-
Objectives: Human papillomavirus (HPV) is a globally prevalent infection, with multiple genotypes strongly associated with cancers and other diseases. While epidemiological studies in females are extensive, research on HPV genotype distribution in males remains limited.
Methods: We conducted a retrospective study by collecting and analyzing clinical and laboratory data from male patients with confirmed HPV infection at Shenzhen People’s Hospital. The distribution of HPV genotypes and their associations with specific disease types were evaluated.
Results: A total of 2,037 male participants were included, with an overall HPV infection rate of 45%. Low-risk genotypes predominated, with HPV 6 and HPV 11 accounting for 25% and 12% of cases, respectively. High-risk genotypes such as HPV 16 and HPV 52 showed low prevalence (<3%) but exhibited a slight upward trend in 2022. No significant age distribution differences were observed between HPV-positive and HPV-negative groups. The frequency of multiple HPV genotype infections increased slightly with age. Specific HPV genotypes showed unique associations with acne (HPV 56), allergic dermatitis (HPV 59), and amyloidosis (HPV 58).
Conclusions: Low-risk HPV genotypes predominate in males with confirmed exposure. Older males appear more susceptible to multiple infections, and specific genotypes are associated with distinct diseases, supporting the need for male-targeted HPV vaccination and surveillance programs.
-
Human papillomavirus (HPV) is recognized as a leading cause of several diseases, including cervical cancer, anal cancer, penile cancer, oropharyngeal cancer, and genital warts (1–6). Despite significant advances in understanding HPV epidemiology in women, particularly with the widespread implementation of vaccination programs, the prevalence and clinical outcomes of HPV infection in men remain inadequately characterized (7).
HPV infection in men is associated with multiple conditions, including genital warts, anal dysplasia, and oropharyngeal cancer (8–9). However, comprehensive data on the distribution of different HPV genotypes in males, particularly those with confirmed HPV exposure, are limited. This study aims to address this knowledge gap by examining the prevalence of HPV genotypes in a cohort of males with confirmed HPV exposure and investigating their relationship with clinical outcomes.
This study included 3,131 patients who underwent HPV detection at Shenzhen People’s Hospital between September 18, 2018, and October 8, 2022. After excluding patients with incomplete information or unclear diagnoses, 2,037 patients were included in the final analysis. Diagnoses were confirmed by at least two experienced physicians, with the analyzed diseases including warts, amyloidosis, acne, folliculitis, allergic dermatitis, and others.
Patient samples were collected following comprehensive skin examinations of affected areas. Epidermal samples were obtained by scraping the upper epidermis using a scraper or scalpel, or by clipping small tissue pieces with biological tissue forceps. Skin slices were prepared by excising small sections from affected areas, while biopsies were performed using biological tissue forceps or scalpel under local anesthesia. DNA extraction was conducted using a Nucleic Acid Genotyping Kit for Human Papillomavirus (Flow Fluorescence Hybridization Method, Shanghai Tellgen), which detected 27 HPV genotypes, including 17 high-risk types (16, 18, 31, 33, 35, 39, 45, 51, 52, 56, 58, 59, 66, 68, 26, 53, 82) and 10 low-risk types (6, 11, 40, 42, 43, 44, 55, 61, 81, 83) (https://www.tellgen.com/human_papillomavirus/HPV27_pro.htm). The DNA samples were homogenized by vortexing, followed by centrifugation and nucleic acid release, with the supernatant transferred for detection. PCR amplification followed a specific protocol involving initial denaturation, multiple amplification cycles, and final extension. Sequence alignment was performed using the blastn program (10).
This study investigated the prevalence of HPV infection in Shenzhen City, Guangdong Province, China, and analyzed demographic characteristics of participants. From a total of 3,131 male participants enrolled, all with female sexual partners who tested positive for HPV, 2,037 were included in the final analysis after data cleaning. The overall HPV infection rate was 45%. Analysis revealed no significant difference in age distribution between HPV-positive and HPV-negative groups, suggesting that age does not significantly influence HPV infection susceptibility (Figure 1).
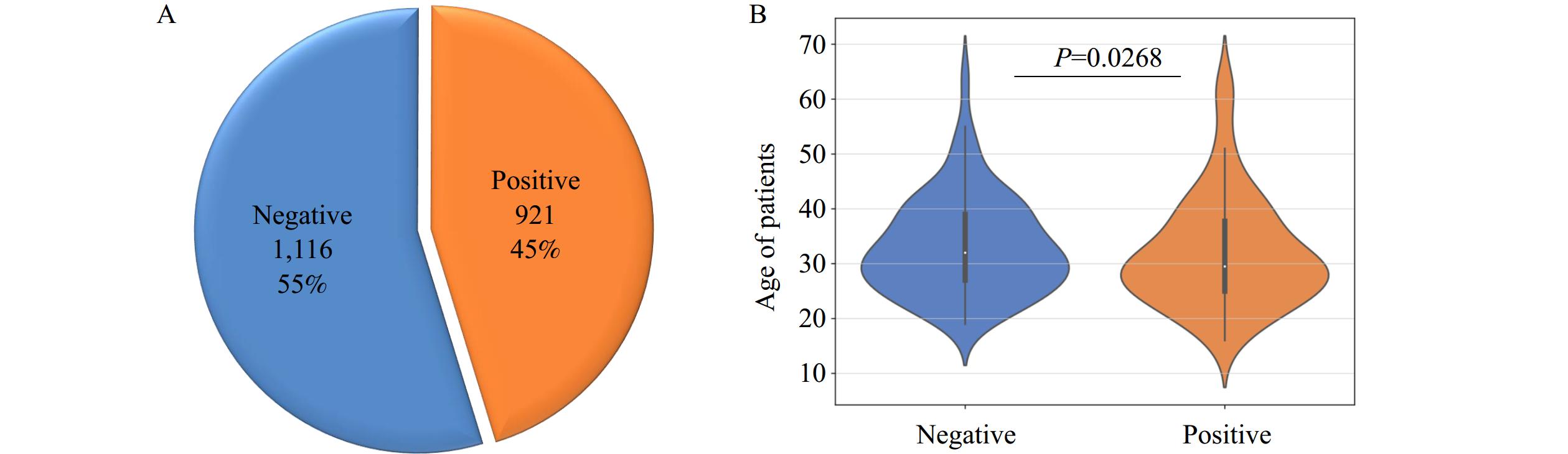 Figure 1.
Figure 1.HPV infection status and age distribution of participants. (A) 45% of the participants showed positive HPV results. (B) There is no significant difference in age distribution between HPV-negative and HPV-positive participants.
Abbreviation: HPV=human papillomavirus.The prevalence of HPV genotypes among males fluctuated throughout the study period (2018–2022). Negative cases increased from 47.99% in 2018 to 61.43% in 2020 before declining to 42.05% in 2022, while positive cases rose from 38.58% in 2020 to 57.95% in 2022. HPV 6 and HPV 11 were the most prevalent genotypes, reaching peaks of 12.92% and 6.82%, respectively. High-risk genotypes such as HPV 16 maintained low prevalence (<3%) but exhibited a slight upward trend in 2022 (Table 1).
Year Negative (%) Positive (%) 6 (%) 11 (%) 16 (%) 39 (%) 43 (%) 44 (%) 53 (%) 66 (%) Other (%) 2018 47.99 52.01 11.07 4.36 3.02 1.34 1.01 0.34 0.00 2.01 31.87 2019 52.54 47.47 12.92 5.36 1.63 0.19 1.05 0.29 0.96 0.29 26.27 2020 61.43 38.58 11.18 4.90 1.51 0.13 0.63 0.25 0.25 0.00 21.99 2021 51.66 48.35 13.72 4.54 1.00 1.00 1.88 0.66 1.00 0.33 27.59 2022 42.05 57.95 7.95 6.82 1.14 2.27 2.27 3.41 2.27 1.14 29.95 Abbreviation: HPV=human papillomavirus. Table 1. Annual distribution of HPV positivity and genotype prevalence in males.
Among HPV-positive participants, 27 distinct HPV genotypes were identified. Low-risk HPV genotypes showed significantly higher cumulative detection rates (47.77%) compared to high-risk types (25.63%) (Figure 2A). Similarly, the average detection rate of low-risk genotypes (3.18%) exceeded that of high-risk types (2.14%) (Figure 2B). Among low-risk types, the five most frequently detected genotypes were HPV 6 (25%), HPV 11 (12%), HPV 53 (6%), HPV 43 (6%), and HPV 59 (6%) (Figure 2C). For high-risk types, the most prevalent genotypes were HPV 52 (6%), HPV 16 (6%), HPV 51 (6%), HPV 39 (4%), and HPV 59 (3%) (Figure 2C). Further analysis clearly demonstrated the predominance of low-risk HPV genotypes among positive participants (Figure 2D).
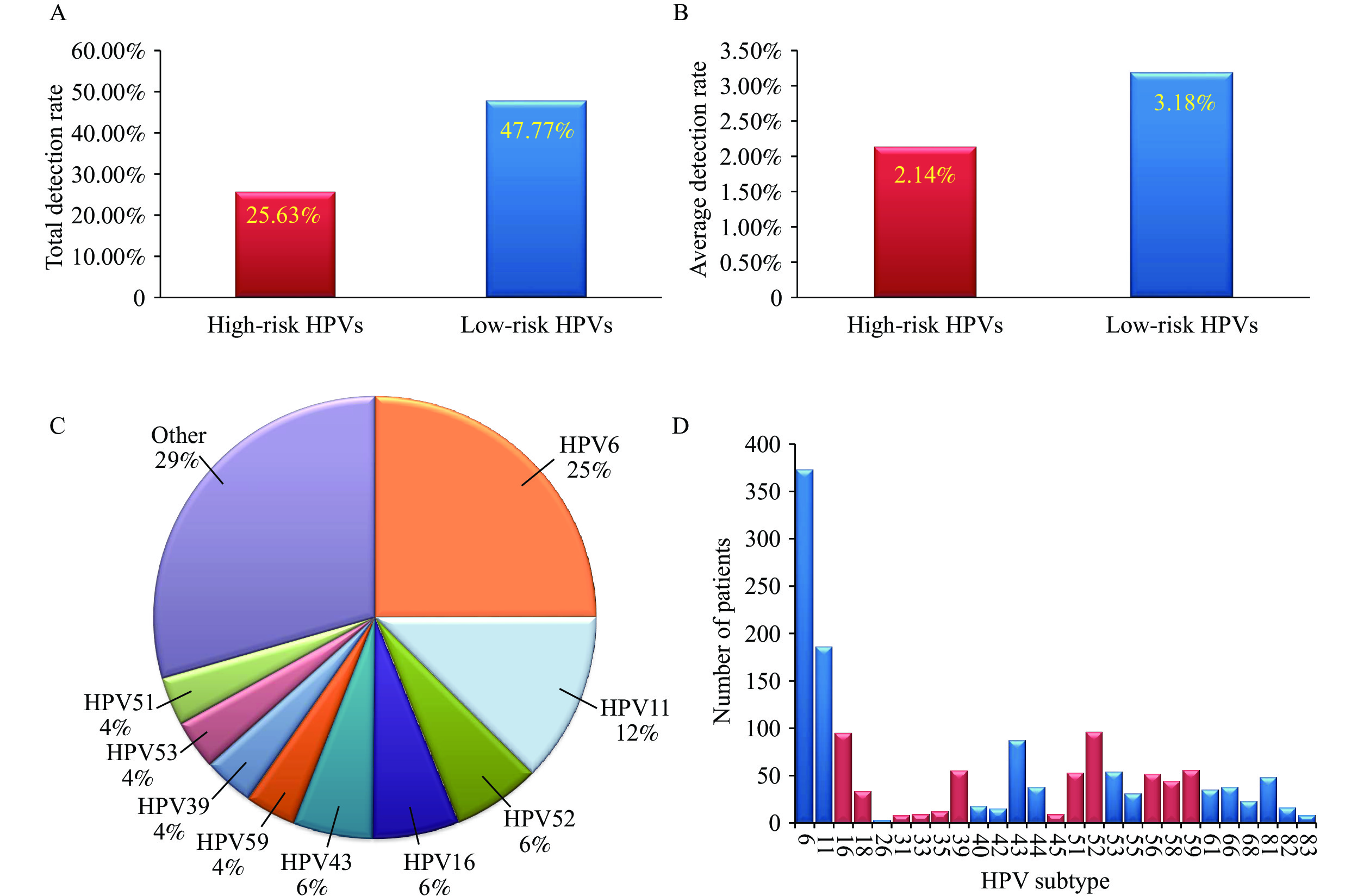 Figure 2.
Figure 2.Detection rates and genotype distribution of high-risk and low-risk HPV genotypes. (A) Total detection rate of high-risk and low-risk HPV genotypes. (B) Average detection rate of high-risk and low-risk HPV genotypes. (C) Proportion of each HPV genotype among HPV-positive participants. (D) Distribution of high-risk and low-risk HPV genotypes among positive participants.
Note: For (D), The histograms show the distribution of high-risk (blue) and low-risk (red) HPV genotypes among positive participants.
Abbreviation: HPV=human papillomavirus.
Significant variations were observed in the distribution of high-risk HPV genotypes among the male population. HPV 16 and HPV 52 exhibited the highest prevalence (18% each), followed by HPV 39 and HPV 59 (11% each), while other genotypes including HPV 18, 51, and 56 showed relatively lower prevalence (Figure 3A). Age distribution analysis revealed that HPV 16 and HPV 18 infections were more common in younger individuals, whereas HPV 52, 59, and 39 were detected across a broader age range, including older individuals, suggesting genotype-specific age patterns (Figure 3B). Further analysis of the relationship between age and multiple genotype infections revealed a gradual increase in the number of genotypes detected with increasing age, indicating a weak positive correlation and suggesting that older males may be more susceptible to multiple HPV genotype co-infections (Figure 3C).
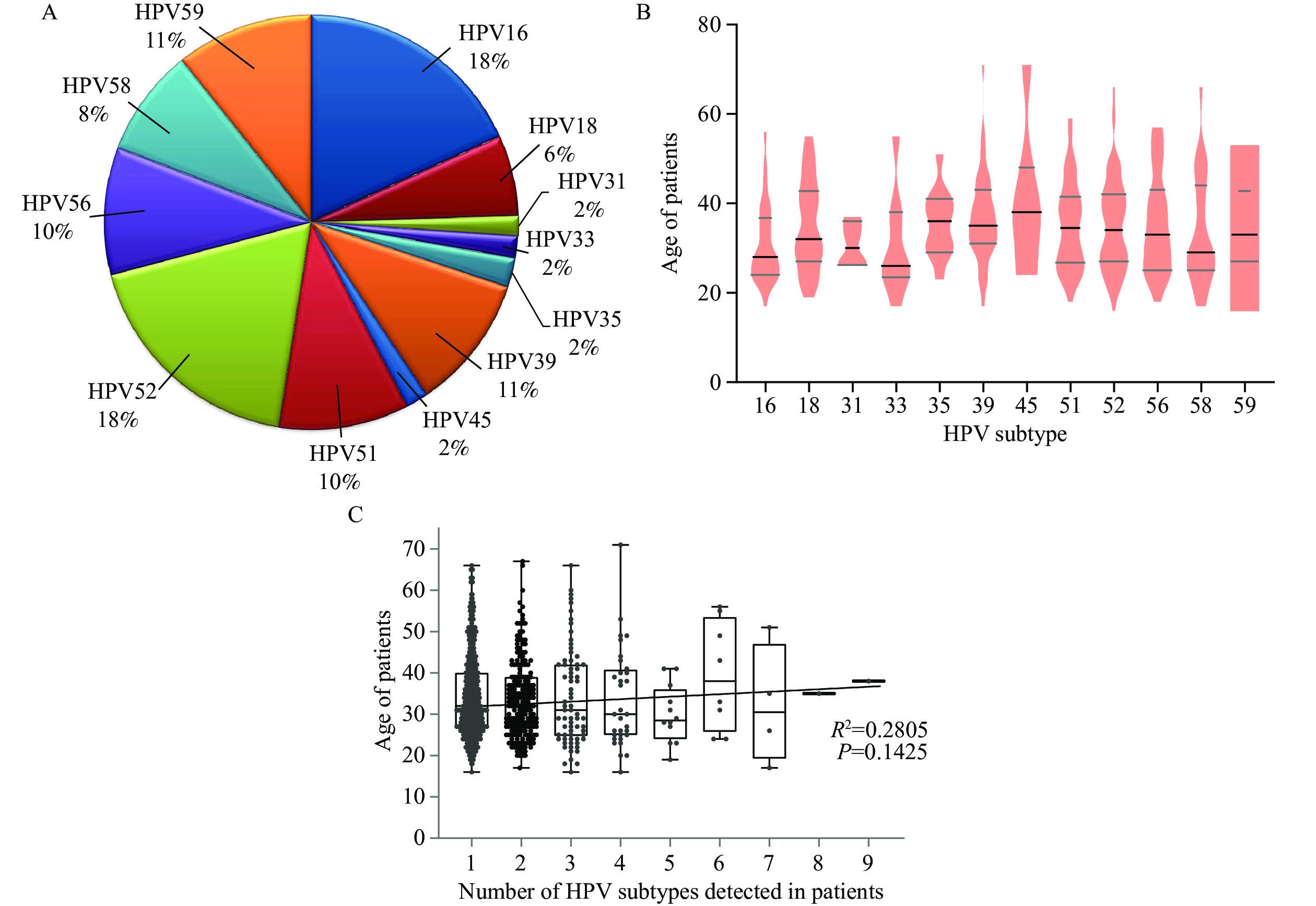 Figure 3.
Figure 3.Distribution of high-risk HPV genotypes and their association with patient age. (A) Proportion of high-risk HPV genotypes. (B) Age distribution of participants infected with different high-risk HPV genotypes. (C) Relationship between multiple HPV genotypes and age in HPV-positive participants.
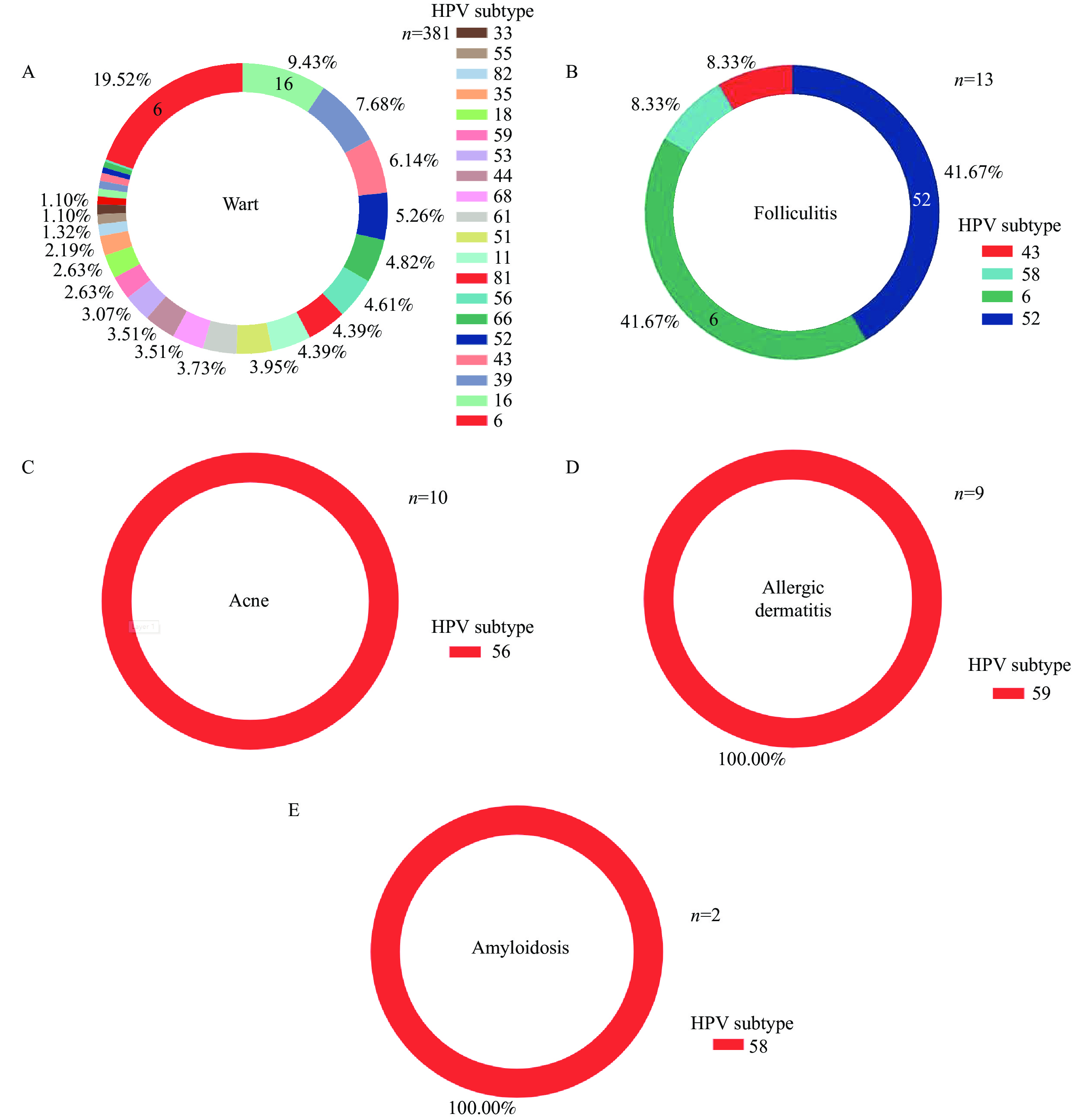
Abbreviation: HPV=human papillomavirus.This study explored the relationship between HPV genotypes and various skin and genital diseases. Patients with warts exhibited diverse HPV genotype infections with no predominant type. In folliculitis patients, HPV 6 and HPV 52 were the most common genotypes detected. Notably, specific HPV genotypes showed unique associations with certain conditions: HPV 56 with acne, HPV 59 with allergic dermatitis, and HPV 58 with amyloidosis. Among balanitis patients, HPV 58 was most prevalent (39.29%), followed by HPV 55 and HPV 59 (17.86% each). Warts patients demonstrated the most diverse HPV genotype profile, with HPV 6 being the most frequently detected, while other genotypes occurred at lower frequencies. In patients with urethritis, HPV 6, HPV 53, and HPV 52 were the predominant genotypes (Figure 4).
-
This study investigated the prevalence of HPV infection among males in Shenzhen City, Guangdong Province, China, revealing an overall infection rate of 45%. Notably, no significant age-related differences were observed between HPV-positive and HPV-negative groups, suggesting that age has minimal influence on HPV infection susceptibility in this population.
The genotype distribution analysis demonstrated a clear predominance of low-risk HPV types, with HPV 6 and HPV 11 accounting for 25% and 12% of positive cases, respectively. High-risk genotypes, particularly HPV 16, exhibited relatively low prevalence (<3%) but showed a concerning upward trend in recent years. The overall HPV positivity rate fluctuated throughout the study period, with negative cases increasing from 2018 to 2020, followed by a substantial rise in positive cases in 2022.
Our age-stratified analysis revealed a modest positive correlation between age and the number of HPV genotypes detected, indicating that older individuals may be more susceptible to multiple genotype co-infections. Specific genotype-age associations were also observed, with HPV 16 and HPV 33 more frequently detected in younger participants, while HPV 35 and HPV 45 showed higher prevalence among older individuals.
The study also identified distinct associations between specific HPV genotypes and various dermatological and genital conditions. Patients with warts demonstrated the most diverse HPV genotype profile, while certain conditions showed exclusive associations with specific genotypes — acne with HPV 56, allergic dermatitis with HPV 59, and amyloidosis with HPV 58. These findings suggest potential genotype-specific pathogenic mechanisms that warrant further investigation.
This study has several limitations that should be considered when interpreting the results. First, it was conducted exclusively in Shenzhen City, Guangdong Province, China, which may limit the generalizability of findings to other regions or populations with different demographic characteristics or health conditions. Future research should encompass broader geographic areas to validate these findings. Second, the use of a hospital-based cohort may introduce selection bias. A multicenter approach would enhance sample representativeness and improve the generalizability of results.
The findings of this study have significant implications for public health strategies, particularly for improving HPV vaccination programs. Currently, vaccination efforts predominantly target females, overlooking males as essential vectors in HPV transmission (11). This gender-specific approach fails to effectively address HPV across the entire population. Expanding vaccination programs to include males represents a critical opportunity to address this gap. Educational campaigns should raise awareness among males about HPV infection risks and vaccine effectiveness. Emphasizing prevention, early intervention, and male inclusion in vaccination programs can substantially reduce the overall burden of HPV-related diseases and improve global public health outcomes.
In conclusion, this study highlights the high prevalence of HPV infection among males with confirmed exposure and identifies significant associations between specific HPV genotypes and certain diseases. Implementing targeted prevention and intervention strategies for males, including vaccination and early screening, not only benefits male health but also plays a crucial role in controlling HPV transmission. This comprehensive approach ultimately contributes to female health protection and reduces the overall public health burden of HPV-related diseases.
HTML
| Citation: |



 Download:
Download: