-
Introduction: Through analysis of a dengue-infected patient presenting symptom 1 day before delivery, this study evaluated the risk of vertical dengue virus transmission through breast feeding. By assessing breastfeeding-associated risks and benefits, this study may inform breastfeeding guidelines for dengue-infected mothers.
Methods: Breast milk samples were collected 10, 15, and 22 days after onset. Field epidemiological investigations and comprehensive laboratory analyses of blood and breast milk samples were conducted, followed by whole-genome viral sequencing using nanopore technology.
Results: Within 10 days of disease onset, dengue virus RNA, NS1 antigen, and IgM in breast milk were all positive (nucleic acid Ct value: 35.58), whereas IgG was negative. Dengue virus RNA, NS1 antigen, and IgG in breast milk were negative on the 15th day of onset, while IgM was negative until the 22nd day of onset. Phylogenetic tree analysis of the whole genome showed that this strain was most closely related to the Guangdong isolate (PP563845.1), with 99.90% homology.
Conclusion: Early breastfeeding by patients with dengue fever during late gestation may pose a risk of viral transmission. Breastfeeding should be cautiously initiated 22 days post-onset only after confirming that both breast milk nucleic acid and IgM have seroconverted to a negative status.
-
Dengue fever is an acute infectious disease caused by the dengue virus. The virus is mainly transmitted by Aedes mosquitoes, making dengue fever a self-limiting disease. While most infections are asymptomatic or cause mild febrile illness, a subset of patients may progress to severe complications, including dengue hemorrhagic fever and dengue shock syndrome (1). The subtropical climate of Guangdong Province fosters optimal conditions for Aedes mosquito proliferation, establishing an ecological foundation for sustained dengue fever transmission. Since Guangzhou’s first case of dengue fever reported in 1978 (2), it has become one of the main epidemic areas in China. Dengue virus includes four serotypes: DENV1 to DENV4 (3).
Although previous studies have elucidated the transmission pathways of dengue fever, research on breast milk as a potential diagnostic specimen remains limited. To address this knowledge gap, this study investigated the risk of vertical dengue virus transmission through the colostrum breast milk of a pregnant woman who developed dengue fever during late gestation. The findings of the study may help refine breastfeeding recommendations for this demographic.
A 35-year-old unemployed Chinese woman, residing with her mother and husband in a city near Guangzhou, presented with a fever (37.8 °C) on November 21, 2024. Her mother and husband had been diagnosed with dengue fever in early November 2024 and received treatment at a local hospital. The patient was hospitalized on November of 22 with a body temperature of 38.9 °C, pulse rate of 136 bpm, respiratory rate of 22 breaths/min, blood pressure of 94/64 mmHg, white blood cell count of 6.66×109/L, and platelet count of 205×109/L, with no apparent rash. An epidemiological investigation revealed that her activities were limited to her residential area 14 days before the symptom onset. Her household had mosquito nets, ornamental plant cultivation and a rooftop vegetable garden, with self-reported frequent mosquito infestations. On the day of hospitalization, the patient underwent an epidural anesthesia-assisted cesarean section to deliver a male infant. Postoperative body temperature fluctuated between 35.8 °C and 39.4 °C, and a chest X-ray ruled out pneumonia.
Breast milk samples were collected 10, 15, and 22 days after onset. Dengue virus testing of maternal blood on November 22 showed positive nucleic acid (nucleic acid Ct value: 24.9) and NS1 antigen, but negative IgM and IgG in the patient. The newborn tested negative for NS1, IgM, and IgG on November 23, and subsequent testing on November 28 revealed negative nucleic acids and NS1, with a clinical presentation of petechiae but no fever. Within 10 days of onset (November 30), dengue virus RNA, NS1 antigen, and IgM in breast milk were all positive (nucleic acid Ct value: 35.58), whereas IgG was negative. Dengue virus RNA, NS1 antigen, and IgG in breast milk were negative on the 15th day of onset (December 5), whereas IgM was negative until the 22nd day of onset (December 12). The patient was discharged on November 28, with follow-up on December 5 showing a white blood cell count of 7.99×109/L and platelets of 471×109/L. Breastfeeding initiation was not suggested for this patient until all breast milk biomarkers yielded laboratory-confirmed negative results (Table 1).
Sampling date Project Sera Breast milk Nucleic acid NS1 IgM IgG Nucleic acid NS1 IgM IgG November 22
(2 days post-onset)Positive
(Ct: 24.9)Positive Negative Negative / / / / November 30
(10 days post-onset)/ / / / Positive
(Ct:35.58)Positive Positive Negative December 5
(15 days post-onset)/ / / / Negative Negative Positive Negative December 12
(22 days post-onset)/ / / / Negative Negative Negative Negative Note: /, No detection. Table 1. Results of dengue virus serological and breast milk tests in mother patient.
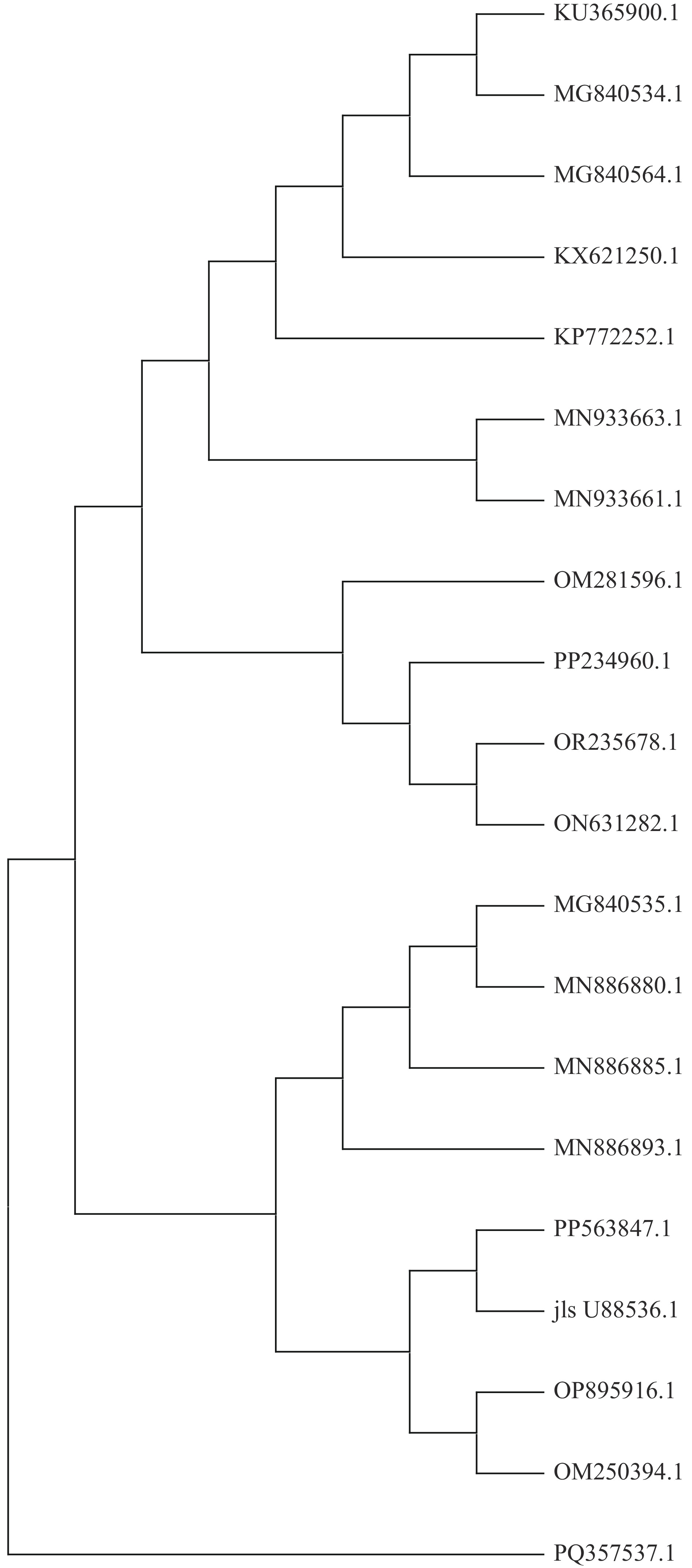
The patient was diagnosed with DENV serotype-1 through dengue viral RNA detection using a reverse transcription-polymerase chain reaction (RT-PCR) assay. Third-generation nanopore sequencing successfully yielded a 10.7 kb viral genomic sequence. BLAST analysis revealed that the nucleotide homology of this strain with the reference (NC001477.1) sequence was 92.46% and exhibited high similarity (99.90%) with the 2023 Guangdong isolate (PP563845.1), with only one amino acid differential site (L617S) in the E protein region of the isolates. Phylogenetic analysis (Figure 1) showed 98.86%–99.90% homology with isolates from Southeast Asian countries, suggesting that this epidemic may be related to imported cases (4-6).
-
To the best of our knowledge, this study documents the first confirmed detection of persistent dengue viral RNA in postpartum breast milk in China, which was identified within 10 days of the onset of maternal symptoms. Our integrated epidemiological and laboratory evidence demonstrates that perinatal dengue infections may pose dual health risks through both vertical transmission and breastfeeding exposure pathways.
Arragain et al. found that the nucleic acid of the dengue virus was present in breast milk; the viral genome was detected in breast milk 1–14 days after disease onset (7). This finding is similar to that of our study, suggesting that breast milk may be a potential route of neonatal infection. Barthel et al. reported a case of vertical transmission of dengue fever; the virus was detected in continuous blood samples from the mother and infant as well as in breast milk, raising concerns about the risk of transmission of dengue fever to newborns during breastfeeding (8). Wang et al. demonstrated that while newborns infected with dengue fever in late gestation may not show severe manifestations of dengue hemorrhagic fever, there is still a risk of vertical transmission of the dengue virus (9). It has been reported that in cases of vertical transmission, maternal infection can lead to viremia, resulting in IgM-positive responses in both mothers and newborns (10). Studies indicate that IgM antibodies against human immunodeficiency viruses, Zika virus, and cytomegalovirus can be transmitted through breast milk, and the persistence of IgM antibodies may pose potential risks to neonates (11).
Biomarker testing revealed that the patient’s breast milk was positive for IgM but negative for IgG on the 10th day post-symptom onset, with persistent IgM positivity observed until day 15, indicating an incomplete or transient immune response following acute infection. The World Health Organization and United Nations Children’s Fund recommend that children initiate breastfeeding within the first hour of birth and be exclusively breastfed for the first 6 months of life (12). Our findings highlight the potential risk of vertical transmission via breastfeeding during the period of detectable dengue viral RNA in breast milk. Based on the case-specific results of this study, breastfeeding should be cautiously initiated 22 days post-onset only after confirming that both breast milk nucleic acids and IgM have seroconverted to negative status, with concurrent verification of infant afebrile status, absence of cutaneous eruptions, and laboratory exclusion of dengue infection. Notably, Lee et al. showed that maternally transferred dengue-specific IgG antibodies via breastfeeding not only extended the disease enhancement window in murine models, but also provided protection against homologous viral challenge (13). The identification of breast milk components that enable neutralizing antibody transfer while facilitating viral transmission provides crucial evidence supporting the need to update breastfeeding recommendations, particularly for convalescent mothers in dengue hyperendemic regions. An early study reported the anti-dengue activity of the lipid components of human milk and colostrum. This suggests that breastfeeding protects infants from the dengue virus in dengue-endemic areas (14).
The findings in this report are subject to at least four limitations. First, direct evidence of vertical transmission through breastfeeding could not be established, because the newborn was not breastfed during the study period and tested negative for the virus. Second, the absence of placental tissue and cord blood samples precluded further investigation of potential transmission mechanisms. Third, the newborn had petechiae but no fever, with negative nucleic acid and NS1; therefore, we did not proceed with further dengue testing for the infant. This presentation may be because severe dengue infections lead to endothelial damage and increased vascular permeability (15). Finally, because this evidence stems from an isolated case report, its generalizability to a broader population remains unclear. Consequently, our findings should be interpreted with caution, and further studies with a more complete sample collection are needed to fully evaluate the risk-benefit ratio of breastfeeding in dengue-infected mothers.
In conclusion, this study revealed that there may be a risk of viral transmission during early breastfeeding for patients infected with dengue fever in late gestation. Based on this individual case, cautious breastfeeding after ruling out clinical symptoms of dengue infection in both mothers and infants may help prevent viral transmission and poor health outcomes. During seasonal transmission periods in dengue-endemic regions, household members of pregnant women exhibiting suspected dengue symptoms should seek immediate medical attention for dengue NS1 antigen testing. Additionally, future breastfeeding guidelines should incorporate biomarker testing to safeguard maternal-infant health.
-
The patient for participating in the study.
-
Approval from the institutional review board of Guangzhou Center for Disease Control and Prevention (No.: [PJ2025004]) on May 28th, 2025.
HTML
| Citation: |



 Download:
Download:




