-
Introduction: On November 27, 2024, an active pulmonary tuberculosis case (pathogen positive) was identified in a senior high school in Guigang City, Guangxi Zhuang Autonomous Region, China.
Methods: A comprehensive field epidemiological investigation was conducted to identify close contacts. Close contacts underwent detailed interviews regarding their exposure history and symptoms, followed by diagnostic testing including the recombinant M. tuberculosis fusion protein test or interferon-γ release assay, along with chest X-ray or CT imaging. Suspected cases were subjected to comprehensive laboratory evaluation, including sputum smear microscopy, sputum culture, and molecular biological testing. Drug susceptibility testing and genomic sequencing analysis were performed on culture-positive strains. Epidemiological associations were systematically assessed.
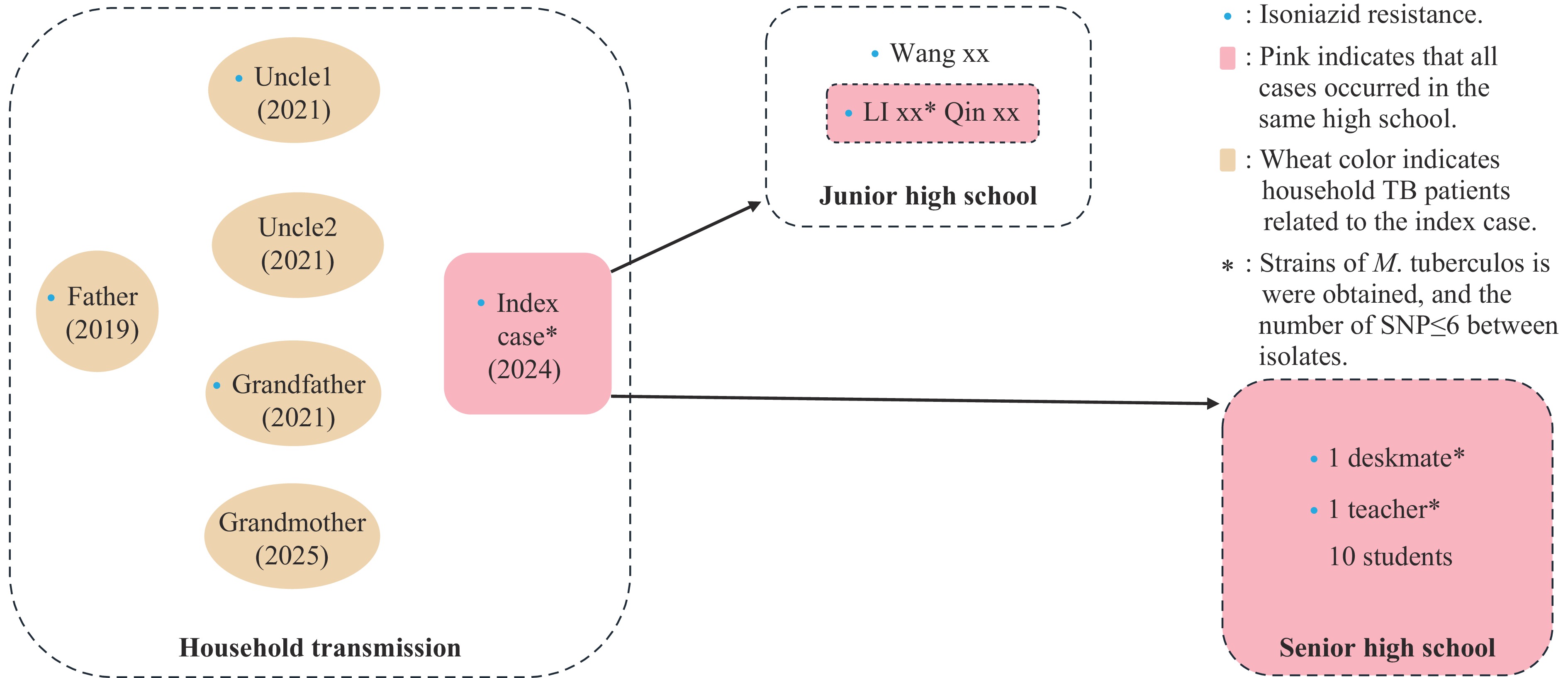
Results: Screening encompassed 957 close contacts (919 from the senior high school and 38 from the index case’s junior high school class). Among these contacts, 18 active pulmonary tuberculosis cases (16 epidemiologically linked and 2 sporadic), 12 suspected cases, and 36 latent tuberculosis infections were identified. Four M. tuberculosis strains were successfully isolated from epidemiologically associated cases (including the index case, his junior high school classmate, high school deskmate, and current teacher). Genomic sequencing revealed that all strains exhibited isoniazid resistance and demonstrated high genetic homology (with <6 single nucleotide polymorphisms, SNPs). The index case had exhibited symptoms including cough and expectoration during junior high school; however, no abnormalities were detected during the physical examination upon senior high school enrollment. Additionally, routine daily health screenings conducted during morning and afternoon periods yielded consistently normal results. The investigation revealed that the index case had significant family contact history, with his father, two uncles, grandfather, and grandmother diagnosed with active pulmonary tuberculosis between 2019 and 2025, three of whom had confirmed isoniazid-resistant tuberculosis.
Conclusion: This outbreak represented a tuberculosis cluster resulting from household transmission that subsequently spread across different school grades and classes. The delayed identification of the index case, attributable to multiple systemic factors, constituted the primary driver of disease dissemination. These findings underscore the critical importance of screening close contacts, particularly those who are teachers or students within affected families.
-
On November 27, 2024, the Qintang CDC in Guigang City of Guangxi Zhuang Autonomous Region received notification from Guigang CDC regarding a severe student pulmonary tuberculosis (PTB) case at a local high school. Preliminary screening conducted by Qintang CDC revealed 26 cases (47.27%) with strongly positive EC (Recombinant Mycobacterium Tuberculosis Fusion Protein) skin test results and 4 cases (7.27%) with abnormal chest X-ray findings. Subsequently, Guangxi Zhuang Autonomous Region (Guangxi) CDC, Guangxi Chest Hospital, and Guangxi Health Supervision Institute launched a joint investigation. Comprehensive screening of 957 close contacts — including 919 individuals from the senior high school and 38 from the junior high school — identified 18 active TB cases, 12 suspected TB cases, and 36 latent TB infections (LTBI). By the conclusion of the previous semester, a total of 22 tuberculosis cases had been confirmed: three cases were reclassified from “suspected” status following additional diagnostic workup, and one case progressed from latent TB infection to active disease. This outbreak, originating from household transmission, spread across both junior and senior high school populations. This report presents the epidemiological investigation and laboratory analysis of this outbreak to inform management strategies for similar future incidents.
-
The outbreak occurred at a boarding high school comprising 51 classes across three grade levels, with a total enrollment of 2,699 students and 215 staff members. Each classroom occupied approximately 64 m2 and accommodated around 55 students, featuring adequate natural ventilation and maintained cleanliness standards. Student dormitories (approximately 24 m2 each) housed 14 residents and were equipped with two electric fans and one air conditioning unit. Each dormitory provided cross-ventilation through doors and windows positioned at opposite ends. Male dormitories lacked private bathrooms, while female dormitories included individual bathroom facilities.
The index case was a 16-year-old underweight male freshman who had experienced chronic productive cough during his junior high school enrollment (Class 55), though this condition received inadequate clinical attention at that time. During the investigation period, he was enrolled as a student in Class 2403 of the senior high school and resided in Dormitory 311. In September 2024, he completed the mandatory freshman entrance physical examination, during which the tuberculin skin test (TST) yielded negative results. On October 17, 2024, he presented to the local community health center with a 3-day history of cough and sputum production. Physical examination revealed bilateral coarse crackles; however, chest radiography was not performed. Daily health screening records maintained by his class documented no abnormal findings from September 1, 2024, through the day preceding symptom onset.
On November 14, 2024, the patient presented to Gangbei District People’s Hospital of Guigang City with a two-month history of recurrent productive cough and fever. Due to disease severity, he was subsequently transferred to Guigang People’s Hospital and then to Nanning Fourth People’s Hospital. Initial evaluations indicated that surgical intervention might be necessary. On November 30, 2024, revised diagnostic imaging revealed secondary pulmonary TB with bilateral involvement: cavitary lesions in the right upper and middle lobes and left upper lobe (newly diagnosed, smear-positive), left-sided tuberculous pleurisy (newly diagnosed, smear-negative), complicated by left hydropneumothorax with approximately 80% compression of left lung parenchyma. Drug-susceptibility testing results provided on December 12, 2024, indicated rifampicin sensitivity but isoniazid resistance (Hr)-TB.
Following the Guidelines for Tuberculosis Prevention and Control in Chinese Schools (2020), Qintang CDC initiated comprehensive case investigation and close contact screening. The investigation revealed that the index case had exhibited prolonged symptoms of cough and sputum production during junior high school, which had not received adequate medical attention. Notably, the index case had a significant family history of TB. His father received an active PTB diagnosis in 2019, followed by his grandfather (2021), two uncles (2021), and grandmother (2025). Among these family members, the father, grandfather, and one uncle were Hr-TB cases (Figure 1).
-
Three rounds of close contact screening were conducted (Table 1). The first-round screening (November 29–December 3, 2024) targeted 66 individuals comprising 52 students and 14 teachers from the index case’s class. The second-round screening (December 3–December 8, 2024) encompassed 405 individuals including 367 students and 38 teachers from adjacent floors and classes. The third-round screening (December 9–December 12, 2024) involved 448 individuals, including contacts from classes taught by the case teacher, the index case’s junior high school classmate Li xx’s class, and dormitory contacts. Screening for class 55 (the class where the index case studied during junior high school) was conducted from December 7th to 20th, 2024. All screening protocols included recombinant M. tuberculosis fusion protein skin test and chest digital radiography (DR), with selected participants undergoing interferon-γ release assay (IGRA) testing and computed tomography (CT) scanning. The first round identified 22 positive individuals (22/66) on skin testing, four with abnormal DR findings (4/66), leading to the detection of four confirmed cases and 17 suspected cases. The second round identified 12 positive individuals (12/405) on skin testing, with no abnormal DR findings; CT re-examinations of these 12 individuals revealed one new clinically diagnosed case and one suspected case. The third round identified nine positive individuals (9/448) on skin testing and one with abnormal DR findings (1/448); CT re-examinations of ten individuals detected two new clinically diagnosed cases (a school security guard and a canteen staff member, with no epidemiological links to the previous cases) and four suspected cases (two students, one canteen staff member, and one convenience-store employee). Concurrent screening of close contacts from the index case’s former junior high school class identified three additional active PTB cases, including Li xx (who studied at the same senior high school as the index case but in a different class, and was confirmed as a PTB case on December 8th), Qin xx, and Wang xx (Figure 1). Following final confirmation by the Guangxi Chest Hospital, a total of 18 confirmed TB cases were identified, including one index case, seven confirmed cases (as referenced earlier), and ten additional cases reclassified from suspected to confirmed status (Table 1). Furthermore, 12 patients were categorized as suspected TB cases.
Screening Class number and location Duration Number of screened cases Number of newly confirmed cases Number of newly suspected cases First-round screening 2403: the index case’s class. 11.29–12.3 66 11: four confirmed cases and 7 reclassified from suspected to confirmed status, 1 teacher and 10 students. 8 Second-round screening 2401, 2402, 2404 and 2405: The same floor;
2316: Up floor;
2406, 2407, 2408, 2409 and 2410: classes of students residing on the same dormitory floor.12.3–12.8 405 1 1 Third-round screening 2419: Li xx’s (the index case’s junior high school classmate) class;
2413: Qin xx’s (the index case’s junior high school classmate) class;
2416, 2417 and 2418: the classes of students residing on the same dormitory floor;
2407, 2409 and 2412: the class taught by the teacher.12.9–12.12 448 2: 2 staff. 3 Other 55: the Junior high school where the index case once studied. 12.7–12.20 38 3: Li xx, Qin xx and Wang xx (the index case’s junior high school classmates) 0 Table 1. The details of close contacts screening.
-
Following the tuberculosis outbreak, relevant agencies launched a coordinated response. The school conducted comprehensive contact tracing and screening of staff and students while implementing tuberculosis prevention education campaigns. Daily health monitoring was intensified, sick-leave data were systematically tracked, and targeted psychological support was provided to students, parents, and staff to address concerns and alleviate fears. The CDC provided technical guidance on screening protocols and containment measures, conducted thorough epidemiological investigations, assisted in identifying close contacts, disseminated evidence-based preventive strategies, and maintained timely communication with all stakeholders regarding outbreak developments. The hospital managed diagnosis, treatment, and follow-up care, and issued medical clearance documentation for safe return to school or work.
Upon comprehensive review and expert panel consultation, 15 students, one teacher, and two other staff members were confirmed as having pulmonary tuberculosis, along with 48 suspected and latent infection cases. Among confirmed cases, six were etiologically positive. All confirmed pulmonary tuberculosis cases received either home isolation treatment or hospitalization based on clinical severity. Of the suspected and latent tuberculosis infection cases, two required hospitalization (meeting established hospitalization criteria) and 16 received preventive treatment. By the end of the previous semester, three cases had transitioned from suspected to confirmed tuberculosis patients, one case had progressed from latent infection undergoing preventive treatment to active tuberculosis, and the remaining cases continued under follow-up monitoring or preventive treatment protocols. The confirmed patients were distributed across classes 2403, 2402, 2413, and 2419, involving boys’ dormitories 311, 312, and 406, as well as girls’ dormitories 408, 406, and 509. Four strains of M. tuberculosis were successfully isolated during this outbreak, including strains from the index patient and epidemiologically linked cases from junior high school. Drug susceptibility testing revealed that all four isolates demonstrated isoniazid resistance. Whole-genome sequencing demonstrated ≤6 single nucleotide polymorphisms (SNPs) between isolates, and genotype analysis confirmed that all strains belonged to the Beijing genotype.
-
Tuberculosis control in schools represents a critical public health priority in China; however, outbreaks continue to pose significant challenges. From 2008 to 2018, the reported incidence rate of TB among students was approximately one-third to one-fourth that of the general population, exhibiting an initial decline followed by an upward trend (1). The rate declined from 27.92 per 100,000 population in 2008 to 13.30 per 100,000 in 2015, then gradually increased to 17.97 per 100,000 in 2018 (1). The reported TB incidence among students was highest in the western region and lowest in the eastern region (2). The outbreak described in this study occurred in Guangxi, a province in southwest China with a reported TB incidence rate of 67.54 per 100,000 in 2023.
Tuberculosis outbreaks typically occur among individuals living in close-contact environments, with schools being common sites of transmission. Outbreaks usually occur within the same class or dormitory. However, this outbreak exhibited distinct epidemiological characteristics and demonstrated high clustering patterns. With the exception of two staff members, all PTB cases were epidemiologically linked, indicating that this represented a cross-household, cross-school-grade, cross-junior/senior-high-school clustered outbreak. In this outbreak, five cases were Hr-TB. Although the management of isoniazid-resistant tuberculosis and drug-sensitive tuberculosis during an outbreak follows similar protocols, their treatment regimens and public health implications differ substantially. Compared with drug-sensitive tuberculosis patients, patients with Hr-TB demonstrate higher treatment failure rates (11% vs. 1%), higher recurrence rates (10% vs. 5%), and higher rates of acquired resistance (8% vs. 0.3%) (3). Molecular epidemiological studies have been widely utilized in contact tracing to understand person-to-person transmission patterns. Spacer oligonucleotide typing (spoligotyping) and MIRU-VNTR typing (mycobacterial interspersed repetitive units-variable number of tandem repeats) are commonly employed typing methods, but they are unsuitable for confirming transmission events in China, due to their limited ability to identify transmission chains in most TB outbreak scenarios. Several studies have demonstrated the utility of whole-genome sequencing (WGS) in epidemiological investigations and have suggested that WGS offers superior discriminatory power compared to spoligotyping and VNTR typing (4-6). In this outbreak, we employed WGS in our epidemiological investigation and demonstrated extremely high genetic similarity (<6 SNPs) between isolates. These results provided evidence that transmission may have begun during junior high school and originated from a single recent transmission source. However, it remains impossible to accurately determine the onset time of the identified cases, and thus the exact transmission chain cannot be definitively established. Based on epidemiological associations and the WGS results, we conclude that the primary transmission chain of this outbreak most likely originated within a household and subsequently spread from the index case to close contacts, including classmates, roommates, and the teacher. The remaining two cases, involving school staff, showed no obvious epidemiological links with the aforementioned 16 cases and may represent independent infections from other sources. As no bacterial isolates were obtained from these cases, further molecular analysis was not possible.
LTBI represents a persistent immune response to M. tuberculosis infection without clinical manifestations or radiological evidence of active disease (7). Approximately 23% of the global population harbors LTBI. Among infected individuals, 5% to 10% will progress to active tuberculosis during their lifetime. Given the substantial prevalence of LTBI, even a modest progression rate to active disease could significantly impact tuberculosis control efforts. Consequently, preventive treatment was administered to selected cases in this outbreak.
The fusion protein skin test or tuberculin skin test serves as a standard screening method; however, false-negative results may occur in certain cases. This limitation may have contributed to the failure to detect the index patient during school enrollment screening. Furthermore, multiple additional factors likely contributed to this public health emergency. First, the diagnosis of the index case experienced significant delay. Second, daily symptom monitoring and student absenteeism tracking failed to identify symptomatic students. This outbreak underscores the critical importance of household contact screening, particularly when household members include students or teachers. Simultaneously, the outbreak has highlighted the need to enhance the quality and effectiveness of freshman entrance physical examinations. Essential routine practices such as monitoring and documenting illness-related absenteeism, conducting daily morning and afternoon health screenings, and providing comprehensive health education require strengthening and standardization.
-
Mr. Canyou Zhang (China CDC), Ms. Hui Chen (China CDC), Ms. Shan Yu (Chinese PLA General Hospital), and Dr. Zhijun Li (U.S. CDC China Office) for their valuable contributions to this investigation.
HTML
Description of Index Case and Epidemiological Investigation
Expanded Screening
Outbreak Control and Treatment Outcomes
| Citation: |



 Download:
Download:




