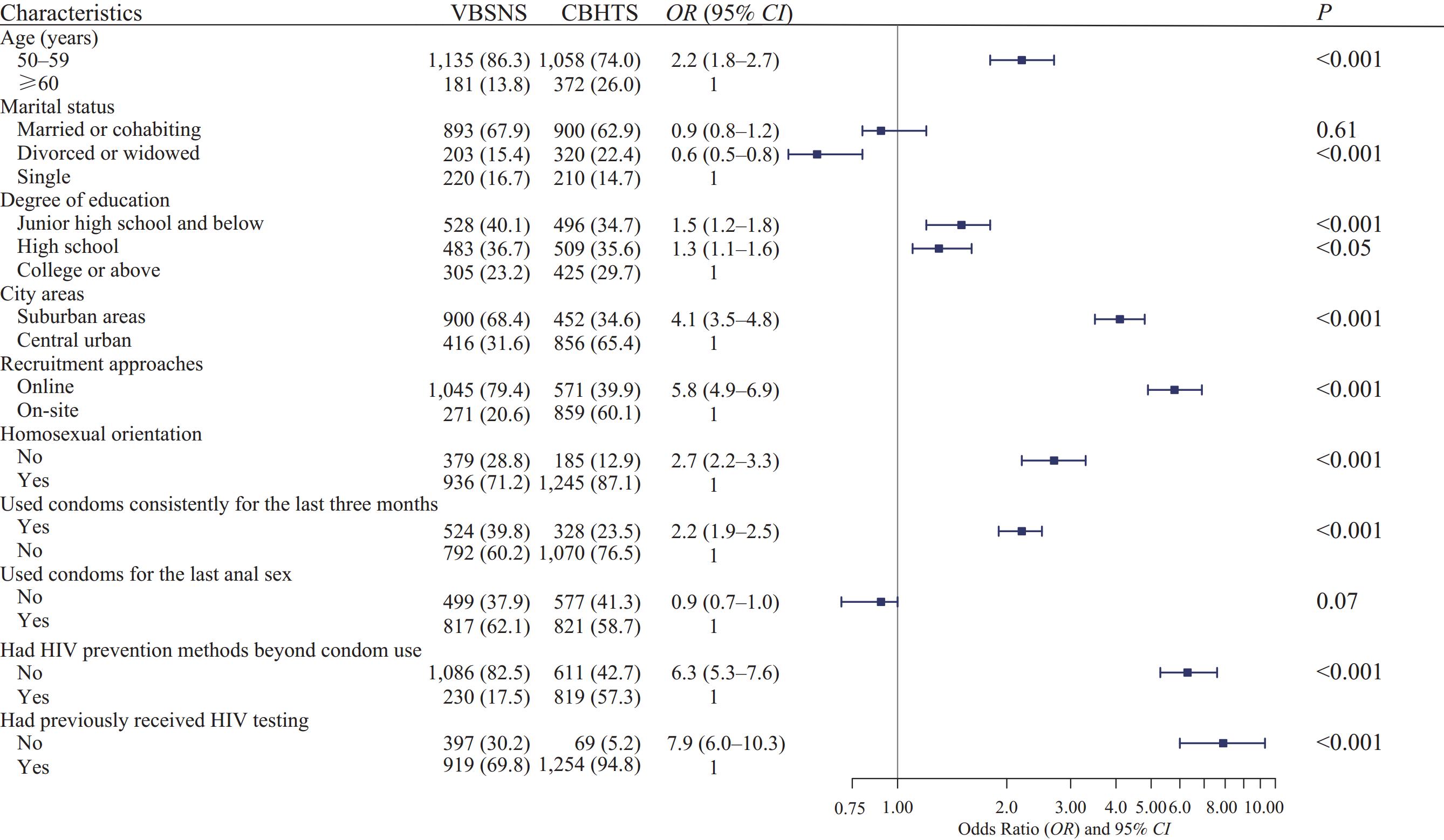 Figure 2.
Figure 2.Sociodemographic and behavioral characteristics of participants in CBHTS and VBSNS.
Abbreviation: CBHTS=community-based HIV testing services; VBSNS=volunteer-based social network HIV testing services.
* P<0.05; ** P<0.01.
For 2021, 2022, 2023, and 2024, VBSNS recruited 64, 53, 72, and 55 volunteers, respectively. Of these, 65 volunteers participated in multiple years, resulting in a total of 144 unique volunteers. On average, each volunteer facilitated testing for 9.1 participants. Each volunteer was assigned a distinct identification number from 001 to 144. Those who conducted 50 or more tests in a given year included volunteers 017, 034, and 107 in 2021; 011, 034, and 107 in 2022; 011, 034, and 091 in 2023; and 011, 034, 055, and 071 in 2024 (Figures 3). A total of 1,316 individuals were tested through VBSNS. The annual number of tests among MSM aged 50 and above was 213, 191, 340, and 572, respectively. In comparison, CBHTS reached 1,430 individuals during the same period, with annual test counts of 313, 124, 357, and 636, respectively. VBSNS accounted for 47.9% of all local tests and conducted 900 tests in suburban areas, representing 66.6% of the total tests conducted in those areas. Among the 10 distant suburban districts, only three reported fewer tests through VBSNS than through CBHTS (Figure 4).
 Figure 3.
Figure 3.Visualization of VBSNS and CBHTS testing between 2021 and 2024. (A) VBSNS: The orange circular with a number represents volunteers who have tested more than 50 people this year, and the thickness of the line is positively correlated with testing frequency. (B) CBHTS: Numbers above the column represent the testing frequency of participants in the testing sites, and percentage numbers indicate the proportion of the testing site’s testing volume in the total testing sites.
Abbreviation: CBHTS=community-based HIV testing services; VBSNS=volunteer-based social network HIV testing services.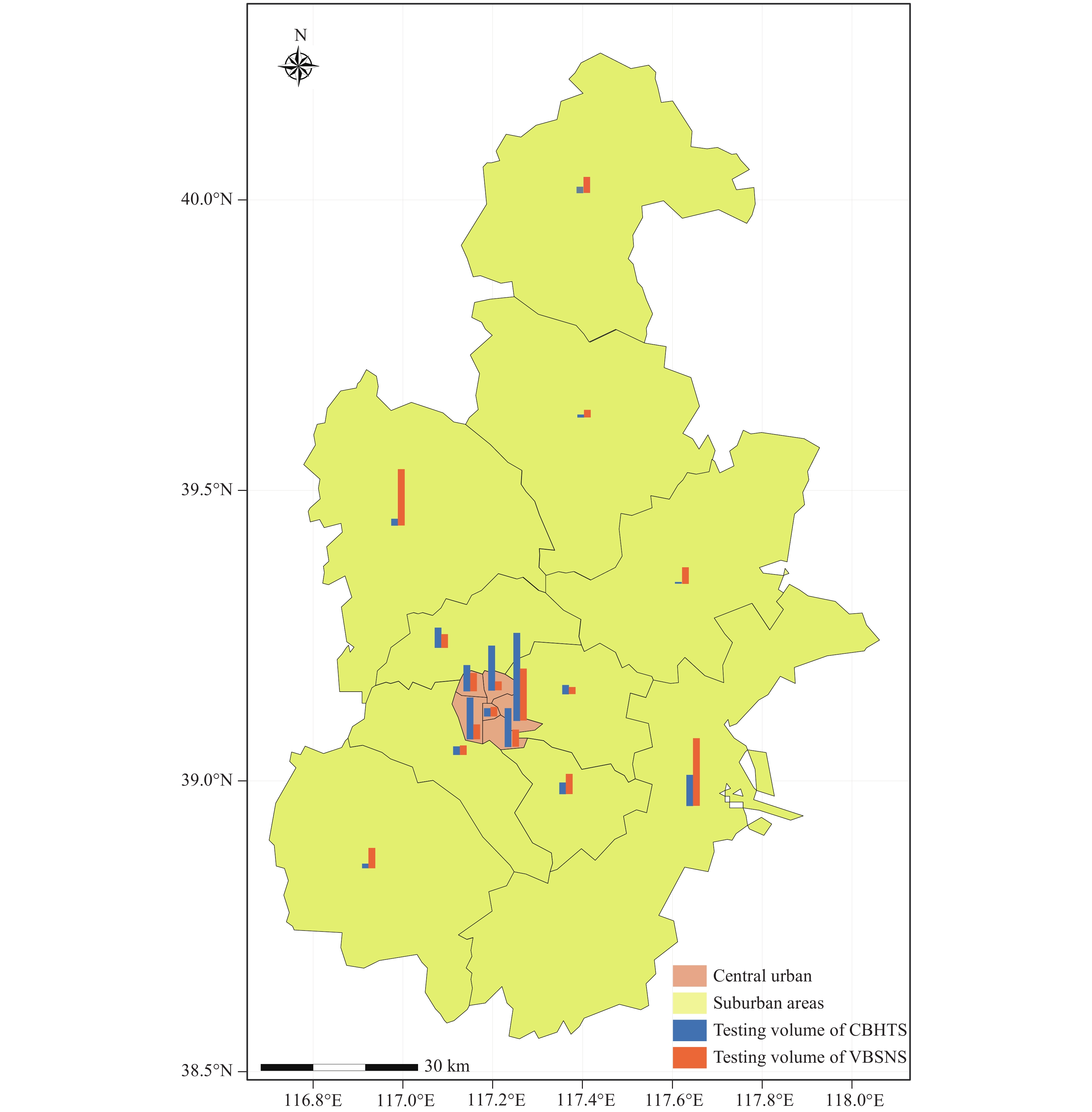 Figure 4.
Figure 4.Map of HIV testing volume in VBSNS and CBHTS.
Abbreviation: CBHTS=community-based HIV testing services; VBSNS=volunteer-based social network HIV testing services; HIV=human immunodeficiency virus.Between 2021 and 2024, 78 newly reported HIV-positive cases were identified through VBSNS, resulting in an HIV-positive rate of 5.9% (78/1,316). The annual positivity rate was 7.2% in 2021, 3.0% in 2022, 3.1% in 2023, and 2.5% in 2024. In comparison, CBHTS identified 38 new cases, yielding a positivity rate of 2.7% (38/1,430); the annual rate was 2.6%, 1.7%, 2.2%, and 1.3%, respectively. VBSNS accounted for 67.2% of all newly reported cases, compared to 32.8% for CBHTS, with annual rates of 69.1%, 66.7%, 55.6%, and 63.6%.
-
The results regarding testing efficiency underscore the significant role of VBSNS in enhancing access to HIV services, especially in under-resourced suburban areas. Notably, VBSNS accounted for 47.9% of the area’s total tests. Its effectiveness was particularly pronounced in remote suburban regions, where it accounted for 66.6% of all tests, markedly exceeding the reach of CBHTS. These findings highlight VBSNS’s advantage in reaching and mobilizing key populations, particularly MSM aged 50 and above.
An analysis of volunteer efficiency under VBSNS reveals that each volunteer conducted an average of 9.2 tests, which exceeds the average of 2.9 tests per volunteer reported in a self-testing kit distribution strategy in Zhuhai and surpasses the 6.7 participants per recruiter documented in U.S.-based social network strategy studies (11–12). A major factor contributing to this outcome is the role of volunteers as “peer motivators,” whose integration within the target community enhances both their reliability and trustworthiness. Additionally, the study identified a group of exceptionally effective “core volunteers” (e.g., 011, 017, 034), each of whom tested more than 50 participants annually. These high-performers played a central role in the success of VBSNS. Therefore, the long-term incentive system for volunteers has proven effective and will be maintained.
In terms of detection effectiveness, a key finding from this study is that VBSNS successfully reached high-risk populations for HIV that are typically difficult for traditional services to cover. VBSNS also identified a significantly higher proportion of newly reported HIV-positive MSM, accounting for 67.2% of all local cases during the study period. The positivity rate for VBSNS was 5.9%, considerably higher than the 2.7% observed for CBHTS. The testing rate among VBSNS participants (69.8%) was comparable to averages for MSM in major Chinese cities such as Shanghai and Qingdao (13) but lower than the 93.1% rate seen in developed countries such as the United States (14). This gap highlights the considerable challenges China faces in expanding testing coverage among elderly MSM, while simultaneously underscoring the potential of alternative strategies such as VBSNS to narrow this gap.
This study has several limitations. First, we identified three districts where testing volumes were lower under VBSNS than under CBHTS. This uneven distribution suggests that the performance of VBSNS may be influenced by local sociocultural factors and the reach of volunteer networks. Future work should conduct focus group discussions or individual interviews to explore the specific challenges faced by volunteers in these areas. Second, when volunteers with low engagement levels dropped out of the program, their social contacts were lost to follow-up testing. Future interventions should strengthen support and training for such volunteers and establish a structured handover system to facilitate the integration of replacements.
Despite its limitations, VBSNS effectively engaged high-risk MSM aged 50 and above, thereby increasing both testing uptake and case identification in remote areas. This model provides a valuable alternative for regions where traditional on-site testing and counseling services are not feasible.
-
Tianjin Center for Disease Control and Prevention, Tianjin Shen Lan Public Health Consulting Service Center, for providing access to volunteers recruitment, training, and technical assistance. We also express our appreciation to Chu Zhou and Maohe Yu for their insightful suggestions and constructive feedback during the preparation of this manuscript.
-
Approval by the Ethics Committee of the Tianjin Center for Disease Control and Prevention (Approval No: TJCDC-R-2023-020).
HTML
| Citation: |



 Download:
Download:




