-
Resilience has become an attractive and widely discussed concept across multiple disciplines (1). Before evolving into its diverse contemporary applications, resilience originated in 19th-century material sciences as a purely mechanical concept, referring to an object’s elastic recovery capacity and its maximum recoverable deformation after exposure to external forces (2-3). Since the 1970s, fields including ecology (4-5), psychology (6), and sociology (7) have developed discipline-specific understandings of resilience.
As natural disaster frequency has substantially increased in recent decades (8), the international community and disaster management researchers have recognized the importance of reducing natural hazard risks and building disaster resilience (9-12). The concept has become mainstream in addressing complex disaster risk challenges (13). Research on resilience to hazards and disasters has explored a broad range of potential threats and their consequences. While some studies focus on resilience to generic natural hazards, others examine specific hazard types, with meteorological and geological events such as floods, earthquakes, and hurricanes receiving the most attention. Public health crises, however, have received comparatively limited consideration (10,14-15). In these studies, resilience is typically described as a system’s ability to absorb, accommodate, or recover from hazardous events while maintaining acceptable functioning and structure (8-9,16-18). This conceptualization applies particularly to hazards and disasters that are difficult to prevent and cause substantial short-term damage to infrastructure and social systems.
With the increasing threats of emerging infectious diseases (EIDs) since the 21st century, including severe acute respiratory syndrome (SARS), pandemic influenza (H1N1) 2009, Ebola, and the coronavirus disease 2019 (COVID-19) pandemic, resilience has been identified as a critical concept for addressing complex public health crises in countries, communities, and health systems in novel ways (19–20). An increasing number of studies have explored resilience in the context of social systems or health systems facing public health crises (21–29), largely following the understanding of resilience developed for hazards and disasters.
Infectious diseases and outbreaks differ significantly from other natural hazards and disasters in their impact patterns and response processes. Ignoring these differences results in a lack of appropriate resilience concepts for infectious disease outbreaks, which can misdirect attention from key issues in outbreak prevention and control, hindering effective application of the resilience concept. There is an urgent need to develop a specific understanding of resilience applicable to infectious disease outbreaks.
-
We compared the characteristics of infectious diseases and outbreaks with other commonly studied natural hazards and disasters in resilience research, including earthquakes, floods, and tropical cyclones, to illustrate the distinctions between them in several categories (Table 1). According to the crisis life cycle (30), we identified three categories: “prevention and preparedness”, “emergency response”, and “recovery and reconstruction” with nine sub-categories that represent aspects of prevention and response to hazards and disasters.
Categories Sub-categories Hazards characteristics Earthquake (geological) Flood, tropical cyclone (hydro-meteorological) Infectious diseases (biological) Prevention and preparedness Controllability of risk occurrence Uncontrollable Uncontrollable A certain degree of controllability Accuracy of monitoring and warning May not be accurate Relatively accurate Routine outbreaks: relatively accurate; EIDs: inaccurate Time from warning to response A few or tens of seconds Several days A few days or more Emergency response Disaster intervention Unable to intervene Unable to intervene Interventions are key response measures Protection of population and reduction of losses Evacuation, emergency rescue, medical treatment Protective measures in advance, emergency rescue, evacuation, medical treatment NPIs, vaccine development and emergency use, medical treatment, etc. Recovery and reconstruction Impact on people Injuries or loss of life Injuries or loss of life Harmful to health and may cause death Impact on infrastructure May be destructive May be destructive No significant impact on infrastructure Impact on social and economic May cause disruption of social order, economic losses May cause disruption of social order, economic losses Large-scale outbreaks can have some impact on social life and the economy Need for recovery and reconstruction Usually required Usually required May include recovery; reconstruction not required Abbreviation: EIDs=emerging infectious diseases; NPIs=non-pharmaceutical interventions. Table 1. Comparison of infectious diseases with common natural hazards and disasters.
The comparison revealed several key distinctions between infectious diseases and other hazards (8,31-33), indicating that resilience against infectious disease outbreaks should not directly adopt disaster resilience frameworks. First, most natural hazards and disasters cannot be directly intervened in or altered, and losses can only be reduced through preventive preparations before the disaster and rapid rescue afterward (34). In contrast, infectious disease outbreaks allow for a shift from reactive response to proactive measures (33), with key emergency responses focusing on appropriate non-pharmaceutical interventions (NPIs) based on understanding the epidemiology and transmission dynamics to control outbreak spread. Second, disasters caused by natural hazards are often destructive, resulting in substantial infrastructure damage, injuries or loss of life, and disruption of social order and economic systems, requiring significant post-disaster recovery and reconstruction. However, local infectious disease outbreaks can often be managed early through routine prevention and control measures, with limited impact on social life (8,34). Third, while epidemics or pandemics may impact infrastructure and social systems, they are not inherently destructive (35-36), thus eliminating the need for post-disaster infrastructure reconstruction.
-
Based on the similarities and differences between infectious diseases and other hazards, as well as our understanding of resilience to hazards and disasters, we propose several key aspects that should be emphasized to clarify resilience applicable to infectious disease outbreaks. The connections and distinctions between resilience against infectious disease outbreaks and the general understanding of resilience in the field of hazards and disasters have been summarized in Table 2.
Elements Resilience to hazards and disasters Resilience against infectious disease outbreaks Connections Primary sense The ability to withstand external pressures Content Well-prepared, risk identification, remaining functional under extreme stresses, and recovery Distinctions Research scope Regions/social or health systems Including health systems and participants from communities and social systems when the outbreak exceeds the routine level Dimension: core capacity Remaining functional under extreme stresses; recovered and re-established from the effects of hazardous events Proactive response and control; dynamic control strategies adjusted by local capacity and outbreak levels to maintain functions of health systems and social systems Dimension: external pressure Extreme events and disasters that would cause much damage to infrastructure and social systems in the short term Infectious diseases with incubation periods that can escalate to different levels of outbreaks and can be controlled by public health measures. Critical point The limit to remaining functional under extreme stresses The switching point: the critical values of shifting from the condition of daily outbreak response to the emergency response; the resilience threshold: the point at which outbreaks reach the maximum intensity that can be handled within the capacity of an area Table 2. Connections and distinctions between resilience to disasters and resilience against infectious disease outbreaks.
-
While most natural disasters cannot be controlled and occur suddenly with large-scale impacts in a short period, resilience to disasters emphasizes an area’s ability to passively withstand, recover, and reconstruct to minimize socio-economic losses. In contrast, infectious diseases with high epidemic potential typically have incubation periods and transmission processes that allow for a relatively long intervention window after early warning. Measures targeting the source of infections, interrupting transmission routes, and protecting susceptible populations (37) can be implemented according to the transmission patterns and dynamics of infectious diseases to contain outbreaks before they escalate to larger scales and impact communities.
-
An area’s capacity determines the extent of outbreaks it can effectively control. Areas with sufficient resources and strong capacities can manage outbreaks using existing infrastructure for extended periods, while vulnerable areas with capacity limitations require more stringent measures to maintain basic functions and avoid rapidly exceeding local capacity during outbreaks. Resilience against infectious disease outbreaks encompasses multiple capacity dimensions beyond health systems alone. The capacities required differ between daily outbreak response and emergency response conditions. Generally, capacities related to resilience against infectious disease outbreaks include the professional expertise of local disease control and prevention agencies, resource reserves and utilization, surge capacity of health facilities, multisectoral cooperation, and community engagement.
-
Negative impacts on health and social systems can be minimized if interventions are implemented effectively during the early stages of outbreaks. While restoring health facility functions and resuming social activities is necessary once large-scale outbreaks are controlled, this recovery process is relatively rapid compared to recovery from other types of disasters. Furthermore, since outbreaks typically do not cause substantial damage to infrastructure, post-outbreak efforts should focus on addressing weaknesses in health systems to better prepare for and prevent future pandemics, rather than reconstructing buildings and facilities, which is often emphasized in disaster resilience.
-
Building on the aspects that should be emphasized for resilience against infectious disease outbreaks, resilience against infectious disease outbreaks can be defined as the capacity of an area to effectively prevent, detect, respond to, and control outbreaks without seriously affecting essential functions of health and social systems. The largest outbreak intensity that an area can cope with indicates the upper limit of resilience against outbreaks, which can be recognized as the resilience threshold.
The capacity of an area to cope with infectious disease outbreaks determines the maximum degree of outbreaks that the area can withstand, forming the scope of resilience against infectious disease outbreaks. Under the condition of daily outbreak response, the required capacities mainly include the basic skills for disease control and prevention at the local level, timely detection and reporting of infectious disease cases of unknown origin at all levels of healthcare institutions, emergency response planning, resource reserves, and other preparations for epidemics and pandemics. Under the condition of emergency response against a large-scale outbreak exceeding the daily level, advanced professional skills, utilization of redundant resources, and surge capacity of health facilities are required. Once the outbreak level exceeds the capacity of local agencies for disease control, coordination of actors within and outside health systems is often needed in addition to other capacities. Depending on the scale of outbreaks, reflection on lessons learned and continuous improvement of overall capacity are also required once the outbreak is under control.
Since routine outbreaks can be controlled through daily operations by local agencies, building resilience against outbreaks should focus on capacities to control outbreaks that exceed daily levels. These large-scale outbreaks put pressure on local capacity and require emergency response with the utilization of reserved resources. The threshold of resilience against infectious disease outbreaks in an area is likely determined by the weakest critical component of its prevention and control capacity.
Based on the above understandings, resilience against infectious disease outbreaks can be represented by a schematic (Figure 1). The horizontal axis represents the outbreak prevention and control capacity of areas, while the vertical axis represents the intensity of infectious disease outbreaks over time. The capacity of each area determines the upper limit of outbreaks that can be handled in that area, resulting in the corresponding level of resilience. The curve of Resilience thresholds represents the critical values of the maximum intensity of outbreaks that can be handled within the capacity of areas, and the curve of Switching points represents the critical values of shifting from the condition of daily outbreak response to the condition of emergency response in areas. The schematic illustrates a possible changing pattern of resilience against infectious disease outbreaks in areas with different capacities.
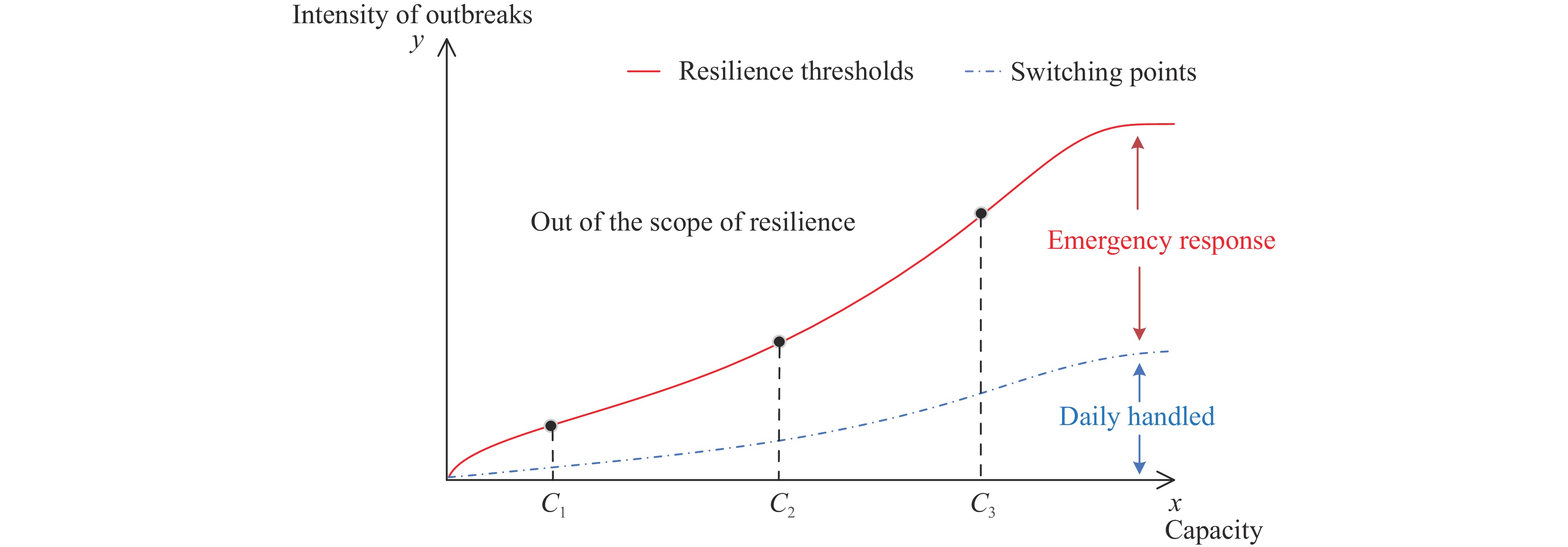 Figure 1.
Figure 1.Schematic of resilience against infectious disease outbreaks.
Note: 1) x is the outbreak prevention and control capacity, and y is the intensity of infectious disease outbreaks over time. Capacity determines the intensity of outbreaks in a certain period that can be handled in an area. 2) The curve of Resilience thresholds represents the critical values of the maximum intensity of outbreaks that can be handled within the capacity of areas, and the curve of Switching points represents the critical values of shifting from the condition of daily outbreak response to the condition of emergency response in areas. C1, C2, and C3 represent regions with different capacity have corresponding levels of resilience thresholds and switching points. -
By inheriting the fundamental understanding of resilience and developing the concept of disaster resilience based on the characteristics of infectious diseases, this study proposes a concept and scope of resilience specifically applicable to infectious disease outbreaks. This framework provides valuable insights for addressing critical issues related to outbreak prevention and control, and can guide preparation and response strategies in different regions, highlighting the importance of resilience in infectious disease management.
The concept of resilience against infectious disease outbreaks proposed in this study focuses on acute infectious diseases that can cause sudden onset and large-scale outbreaks in the short term, regardless of their transmission routes (airborne, vector-borne, direct contact, etc.). Diseases with high transmissibility or virulence, such as SARS, COVID-19, and Ebola, pose the greatest threat to resilience because they can rapidly overwhelm local health systems, leaving insufficient response time. These diseases require comprehensive capacity and redundant resources to prevent epidemics from exceeding the upper limit of local resilience. In July 2024, the WHO launched a pathogens prioritization framework (38) for epidemic and pandemic research preparedness, which can help clarify which diseases should be prioritized to enhance global resilience against epidemics and pandemics, though priorities may differ when adopting a regional perspective.
Our findings provide insights into resilience against infectious disease outbreaks, aligning with the WHO’s recommendation to further explore and understand the application of resilience to various health system challenges (39). The WHO’s recent reports (40-41) define a framework for health system resilience against diseases and other events that is consistent with our overall concept. However, the WHO’s framework encompasses both acute and chronic diseases and provides general capacity requirements for health systems across countries with varying development and economic conditions. In contrast, our concept specifically addresses resilience against acute infectious disease outbreaks and integrates the temporal intensity of outbreaks with the capacity of local health systems and other stakeholders. Additionally, we developed specific capacity elements for resilience against outbreaks primarily in the context of China’s health systems. Similar distinctions exist between our approach and Nuzzo’s study (24). The advantage of this study’s concept is that it considers the dynamic nature of epidemics relative to regional capacities, providing a framework for measuring resilience against infectious disease outbreaks across different areas. Unlike Zhao’s study (42), which measures resilience using indicator system scores, our proposed resilience threshold allows regions to identify specific capacity shortcomings that limit their ability to manage outbreaks, enabling more targeted improvements rather than applying uniform standards across different regions.
Redundancy and resourcefulness are key attributes for pandemic preparedness (43-44) and are recognized as important “means” of resilience to natural hazards and disasters (45-46). Resilience against infectious disease outbreaks should be assessed proactively to ensure adequate redundant resources and appropriate mechanisms for resource utilization and deployment. Based on their resilience capacity, regions can develop and revise contingency plans for outbreaks of varying intensity; authorities and agencies should establish mechanisms for transforming public health strategies and allocating redundant resources to effectively implement interventions that can withstand large-scale outbreaks and potentially long-lasting pandemics.
For infectious disease outbreak prevention and control, the resilience threshold has a unique meaning that differs from the ecological resilience threshold (47-48). It represents the point at which an outbreak reaches the maximum intensity that can be managed within a region’s capacity. When this threshold is exceeded, the outbreak has caused widespread transmission beyond the region’s capacity to control, which can seriously affect health and social systems, resulting in significant costs. Support from other regions and implementation of strict public health and social measures become necessary. Therefore, a region should assess its resilience threshold in advance and take measures to avoid exceeding it during epidemics and pandemics.
In conclusion, resilience requires specific definitions tailored to different fields to be effectively applied. Based on the understanding developed in this study, the exact scope and elements of resilience against infectious disease outbreaks at local and regional scales can be further defined. This will guide regions in implementing appropriate measures for different outbreak levels, achieving overall capacity improvements, and enhancing their sustainability against large-scale outbreaks while better preparing for future pandemics.
-
The authors acknowledge the reviewers for their valuable feedback and constructive suggestions on this paper.
HTML
Comparison Between Infectious Diseases and Natural Hazards
Aspects that Need to Be Emphasized for Resilience Against Infectious Disease Outbreaks
Proactive response and control
Outbreak response strategies should be aligned with local capacities
Rapid recovery and improvement
Concept and Scope of Resilience Against Infectious Disease Outbreaks
Discussion and Conclusions
| Citation: |



 Download:
Download:




