-
Life expectancy (LE) is a key indicator for comprehensively evaluating population health status and healthcare service quality. With the increasing accessibility and optimization of antiretroviral therapy (ART) worldwide, mortality rates among human immunodeficiency virus (HIV)-infected patients have declined significantly, with their LE gradually approaching that of the general population (1-2). Recent studies have further identified that increasing LE contributes to HIV population aging. In China, ART coverage reached 92.8% by 2022, with all-cause mortality decreasing to 2.7% (3). However, comprehensive analyses of LE among Chinese HIV-infected patients remain scarce. Based on data from China’s nationwide ART cohort, we conducted a continuous cross-sectional study analyzing changes in LE among HIV-infected patients receiving ART in China from 2013 to 2023. Our findings revealed that LE at age 20 years increased from 30.2 years in 2013 to 45.7 years in 2023, though with significant variations across different subpopulations. This study provides vital evidence of improved health outcomes for the HIV population.
All data in this study were derived from the Chinese National Free ART Program (NFATP) database, which contains comprehensive information on all HIV-infected patients receiving ART in Chinese mainland. We implemented a multiple cross-sectional design examining patients who received ART from January 1, 2013 to December 31, 2023 and who initiated treatment at age 15 years or older. Data extraction occurred on June 30, 2024 to account for reporting delays in death records. Following established methodologies in international literature (1), we constructed abridged life tables using the Chiang method to estimate LE at ages 20 and 50 years, with further stratification by sex, baseline CD4 cell count, transmission route, and geographical region (eastern, central, and western) (4). Age-specific mortality rates were calculated using total deaths in a given year as the numerator and half the sum of survivors at the beginning and end of that year as the denominator. We employed joinpoint regression with natural log-transformed rates to examine temporal trends in LE, computing annual percentage changes (APCs) and average annual percentage changes (AAPCs). Additionally, we estimated the contribution of changes in age-specific mortality to longitudinal gains in LE from 2013 to 2023 using the Arriaga decomposition method (5). LE data for the general population were derived from the Global Burden of Disease Study 2021 (the latest available reference for LE at ages 20 and 50 years). Statistical analyses were conducted using SAS (version 9.1, SAS Institute Inc., Cary, NC, USA) and the Joinpoint Regression Program (version 4.9.1.0, Statistical Research and Application Branch, National Cancer Institute, Rockville, Maryland, US).
At the beginning of 2013, 183,498 people living with HIV/AIDS were receiving ART in China, with an additional 1,288,634 patients entering the NFATP during 2013–2023. A total of 1,459,173 eligible HIV-infected patients were included in this study. Most participants were male (75.3%) and contracted HIV via heterosexual transmission (67.3%). Baseline CD4+ T cell counts were available for 1,412,873 subjects, with 37.8% having CD4 <200 cells/μL. From 2013 to 2023, the LE of HIV-infected patients receiving ART in China exhibited a consistent upward trend. The LE at age 20 increased from 30.2 years to 45.7 years (2013–2016: APC=7.9%; 2016–2023: APC=2.9%; AAPC=4.4%, P<0.05). This upward trend was less pronounced in older age groups, with LE at age 50 increasing from 16.1 to 22.7 years (2013–2023: APC=3.3%; AAPC=3.3%, P<0.05) (Figure 1). Decomposition analysis revealed that decreased mortality rates across all age groups positively contributed to the increase in LE at age 20 from 2013 to 2023, with the cumulative contribution of the ≥50 years age group accounting for 20.5% of the increased LE (Table 1). Compared to the general population, the LE at age 20 of HIV-infected patients on ART was 26.9 years less in 2013, with this gap narrowing to 14.6 years by 2021 (Figure 1).
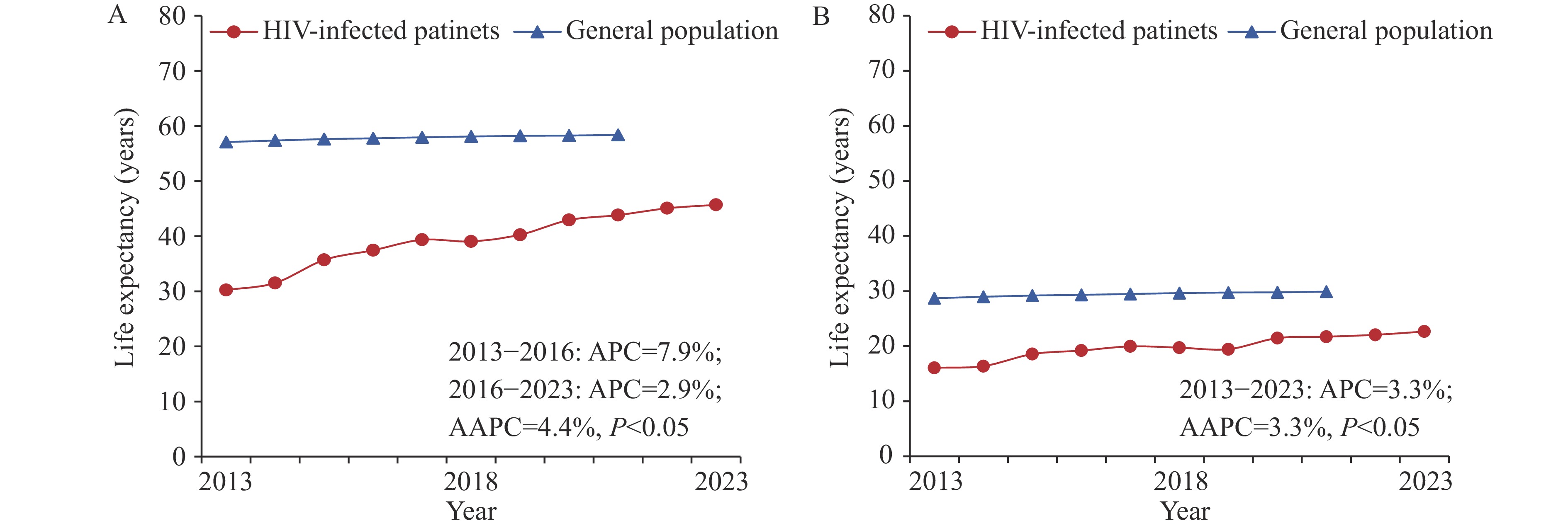 Figure 1.
Figure 1.Life expectancy at age 20 years and at age 50 years for HIV-infected patients receiving ART in China, 2013–2023. (A) Life expectancy at age 20 years; (B) Life expectancy at age 50 years.
Abbreviation: APC=annual percentage changes; AAPC=average annual percentage changes; ART=antiretroviral therapy.Age group
(years)Direct effect Indirect and interaction effect Total effect Contribution (%) 20 0.1 2.3 2.5 15.9 25 0.1 2.1 2.2 14.3 30 0.2 2.3 2.5 16.3 35 0.2 1.9 2.1 13.3 40 0.2 1.6 1.8 11.4 45 0.1 1.1 1.3 8.3 50 0.1 0.7 0.8 5.0 55 0.1 0.6 0.7 4.8 60 0.1 0.4 0.5 3.3 65 0.1 0.4 0.5 3.3 70 0.6 0.0 0.6 4.1 Abbreviation: ART=antiretroviral therapy. Table 1. Contributions of different age groups to life expectancy gains for HIV-infected patients receiving ART in China, between 2013 and 2023.
Persistent differences in LE were observed among ART recipients by sex, baseline CD4 level, HIV transmission group, and geographical region throughout the 2013–2023 period. Sex-specific analyses revealed higher LE for females than males, with the difference in LE at age 20 decreasing from 10.2 years in 2013 to 7.8 years in 2023. When stratified by baseline CD4 levels, the LE gap between patients with CD4 ≥200 cells/μL and those with CD4 <200 cells/μL decreased from 16.4 years in 2013 to 9.5 years in 2023. Transmission route analyses demonstrated that the LE at age 20 for patients contracting HIV via male-to-male sexual contact (2013: 37.5 years; 2023: 55.0 years) was significantly higher than for those who acquired HIV through heterosexual contact (2013: 30.2 years; 2023: 44.0 years), while the lowest LE was observed among patients acquiring HIV through injection drug use (2013: 19.5 years; 2023: 34.1 years). Regional comparisons showed that the gap in LE at age 20 between patients in the eastern region and those in the central region widened from 3.6 to 8.1 years between 2013 and 2023, while the gap between the eastern and western regions increased from 3.2 to 9.7 years during the same period (Figure 2).
 Figure 2.
Figure 2.Life expectancy at age 20 years and at age 50 years for HIV-infected patients receiving ART in China, 2013–2023. (A) LE at age 20 by sex; (B) LE at age 50 by sex; (C) LE at age 20 by CD4 cell count at ART initiation; (D) LE at age 50 by CD4 cell count at ART initiation; (E) LE at age 20 by transmission route; (F) LE at age 50 by transmission route; (G) LE at age 20 by geographical region; (H) LE at age 50 by geographical region.
Abbreviation: HIV=human immunodeficiency virus; ART=antiretroviral therapy; LE=life expectancy. -
To the best of our knowledge, this is the first nationwide study to evaluate the LE of Chinese HIV-infected patients during the past decade. Consistent with international evidence (1–2), the LE of HIV-infected individuals receiving ART has shown a consistent increase from 2013 to 2023, with the gap between HIV patients and the general population narrowing annually. This improvement is largely attributable to China’s comprehensive ART efforts, including expanded treatment coverage, optimized regimens, and enhanced service delivery systems (3). Notably, our findings revealed that LE increases were less pronounced among older patients, suggesting that targeted interventions may be needed to reduce mortality risk in older HIV-infected individuals — a vulnerable population facing compounded health challenges including multimorbidity and age-related frailty.
Our analysis revealed significant disparities in LE among HIV-infected patients in the current ART era. Females demonstrated higher LE than males, which may be attributed to earlier diagnosis through prenatal screening or pregnancy testing, healthier lifestyles, or better treatment adherence (6). However, research findings on gender differences in LE among HIV-infected patients remain inconsistent across settings. While high-income countries show minimal gender differences in LE, low/middle-income countries report substantial disparities, with males initiating ART at age 20 having an LE of 22.9 years compared to 33.0 years for females (7). These variations require further investigation. Additionally, we found that patients with baseline CD4 <200 cells/μL had significantly lower LE than those with CD4 ≥200 cells/μL. Evidence indicates that lower CD4 counts, especially <200 cells/μL, are associated with poor immune recovery, active viral replication, and advanced disease (8). These findings underscore the importance of early detection and prompt ART initiation to maximize treatment benefits and extend LE. Consistent with prior studies, we observed considerable differences in LE across HIV transmission groups. The relatively lower LE among people who inject drugs may be attributed to lower socioeconomic status, poorer lifestyle factors, and reduced access to care — factors that often contrast with the circumstances of men who have sex with men (9). Persistent spatial disparities in LE remain prevalent globally, likely resulting from differences in socioeconomic status, healthcare resource distribution, and population characteristics (1,10).
This study has several limitations. First, due to constraints in routine data collection, potentially influential factors such as socioeconomic status and lifestyle behaviors were not included in our analysis. Additionally, the LE estimates for the general population were derived from the Global Burden of Disease Study rather than from a matched control group, potentially introducing differences in population characteristics. Future research should identify underlying factors contributing to persistent LE disparities among different subpopulations, enabling targeted interventions to improve health outcomes across the HIV-positive population.
HTML
| Citation: |



 Download:
Download:




