-
Introduction: Human papillomaviruses (HPV) testing and liquid-based cytology (LBC) are the primary screening methods for cervical cancer. However, recent nationwide data on HPV distribution across different cytological conditions in China remains limited.
Methods: This nationwide cross-sectional study analyzed health check-up data from the Dian laboratory network across China in 2023. The study included 238,807 women aged ≥20 years from 23 PLADs who underwent both HPV genotyping and LBC testing. The rates of abnormal cytology and HPV infection were weighted and standardized according to the Seventh National Population Census (2020).
Results: The overall weighted rates of HR-HPV infection and abnormal cytology were 12.30% and 9.25%, respectively. Among women with abnormal cervical cytology, HPV-16 was the most prevalent HR-HPV genotype, followed by HPV-58 and HPV-52.
Conclusions: The detection rates of HR-HPV and abnormal cytology remain relatively high in China. Both single and multiple HR-HPV infections were associated with increased risk of abnormal cervical cytology. These findings may inform the development of HPV genotype-specific vaccination and screening strategies to reduce cervical cancer burden.
-
Cervical cancer ranks as the fourth most common cancer globally in terms of both incidence and mortality among women, with a particularly high burden in low- and middle-income countries (1). Analysis of 700 population-based cancer registries in China revealed approximately 150,700 new cervical cancer cases and 55,700 deaths in 2022 (2). Human papillomaviruses (HPV) are sexually transmitted viruses that have been established as the primary etiological factor in cervical cancer development. While HPV testing and liquid-based cytology (LBC) remain the cornerstone methods for cervical cancer screening, current comprehensive data on high-risk HPV (HR-HPV) infection and LBC findings across China are limited. This nationwide, cross-sectional, population-based study conducted in 2023 aimed to characterize the detection rates of HR-HPV infection and abnormal cervical cytology among women undergoing health check-ups, and to analyze the associations between cytological abnormalities and HR-HPV infections. The study included 238,807 eligible women aged 20 years or older from 23 provincial-level administrative divisions (PLADs). Analysis revealed weighted detection rates of 12.30% for HR-HPV infection and 9.25% for abnormal cytology. Among women with abnormal cervical cytology, HPV-16 was the predominant HR-HPV genotype, followed by HPV-58 and HPV-52. These findings, derived from a large population-based sample in China, provide valuable insights into the current status of cervical cancer screening outcomes and may inform the development of HPV genotype-specific vaccination and screening strategies to reduce cervical cancer burden.
This nationwide, cross-sectional, population-based study utilized de-identified data from the Dian laboratory health check-ups database across China. From 248,913 women who underwent routine health check-ups or cervical cancer screening in 2023 across 1,638 submission units in 221 cities across 28 PLADs, 238,807 eligible women (95.9%) from 208 cities in 23 PLADs met the inclusion criteria: complete age and submission unit data, comprehensive testing data for 23 HPV genotypes and LBC outcomes, age ≥20 years, and a minimum of 1,000 individuals tested per PLAD. HPV specimens were collected by clinical physicians or nurses following standardized protocols. HPV detection and genotyping were performed using the Human Papillomavirus DNA Test Kit (Fluorescence Melting Curve Method) (Hangzhou DIAN Biotechnology Co., Ltd). The assay detected 14 HR-HPV genotypes: HPV-16, -18, -31, -33, -35, -39, -45, -51, -52, -56, -58, -59, -66, and -68. Single infection was defined as infection with one HPV genotype, while multiple infections were defined as infections with two or more genotypes. LBC was conducted following standard operating procedures, including Papanicolaou staining and liquid-based cytology sample preparation. LBC outcomes were classified according to The Bethesda System for Reporting Cervical Cytology (TBS) as: negative for intraepithelial lesion or malignancy (NILM), atypical squamous cells (ASC) including atypical squamous cells of undetermined significance (ASC-US) and atypical squamous cells-cannot exclude high-grade squamous intraepithelial lesion (ASC-H), low-grade squamous intraepithelial lesion (LSIL), high-grade squamous intraepithelial lesion (HSIL), squamous cell carcinoma (SCC), and atypical glandular cells (AGC). Due to low detection rates, ASC-H was combined with ASC-US into ASC for analysis, while AGC and SCC were excluded due to insufficient numbers for independent analysis.
Statistical analysis included descriptive statistics using frequencies and proportions, with group comparisons performed using Chi-square tests. Detection rates for abnormal cytology and HPV infection were weighted and standardized by 5-year age groups and provinces according to the female population distribution (aged ≥20 years) from the Seventh National Population Census in 2020. Multivariable logistic regression was employed to calculate odds ratios (OR) and 95% confidence intervals (CI), adjusting for age group, geographical region, and city-level random effects. Analyses were conducted using R software (version 4.4.2, R Core Team, Vienna, Austria), with statistical significance set at P<0.05 using two-tailed tests.
Among the 238,807 women aged 20 years and older (mean age 42.0±10.2 years), 17,271 individuals presented with cytological abnormalities. The weighted rates were 6.24% for ASC-US, 0.27% for ASC-H, 2.34% for LSIL, and 0.40% for HSIL (Table 1). Significant differences in LBC outcomes were observed across age groups (P<0.001), with total abnormality, LSIL, and HSIL rates increasing with age. Notable variations were also found across regions and HR-HPV infection groups, with the weighted rate of cytological abnormality exceeding 50% in the multiple infection group.
Characteristics N (%) NILM
(%, 95% CI)ASC-US
(%, 95% CI)ASC-H
(%, 95% CI)LSIL
(%, 95% CI)HSIL
(%, 95% CI)P Overall 238,807
(100.00)90.75
(89.59, 91.97)6.24
(5.87, 6.71)0.27
(0.20, 0.49)2.34
(2.11, 2.67)0.40
(0.27, 0.67)Age groups (years) <0.001 20−24 5,923
(2.48)90.60
(87.01, 94.44)7.04
(5.94, 8.44)− 2.36
(1.82, 3.24)− 25−29 17,268
(7.23)93.62
(91.47, 95.84)4.51
(4.03, 5.08)0.04
(0.02, 0.22)1.77
(1.43, 2.22)0.06
(0.02, 0.24)30−34 39,132
(16.39)93.82
(92.30, 95.39)4.41
(4.07, 4.81)0.12
(0.08, 0.23)1.54
(1.32, 1.81)0.11
(0.05, 0.24)35−39 43,184
(18.08)93.16
(91.70, 94.66)4.66
(4.32, 5.03)0.16
(0.09, 0.28)1.85
(1.63, 2.12)0.18
(0.13, 0.28)40−44 39,320
(16.47)93.42
(91.86, 95.02)4.71
(4.34, 5.12)0.13
(0.07, 0.24)1.54
(1.34, 1.80)0.21
(0.12, 0.35)45−49 36,602
(15.33)92.35
(90.61, 94.13)5.22
(4.78, 5.71)0.15
(0.08, 0.30)2.11
(1.83, 2.45)0.18
(0.11, 0.32)50−54 30,267
(12.67)90.70
(88.84, 92.63)6.49
(5.95, 7.09)0.26
(0.15, 0.46)2.22
(1.92, 2.59)0.33
(0.22, 0.53)55−59 15,613
(6.54)88.98
(86.38, 91.69)7.48
(6.76, 8.32)0.44
(0.26, 0.80)2.79
(2.33, 3.39)0.32
(0.16, 0.65)60−64 6,662
(2.79)87.51
(83.45, 91.88)7.66
(6.55, 9.11)0.96
(0.49, 1.91)3.30
(2.58, 4.40)0.57
(0.29, 1.35)65−69 3,011
(1.26)87.93
(81.55, 95.22)7.14
(5.44, 10.00)0.72
(0.31, 2.78)3.60
(2.23, 6.28)0.62
(0.22, 2.71)≥70 1,825
(0.76)85.91
(78.74, 93.99)9.30
(6.82, 12.89)0.24
(0.01, 2.21)3.00
(1.68, 5.57)1.56
(0.63, 3.88)Geographical regions <0.001 Eastern 98,582
(41.28)91.68
(90.20, 93.23)5.69
(5.26, 6.21)0.23
(0.16, 0.45)2.18
(1.94, 2.52)0.24
(0.17, 0.45)Central 95,710
(40.08)90.77
(88.96, 92.82)6.10
(5.49, 7.03)0.28
(0.14, 0.94)2.29
(1.83, 3.12)0.55
(0.34, 1.22)Western 44,515
(18.64)88.94
(85.74, 92.49)7.50
(6.44, 9.01)0.35
(0.20, 1.23)2.70
(2.19, 3.73)0.51
(0.13, 1.62)HR-HPV infection <0.001 Negative 212,808
(89.11)95.47
(94.11, 97.18)3.55
(3.25, 4.40)0.07
(0.02, 0.96)0.86
(0.74, 1.67)0.05
(0.01, 0.95)Single 22,780
(9.54)60.17
(57.41, 63.80)24.72
(22.69, 27.72)1.70
(1.29, 3.64)10.81
(9.81, 12.98)2.60
(1.62, 4.93)Multiple 3,219
(1.35)47.64
(42.85, 53.80)27.80
(24.35, 32.70)1.51
(0.80, 4.52)19.8
(16.54, 24.59)3.26
(1.77, 6.81)Note: The weighted prevalence of cervical cytology outcomes was standardized by age groups and provinces according to the distribution of the female population aged 20 years and above from the Seventh National Population Census in 2020. “−” means the number of detected cases in this group is zero.
Abbreviation: PLADs=provincial-level administrative divisions; CI=confidence interval; NILM=negative for intraepithelial lesion or malignancy; ASC-US=atypical squamous cells of undetermined significance; ASC-H=atypical squamous cells-cannot exclude high-grade squamous intraepithelial lesion; LSIL=low-grade squamous intraepithelial lesion; HSIL=high-grade squamous intraepithelial lesion; HR-HPV=high-risk human papillomavirus.Table 1. The weighted prevalence of cervical cytology outcomes among women in 23 PLADs, China, 2023.
The overall weighted HR-HPV infection rate was 12.30%, comprising 10.55% single infections and 1.75% multiple infections. Figure 1 illustrates the distribution of HR-HPV genotypes across different LBC outcomes. HR-HPV infection rates varied significantly by cytological status: 7.78% in NILM, 52.34% in ASC, 69.82% in LSIL, and 94.74% in HSIL. HPV-16, HPV-52, and HPV-58 were the predominant genotypes across both single and multiple infections. While HPV-52 and HPV-58 showed the highest infection rates in NILM specimens, HPV-16 demonstrated increasing prevalence in more severe cytological abnormalities, reaching 9.77% for single infections and 2.66% for multiple infections in ASC. In HSIL specimens, HPV-16 single infection rates peaked at 42.27%, with multiple infections at 10.52%.
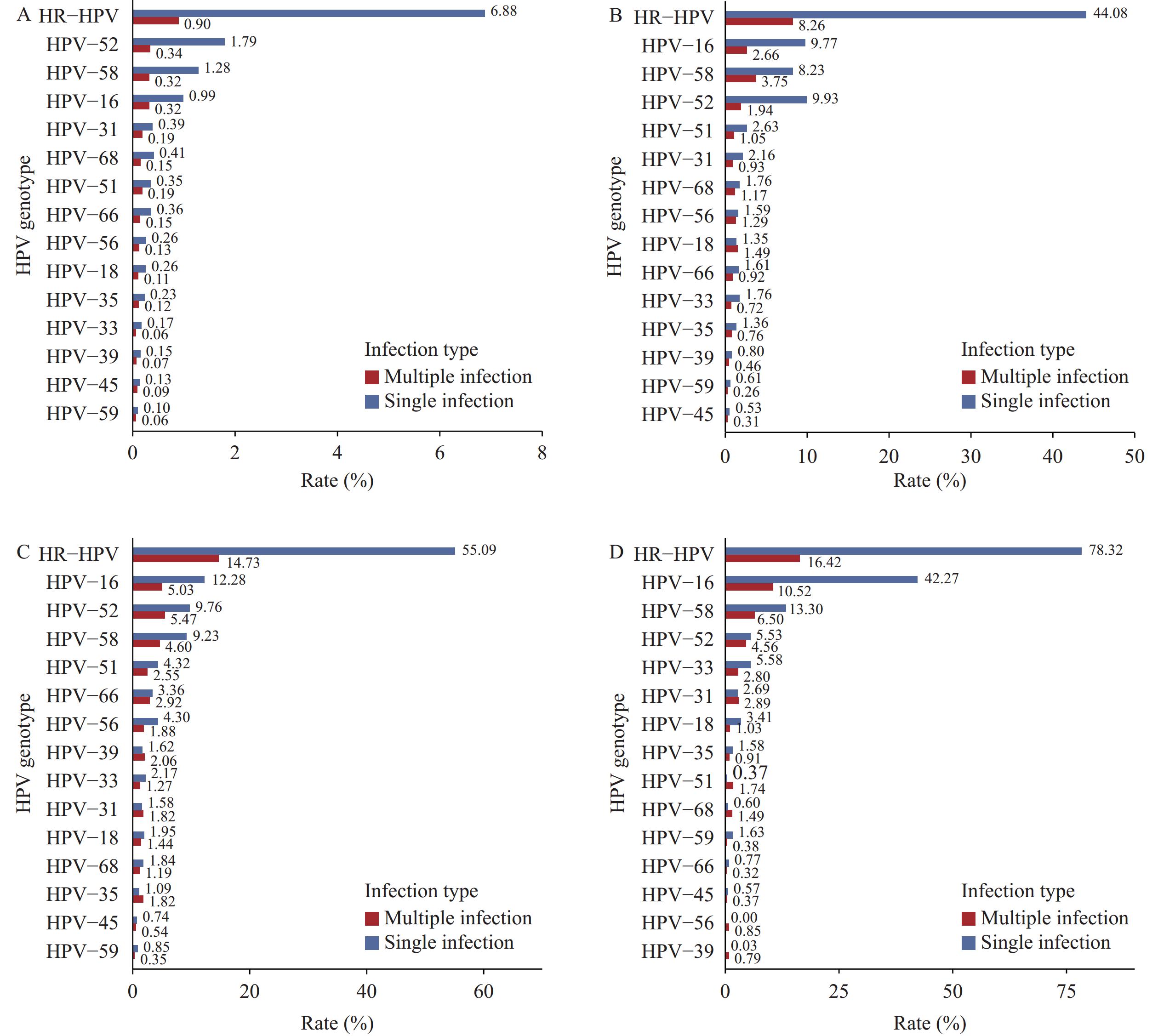 Figure 1.
Figure 1.Distribution of HR-HPV single and multiple infections across cervical cytology outcomes among women in 23 PLADs, China, 2023. (A) NILM; (B) ASC; (C) LSIL; (D) HSIL.
Note: The weighted rates of HR-HPV single and multiple infections were standardized by age groups and provinces according to the female population aged 20 and above from the Seventh National Population Census in 2020.
Abbreviation: HR-HPV=high-risk human papillomavirus; PLADs=provincial-level administrative divisions; NILM=negative for intraepithelial lesion or malignancy; ASC=atypical squamous cells; LSIL=low-grade squamous intraepithelial lesion; HSIL=high-grade squamous intraepithelial lesion.
Table 2 presents the associations between HR-HPV infections and cervical cytological abnormalities. All 14 HR-HPV genotypes exhibited statistically significant positive associations with both ASC and LSIL, regardless of single or multiple infections, when compared to HPV-negative groups. Notably, for HSIL, significant associations were observed exclusively with multiple infection with any HR-HPV genotypes and single infections of HR-HPV types 16, 18, 31, 33, 35, 52, and 58.
HR-HPV genotype NILM ASC LSIL HSIL n (%) n (%) aOR (95% CI)* n (%) aOR (95% CI)* n (%) aOR (95% CI)* HPV-16 Negative 219,049 (93.7) 11,120 (4.8) 1.00 (Ref) 3,466 (1.5) 1.00 (Ref) 205 (0.1) 1.00 (Ref) Single infection 1,996 (51.5) 1,174 (30.3) 12.16 (11.26, 13.13) 500 (12.9) 16.51 (14.85, 18.37) 203 (5.2) 111.23 (90.57, 136.61) Multiple infection 491 (44.9) 363 (33.2) 14.01 (12.18, 16.11) 185 (16.9) 23.63 (19.81, 28.20) 55 (5.0) 116.89 (84.65, 161.42) HPV-18 Negative 220,794 (92.9) 12,317 (5.2) 1.00 (Ref) 4,017 (1.7) 1.00 (Ref) 446 (0.2) 1.00 (Ref) Single infection 539 (62.1) 245 (28.2) 7.82 (6.73, 9.10) 73 (8.4) 7.09 (5.56, 9.04) 11 (1.3) 9.26 (4.94, 17.33) Multiple infection 203 (55.6) 95 (26.0) 8.44 (6.68, 10.65) 61 (16.7) 17.02 (12.85, 22.54) 6 (1.6) 13.71 (5.80, 32.42) HPV-31 Negative 220,367 (92.9) 12,299 (5.2) 1.00 (Ref) 3,990 (1.7) 1.00 (Ref) 442 (0.2) 1.00 (Ref) Single infection 899 (73.0) 239 (19.4) 4.56 (3.94, 5.27) 82 (6.7) 4.79 (3.82, 6.00) 12 (1.0) 5.66 (3.14, 10.18) Multiple infection 270 (56.6) 119 (24.9) 7.23 (5.86, 8.91) 79 (16.6) 15.32 (11.90, 19.73) 9 (1.9) 13.94 (7.00, 27.77) HPV-33 Negative 220,972 (92.9) 12,370 (5.2) 1.00 (Ref) 4,014 (1.7) 1.00 (Ref) 425 (0.2) 1.00 (Ref) Single infection 420 (55.3) 214 (28.2) 8.25 (7.00, 9.72) 98 (12.9) 11.60 (9.27, 14.51) 28 (3.7) 29.09 (19.35, 43.73) Multiple infection 144 (54.1) 73 (27.4) 8.39 (6.37, 11.04) 39 (14.7) 14.82 (10.36, 21.21) 10 (3.8) 30.77 (15.55, 60.89) HPV-35 Negative 220,833 (92.9) 12,385 (5.2) 1.00 (Ref) 4,025 (1.7) 1.00 (Ref) 451 (0.2) 1.00 (Ref) Single infection 507 (69.1) 164 (22.3) 5.32 (4.48, 6.33) 55 (7.5) 5.66 (4.32, 7.40) 8 (1.1) 6.70 (3.27, 13.71) Multiple infection 196 (51.7) 108 (28.5) 9.05 (7.25, 11.29) 71 (18.7) 19.77 (15.13, 25.85) 4 (1.1) 7.94 (2.86, 22.04) HPV-39 Negative 221,068 (92.9) 12,466 (5.2) 1.00 (Ref) 4,053 (1.7) 1.00 (Ref) 460 (0.2) 1.00 (Ref) Single infection 333 (65.2) 127 (24.9) 6.88 (5.62, 8.43) 50 (9.8) 7.96 (5.92, 10.7) 1 (0.2) 1.43 (0.20, 10.50) Multiple infection 135 (54.2) 64 (25.7) 8.49 (6.34, 11.37) 48 (19.3) 21.32 (15.38, 29.56) 2 (0.8) 6.58 (1.55, 27.88) HPV-45 Negative 221,121 (92.8) 12,547 (5.3) 1.00 (Ref) 4,098 (1.7) 1.00 (Ref) 458 (0.2) 1.00 (Ref) Single infection 256 (72.7) 66 (18.8) 4.20 (3.22, 5.46) 29 (8.2) 5.64 (3.89, 8.19) 1 (0.3) 1.56 (0.31, 7.89) Multiple infection 159 (68.8) 44 (19.0) 5.18 (3.74, 7.18) 24 (10.4) 8.65 (5.70, 13.11) 4 (1.7) 11.52 (4.40, 30.14) HPV-51 Negative 220,504 (93.0) 12,223 (5.2) 1.00 (Ref) 3,864 (1.6) 1.00 (Ref) 454 (0.2) 1.00 (Ref) Single infection 746 (62.7) 273 (22.9) 6.57 (5.71, 7.55) 169 (14.2) 12.98 (10.93, 15.42) 2 (0.2) 1.29 (0.31, 5.29) Multiple infection 286 (50.0) 161 (28.1) 9.50 (7.86, 11.49) 118 (20.6) 23.52 (18.87, 29.32) 7 (1.2) 10.48 (4.82, 22.77) HPV-52 Negative 217,250 (93.6) 11,069 (4.8) 1.00 (Ref) 3,479 (1.5) 1.00 (Ref) 414 (0.2) 1.00 (Ref) Single infection 3,697 (67.9) 1,263 (23.2) 6.41 (6.00, 6.86) 454 (8.3) 7.31 (6.59, 8.12) 30 (0.6) 4.01 (2.76, 5.82) Multiple infection 589 (51.2) 325 (28.2) 9.92 (8.64, 11.39) 218 (18.9) 21.79 (18.52, 25.63) 19 (1.7) 14.36 (8.90, 23.16) HPV-56 Negative 220,768 (93.0) 12,331 (5.2) 1.00 (Ref) 3,881 (1.6) 1.00 (Ref) 459 (0.2) 1.00 (Ref) Single infection 538 (58.4) 200 (21.7) 6.51 (5.53, 7.65) 183 (19.9) 18.91 (15.86, 22.55) 0 - Multiple infection 230 (51.5) 126 (28.2) 8.79 (7.11, 10.86) 87 (19.5) 19.57 (15.13, 25.29) 4 (0.9) 6.30 (2.43, 16.33) HPV-58 Negative 218,443 (93.4) 11,416 (4.9) 1.00 (Ref) 3,549 (1.5) 1.00 (Ref) 373 (0.2) 1.00 (Ref) Single infection 2,574 (64.8) 913 (23.0) 6.46 (5.97, 6.99) 425 (10.7) 9.64 (8.64, 10.75) 58 (1.5) 11.61 (8.71, 15.46) Multiple infection 519 (49.1) 328 (31.1) 11.25 (9.78, 12.95) 177 (16.8) 20.64 (17.31, 24.60) 32 (3.0) 31.61 (21.47, 46.55) HPV-59 Negative 221,123 (92.8) 12,529 (5.3) 1.00 (Ref) 4,089 (1.7) 1.00 (Ref) 458 (0.2) 1.00 (Ref) Single infection 285 (70.4) 83 (20.5) 5.13 (4.08, 6.44) 35 (8.6) 6.70 (4.82, 9.31) 2 (0.5) 3.56 (0.87, 14.59) Multiple infection 128 (63.1) 45 (22.2) 6.15 (4.56, 8.30) 27 (13.3) 12.57 (8.66, 18.25) 3 (1.5) 9.40 (2.87, 30.86) HPV-66 Negative 220,451 (93.0) 12,325 (5.2) 1.00 (Ref) 3,890 (1.6) 1.00 (Ref) 456 (0.2) 1.00 (Ref) Single infection 815 (69.4) 204 (17.4) 4.31 (3.69, 5.03) 154 (13.1) 10.39 (8.72, 12.38) 2 (0.2) 1.08 (0.29, 3.98) Multiple infection 270 (52.9) 128 (25.1) 8.13 (6.60, 10.03) 107 (21.0) 22.33 (17.74, 28.11) 5 (1.0) 7.45 (3.10, 17.88) HPV-68 Negative 220,224 (92.9) 12,281 (5.2) 1.00 (Ref) 4,019 (1.7) 1.00 (Ref) 455 (0.2) 1.00 (Ref) Single infection 1,021 (75.9) 251 (18.7) 4.19 (3.64, 4.81) 70 (5.2) 3.46 (2.73, 4.40) 3 (0.2) 1.35 (0.43, 4.27) Multiple infection 291 (60.2) 125 (25.9) 7.26 (5.91, 8.91) 62 (12.8) 10.88 (8.31, 14.25) 5 (1.0) 7.00 (2.82, 17.36) Note: “−” means the number of detected cases in this group is zero.
Abbreviation: HR-HPV=high-risk human papillomavirus; PLADs=provincial-level administrative divisions; NILM=negative for intraepithelial lesion or malignancy; ASC=atypical squamous cells; LSIL=low-grade squamous intraepithelial lesion; HSIL=high-grade squamous intraepithelial lesion; aOR=adjusted odds ratio; CI=confidence interval; Ref=reference.
* Adjusted for age group, geographical region, and the random effects at city level.Table 2. Association between HR-HPV genotype infection and abnormal cervical cytology among women in 23 PLADs, China, 2023.
-
This study revealed that the HR-HPV infection rate was 12.30%, with an abnormal cytology detection rate of 9.25%. The HR-HPV infection rate demonstrated a clear correlation with cervical cytological severity, increasing from 7.78% in NILM to 94.74% in HSIL. Both HR-HPV multiple infections and single infections showed significant associations with cytological abnormalities, with most HR-HPV single infections and all multiple infections conferring higher risks of ASC, LSIL, and HSIL. These findings underscore the critical role of multiple HR-HPV infections and single infections of highly carcinogenic types (particularly HPV-16) in driving cytological changes. Furthermore, these results highlight the essential value of combined LBC and HPV screening in risk assessment for precancerous lesions and the development of clinical management strategies.
The weighted detection rates of HR-HPV infection (12.30%) and abnormal cytology (≥ASC-US) (9.25%) observed in our study are comparable to previous research in China, which reported similar HR-HPV infection rates (12.1%) but lower rates of abnormal cytology (7.48%) (3-4) . Age-specific analysis revealed that cytological abnormalities predominantly manifested as ASC and LSIL in younger age groups, potentially reflecting transient or short-term HR-HPV infections. Conversely, HSIL detection rates increased with age, particularly among women aged 60 and above. This age-dependent increase in HSIL likely results from the cumulative effects of persistent HPV infections, immunological changes, and hormonal variations. These patterns emphasize the necessity for age-specific screening and management protocols, with particular attention to screening and follow-up in elderly populations. Current evidence has identified 13 HPV genotypes as carcinogenic for cervical cancer (5). Persistent infection with HR-HPV, especially those with high carcinogenic potential, is well-established as the primary etiological factor in the development of abnormal cervical cytology, precancerous lesions, and cervical cancer (6). Our findings demonstrated that HR-HPV multiple infection rates increased proportionally with cervical cytological severity. However, since cytological abnormalities do not invariably progress to precancerous lesions, further research is needed to determine whether HR-HPV multiple infections increase the risk of cervical cancer progression.
In this study, the five most prevalent HR-HPV genotypes identified in the population with normal cytology were HPV-52, -58, -16, -68, and -31, aligning with previous global and Chinese research findings (7–8). Although HPV-52 and HPV-58 show relatively high prevalence in China, HPV-16 remained the predominant genotype among women with LSIL and HSIL. This finding underscores the exceptional carcinogenic potential of HPV-16, which accounts for over 60% of cervical squamous cell carcinomas, adenocarcinomas, and other anogenital and oropharyngeal cancers (9). A study examining HPV genotype-specific population attributable fractions (AFs) in invasive cervical cancer reveals that HPV-16, -18, -31, -33, -35, -45, -52, and -58 demonstrate the highest AFs, closely corresponding to the high-detection-rate HR-HPV genotypes in HSIL observed in our study. In China, the combined AF of HPV-16 and -18 reaches 75.6%, while the AF for HPV-16, -18, -31, -33, -45, -52, and -58 collectively accounts for 95.4% (10). Therefore, despite bivalent and quadrivalent HPV vaccines not including HPV-52 and HPV-58, expanding vaccination coverage remains crucial, regardless of vaccine type.
This study’s primary strengths lie in its utilization of a large-scale, multi-center database from across China and standardized quality control procedures, enhancing data reliability and providing valuable insights for cervical cancer screening. However, several limitations warrant consideration. First, while based on comprehensive cervical cancer screening data, the study lacks colposcopy and histopathology results post-screening, which could have enabled further analysis of the causal relationship between HR-HPV genotype infection and invasive cervical cancer. Second, the cross-sectional design without longitudinal follow-up precludes investigation of persistent HR-HPV infection’s impact on cervical cytological changes and precancerous lesions. Third, the database lacks crucial personal information, including residential area and HPV vaccination status. Nevertheless, this remains a significant population-based study in China, providing a foundation for future research.
In conclusion, this nationwide cross-sectional study revealed persistently high detection rates of HR-HPV infection and abnormal cytology based on a large-scale cervical cancer screening database in China. Among women with abnormal cervical cytology, HPV-16 emerged as the predominant HR-HPV genotype, followed by HPV-58 and HPV-52. These findings provide valuable insights that may inform the development of targeted HPV genotype-specific vaccination strategies and optimize screening protocols to reduce the burden of cervical cancer in China.
-
All women who participated in this study and acknowledge the dedicated efforts of the data collection staff at Dian laboratory.
HTML
| Citation: |



 Download:
Download:




