-
Hypertension is the leading global modifiable risk factor for cardiovascular disease and all-cause death (1–2). Elevated blood pressure represents a primary preventable cause of cardiovascular disease (CVD) mortality and disease burden globally and in most regions worldwide (3–5). However, hypertension control rates remain low, particularly in low- and middle-income countries (LMICs) (6–7). In these regions, multiple barriers impede effective implementation, including limited healthcare access, high medication costs, low health literacy, and insufficient public awareness, thereby exacerbating hypertension-related morbidity and mortality. Research demonstrates that interventions led by non-physician healthcare providers can overcome these barriers and improve hypertension control (8–10). The China Rural Hypertension Control Project (CRHCP) introduced a low-cost, multi-level hypertension management model led by village doctors, which demonstrated significant reductions in both blood pressure and cardiovascular events (9,11). There is now an urgent need to promote this model nationwide to reduce the CVD burden across China.
This project comprises two phases: a pilot phase and an extension phase. It builds upon the CRHCP model by implementing a multi-level comprehensive hypertension management strategy targeting the general population in rural and township communities across China, aligned with national policies and local initiatives. In the CRHCP model, the project team conducts screening, provides blood pressure equipment, offers incentives to village doctors, and supports patients with discounted or free medications. In the pilot phase, village doctors received incentives to conduct screening and management, patients received additional support for medications beyond insurance coverage, and blood pressure devices with ID identification were provided to doctors. In the extension phase, patient enrollment was based on screening and local health records by village or community doctors, with no additional benefits beyond existing national policies. Locally sourced automatic blood pressure monitors with data transmission capabilities were used (Table 1). During screening, patients with resistant hypertension or blood pressure over 180/110 mmHg were referred to higher-level hospitals for further treatment after receiving essential antihypertensive treatment and were not included in the follow-up of the extension project. The project will be monitored by tracking key assessment indicators, including blood pressure control rate, medication usage rate, and drug dosage (calculated as the average number of antihypertensive medications being equal to the minimum dosage recommended by guidelines). This study has been approved by the Ethics Committee of the First Hospital of China Medical University. To date, this project has been launched in three provinces.
Program component CRHCP Pilot project Extension project Implementation phase NA Phase 1 Phase 2 Target population Rural areas Rural areas Rural areas & township communities Screening Conductor Project team Village doctors Village/community doctors (using insurance data) Incentives for doctors Yes Yes No Medication Support Discounted/free medications Subsidized through insurance No extra benefits BP equipment source Provided by project team Provided by project team Local equipment used Monitoring indicators Blood pressure and CVD events Blood pressure and use of nationally centralized procured antihypertensive medications Blood pressure and use of nationally centralized procured antihypertensive medications Abbreviation: NA=not applicable; CVD=cardiovascular disease; CRHCP=China Rural Hypertension Control Project. Table 1. Multi-level comprehensive intervention model.
The strategy translated from CRHCP includes five key components during implementation: 1) Community-wide screening of the entire population; 2) Implementation of a three-level hypertension management model across county, township, and village or community levels led by village or community doctors; 3) Ensuring that village or community doctors have prescribing authority and that village health clinics or community health centers provide nationally centralized procured antihypertensive medications (having good quality and low cost) with medical insurance coverage; 4) Adopting a simple and standard treatment protocol [or using artificial intelligence (AI) assisted protocol]; 5) Training village or community doctors in standardized blood pressure measurement, patient management, and healthy lifestyle promotion, such as salt reduction (including community- and family-based salt reduction packages) (12).
For detailed drug selection, a simple and practical standardized medication treatment flowchart for doctors has been developed based on the CRHCP model and the World Health Organization (WHO) HEARTS technical package for cardiovascular disease management in primary health care. In the current stage, medications are adjusted based on office blood pressure readings taken during each follow-up visit, with a target of 140/90 mmHg. In the future, a target of less than 130/80 mmHg will be considered in selected areas. Additionally, AI algorithm-based medication guidance terminals are used to assist with prescription and medication adjustment, ensuring rationality and safety.
-
The pilot project was conducted in two towns of Changtu County. A total of 5,088 hypertensive patients were enrolled in December 2023 through medical records and screening. At baseline, 1,227 subjects (25.7%) achieved the target blood pressure control of <140/90 mmHg. Follow-up assessments were conducted quarterly, including medication guidance and blood pressure monitoring (Table 2).
Variables Pilot project Extension project No. of patients with hypertension 5,088 243,165 Age, mean (SD) 63.6 (10.0) 63.4 (13.1) 60 and over 60, n (%) 3,384 (67.7) 186,124 (87.7) Female, n (%) 2,776 (54.6) 111,128 (52.0) Mean systolic BP (SD) 151.52 (22.2) 147.05 (18.1) Mean diastolic BP (SD) 88.31 (11.7) 88.53 (11.6) Note: Data are presented as mean (SD) or n (%).
Abbreviation: SD=standard deviation; BP=blood presure.Table 2. Baseline characteristics of participants in the pilot and extension projects.
Over the 13.0-month intervention period, blood pressure levels decreased progressively. The blood pressure control rate (<140/90 mmHg) improved substantially from 25.7% at baseline to 72.5%. The follow-up rate remained high at 93.9%. Notably, the proportion of patients achieving the more stringent target of <130/80 mmHg also increased significantly, from 8.7% at baseline to 28.1% (Figure 1).
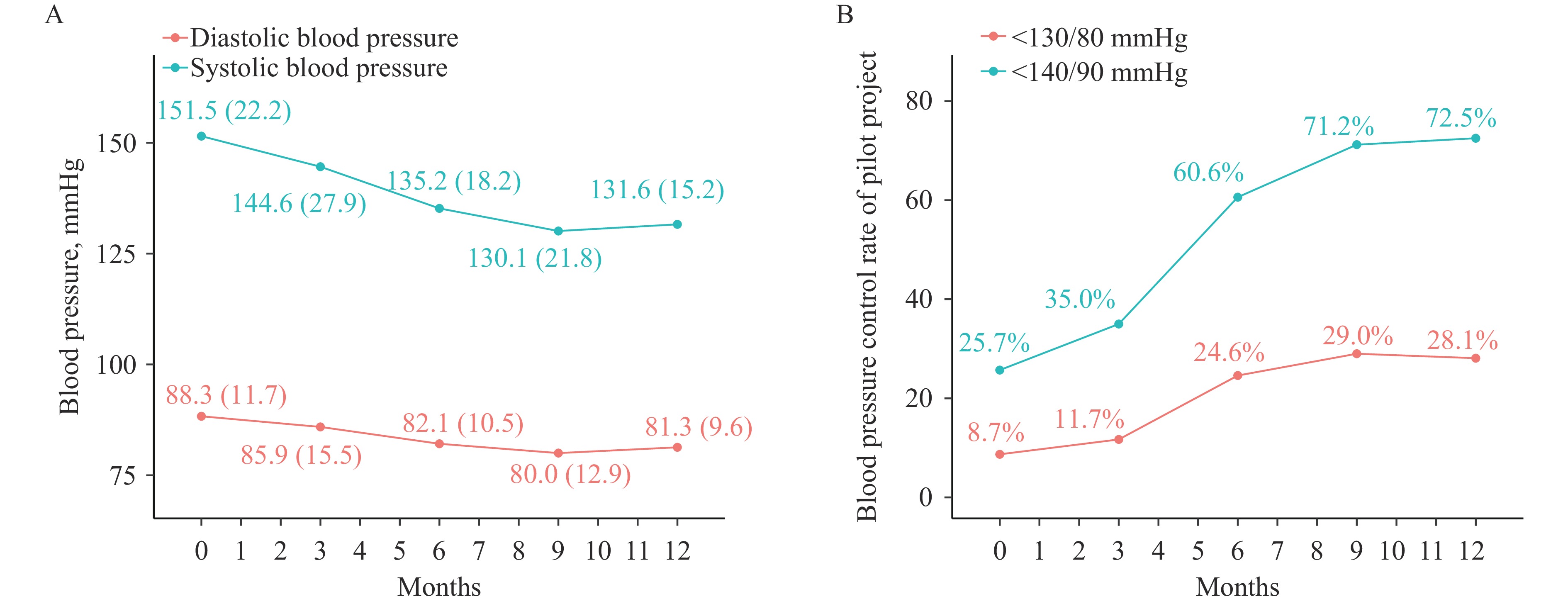 Figure 1.
Figure 1.Blood pressure outcomes and control rate of pilot project. (A) Mean systolic blood pressure and mean diastolic blood pressure. (B) Proportion of patients with systolic blood pressure <130 mmHg and diastolic blood pressure <80 mmHg and those with systolic blood pressure <140 mmHg and diastolic blood pressure <90 mmHg.
Note: For (A), error bars indicate 95% CIs. All P values for interactions between the intervention and follow-up time are <0.0001.
Abbreviation: CI=confidence interval.
-
Following the remarkable results of the pilot project, baseline data collection for the extension project was conducted in three provinces. A total of 244,046 hypertensive patients were identified through screening of 1,002,845 residents in Changtu City (Liaoning Province), Wujiang City (Jiangsu Province), and Tongguan City (Shaanxi Province) (Table 2).
To date, 164,925 patients (67.6%) have completed their first follow-up, with a median follow-up duration of 3.9 months. The treatment rate increased from 31.2% at baseline to 73.6%, accompanied by an increase in the average medication dose from 0.3 to 1.1. The average systolic blood pressure (SBP) and diastolic blood pressure (DBP) decreased from 146.8/88.4 mmHg to 140.4/82.6 mmHg, and the proportion of patients with controlled blood pressure improved from 20.8% at baseline to 44.0%. Ongoing follow-up is expected to yield higher participation rates. These results highlight the model’s effectiveness in implementation across both rural and urban settings (Table 3).
Study phase No. of patients with
hypertensionRate of
treatment*Average
doseAverage SBP
(mmHg)Average DBP
(mmHg)Control rate
(<140/90 mmHg)Control rate
(<130/80 mmHg)Baseline 244,046 30.1% 0.3 146.8 88.4 20.8% 10.0% Follow-up 164,925 73.7% 1.1 140.4 82.6 44.0% 14.4% P NA <0.001 <0.001 <0.001 <0.001 <0.001 <0.001 Abbreviation: NA=not applicable; SBP=systolic blood pressure; DBP=diastolic blood pressure.
* Treatment was defined as taking any dose of antihypertensive medications.Table 3. Blood pressure control and treatment indicators at baseline and 3-month follow-up.
-
This project translated the CRHCP model to improve hypertension control across China. Following adaptation of the CRHCP model into a public health approach, the hypertension control rate increased by 46.2% within one year in the pilot project, while the extension project demonstrated a 24.8% increase within just three months, accompanied by significant improvements in average medication dosage and treatment rates. These results indicate the potential effectiveness of this strategy in both rural and community settings throughout China.
The implementation and scaling of effective interventions often face significant challenges, particularly in resource-limited settings. While the WHO HEARTS technical package has been scaled worldwide, its effects have varied considerably across different contexts. In China, it yielded only limited improvement in hypertension control rates, with as many as 78.5% of enrolled patients lost to follow-up during implementation (13). However, the package worked well in countries with relatively sufficient resources. In four HEARTS countries using digital health information systems, facility-based blood pressure control improved from 18% at baseline to 46% over 48 months (13). Although economic status is important, the most critical factor in similar situations is the implementation of well-designed, evidence-based strategies combined with local resources. For our extension project, we translated the CRHCP model into five key components, with the integration of local resources and the original CRHCP strategy being crucial for improvements in hypertension control. Additionally, benefits likely stemmed from granting village or community doctors prescribing authority and ensuring sufficient centralized nationally procured antihypertensive medications in village health clinics and community health centers.
Building upon the CRHCP comprehensive intervention model, our current approach to hypertension management includes components similar to the HEARTS package (14), such as community-wide enrollment of the general population, a hypertension management system led by village doctors, empowerment of village doctors with prescribing authority, provision of nationally procured antihypertensive medications with medical insurance coverage, adoption of simple standardized treatment protocols, and training of village doctors in blood pressure measurement, patient management, and healthy lifestyle promotion, including salt reduction. The similarities between the HEARTS package and our extension project highlight that maximizing the integration of local resources is essential for achieving significant improvements in blood pressure control. In contrast to the HEARTS package, our project further institutionalizes hypertension care by granting prescribing authority to village doctors and incorporates digital innovations such as artificial intelligence-assisted treatment protocols to enhance clinical decision-making.
This study has several limitations. First, the follow-up duration in the extension phase was relatively short, and blood pressure was used as the primary outcome rather than hard cardiovascular endpoints. Future research will be necessary to assess long-term outcomes such as CVD events and all-cause mortality. Second, heterogeneity existed in the implementation process due to regional differences in resources, policy environments, and intervention measures. However, this variation also highlights a key strength of the study — its capacity to adapt to diverse local contexts and effectively leverage region-specific resources for intervention delivery.
-
The translation of the CRHCP model into a public health program has demonstrated promising results in improving hypertension control across selected regions of China. However, comprehensive long-term observation and evaluation are necessary to fully assess its effectiveness and sustainability. Before considering nationwide implementation, additional studies should be conducted to validate the model's adaptability across diverse settings and populations. If proven successful, this approach could serve as a replicable framework for other low- and middle-income countries and regions, offering an effective strategy for improving public health outcomes related to hypertension management.
-
The governments and village/community doctors of Changtu, Wujiang, and Tongguan Counties for their invaluable support and collaboration in data collection, participant recruitment, and program implementation.
HTML
Pilot Project
Extension Project
| Citation: |



 Download:
Download:




