-
Acute respiratory tract infections (ARTIs), encompassing both the upper and lower respiratory tract infections (RTIs) (1-3), represent a significant cause of morbidity and mortality in children under five years of age, particularly in developing countries (4). Approximately 85% of children worldwide experience an ARTI annually. While multiple pathogens can cause ARTIs, viruses are responsible for nearly 90% of cases in children (2,5). Human respiratory syncytial virus (HRSV) stands as the primary etiologic agent of acute lower RTIs in pediatric patients, characterized by rapid onset, high transmissibility, early non-specific presentations, and a propensity for seasonal and regional epidemics. The severity of the clinical manifestations correlate directly with viral load. Furthermore, HRSV has garnered substantial attention due to its considerable disease burden, being associated with approximately three million hospitalizations and over 100,000 deaths annually in children younger than 5 years globally (5). Epidemiological surveillance of the HRSV in children with ARTI enables understanding of its incidence and epidemic patterns, thereby providing an evidence base for prevention and control strategies. To this end, we analyzed HRSV distribution patterns in children with ARTI from 2021–2023.
-
This study employed sentinel surveillance at four monitoring sites in Shijiazhuang City, Hebei Province, China: the Second and Fourth Hospitals of Hebei Medical University, Hebei Provincial Children’s Hospital, and Lu Quan District People’s Hospital. We collected throat swabs from 20 children with upper RTIs and alveolar lavage fluid samples from 20 children with lower RTIs monthly from 2021 to 2023, yielding 1,440 total cases. All participants met the case definitions and underwent standardized epidemiological investigations with completed case investigation forms. Upper RTI samples were collected from all four sentinel hospitals, with 4–6 samples randomly obtained weekly per site. Lower RTI samples were exclusively collected from Hebei Children's Hospital, with 4–6 samples randomly collected weekly. Inclusion criteria required patients to be ≤14 years old and permanent residents of Shijiazhuang City. All samples were tested specimens were analyzed using a one-step respiratory multiple detection kit (Hangzhou Newrosimin Biotechnology Co., Ltd) to test for human parainfluenza virus (HPIV), influenza virus (IFV), adenovirus (ADV), HRSVA/B, rhinovirus (HRV), human enterovirus, human Boca virus (HBoV), human metapneumovirus, coronavirus OC43/HKU1/229E/NL63, and severe acute respiratory syndrome coronavirus-2.
-
A total of 112 HRSV-positive cases were detected out of the 1,440 specimens, with a detection rate of 7.8%. The detection rates of upper and lower respiratory tract specimens were 6.9% and 8.6%, respectively. There were 23 cases of coinfection (only detected in cases of lower RTIs), including 19 cases of double infection and 4 cases of triple infection. Coinfections with Human bocavirus and influenza virus were the most common (Table 1).
Coinfection Mixed type Number Double infection HRSV+ADV 1 HRSV+IFV 4 HRSV+HBoV 5 HRSV+HPIV 3 HRSV+HRV 3 HRSV+EV 1 HRSV+OC43 2 Triple infection HRSV+HBoV+IFV 2 HRSV+HPIV+HRV 1 HRSV+HBoV+HRV 1 Abbreviation: HRSV=human respiratory syncytial virus; ARTI=acute respiratory tract infection; ADV=adenovirus; IFV=influenza virus; HBoV=human Boca virus; HPIV=human parainfluenza virus; HRV=rhinovirus; EV=human enterovirus; OC43=coronavirus OC43. Table 1. Detection of HRSV coinfection in children with ARTI.
The detection rate of HRSV was the highest in the spring (12.2%), followed by the winter (10.3%), and was lowest in the autumn (2.8%) (P<0.05). Among the upper RTIs, HRSV infection was more common in the spring (14.4%). Lower RTIs were more common in the winter and spring (13.3% and 10.3%) (P<0.05). HRSV rates were the highest in the spring, summer and winter of 2021 (10.0%, 12.5%, and 10.8%), the winter and spring of 2022 (15.8%, 10.0%), and the spring of 2023 (16.7%) (Table 2 and Table 3) . Peak HRSV detection in the spring and summer of 2021 was mainly caused by HRSV-B infection (and was mainly lower RTI cases). Upper RTIs detected in the winter of 2021 were largely caused by HRSVA+HRSVB, and lower RTIs at this time were mainly caused by HRSVA. The spring 2022 peak was mainly caused by HRSVA+HRSVB (and was mainly upper RTIs). The winter 2022 peak and spring 2023 peak were mainly caused by HRSVA infections (Figure 1).
Detection rate Spring n (%) Summer n (%) Autumn n (%) Winter n (%) χ2 P Total detection rate (N=360) 44 (12.2) 21 (5.8) 10 (2.8) 37 (10.3) 27.496 <0.001 Detection rate of upper RTIs (N=180) 26 (14.4) 7 (3.9) 4 (2.2) 13 (7.2) 24.501 <0.001 Detection rate of lower RTIs (N=180) 18 (10.0) 14 (7.8) 6 (3.3) 24 (13.3) 12.072 0.007 Note: Spring includes March to May; Summer includes June to August; Autumn includes September to November; Winter includes December to February.
Abbreviation: ARTI=acute respiratory tract infection; RTI=respiratory tract infection; HRSV=Human respiratory syncytial virus.Table 2. Seasonal distribution of HRSV in children with ARTI in Shijiazhuang City, Hebei Province, China, 2021–2023.
Season Detection rate (N=120) n (%) Upper RTIs (N=60) n (%) Lower RTIs (N=60) n (%) Upper RTIs (N=60) Lower RTIs (N=60) HRSVA n (%) HRSVB n (%) HRSVA n (%) HRSVB n (%) 2021 Spring 12 (10.0) 4 (6.7) 8 (13.3) 2 (3.3) 2 (3.3) 1 (1.7) 7 (11.7) Summer 15 (12.5) 3 (5.0) 12 (20.0) 0 (0.0) 3 (5.0) 1 (1.7) 11 (18.3) Autumn 4 (3.3) 2 (3.3) 2 (3.3) 1 (1.7) 1 (1.7) 0 (0.0) 2 (3.3) Winter 13 (10.8) 6 (10.0) 7 (11.7) 2 (3.3) 4 (6.7) 6 (10.0) 1 (1.7) 2022 Spring 12 (10.0) 10 (16.7) 2 (3.3) 6 (10.0) 4 (6.7) 2 (3.3) 0 (0.0) Summer 2 (1.7) 2 (3.3) 0 (0.0) 2 (3.3) 0 (0.0) 0 (0.0) 0 (0.0) Autumn 2 (1.7) 0 (0.0) 2 (3.3) 0 (0.0) 0 (0.0) 0 (0.0) 2 (3.3) Winter 19 (15.8) 5 (8.3) 14 (23.3) 3 (5.0) 2 (3.3) 10 (16.7) 4 (6.7) 2023 Spring 20 (16.7) 12 (20.0) 8 (13.3) 9 (15.0) 3 (5.0) 8 (13.3) 0 (0.0) Summer 4 (3.3) 2 (3.3) 2 (3.3) 2 (3.3) 0 (0.0) 0 (0.0) 2 (3.3) Autumn 4 (3.3) 2 (3.3) 2 (3.3) 1 (1.7) 1 (1.7) 0 (0.0) 2 (3.3) Winter 5 (4.2) 2 (3.3) 3 (5.0) 1 (1.7) 1 (1.7) 0 (0.0) 3 (5.0) Note: Spring includes March to May; Summer includes June to August; Autumn includes September to November; Winter includes December to February.
Abbreviation: ARTI= acute respiratory tract infection; RTI= respiratory tract infection; HRSV=Human respiratory syncytial virus;HRSVA/B=Human respiratory syncytial virus A/B.Table 3. Seasonal distribution of HRSV and HRSVA/B in children with ARTI in Shijiazhuang City, Hebei Province, China, 2021–2023.
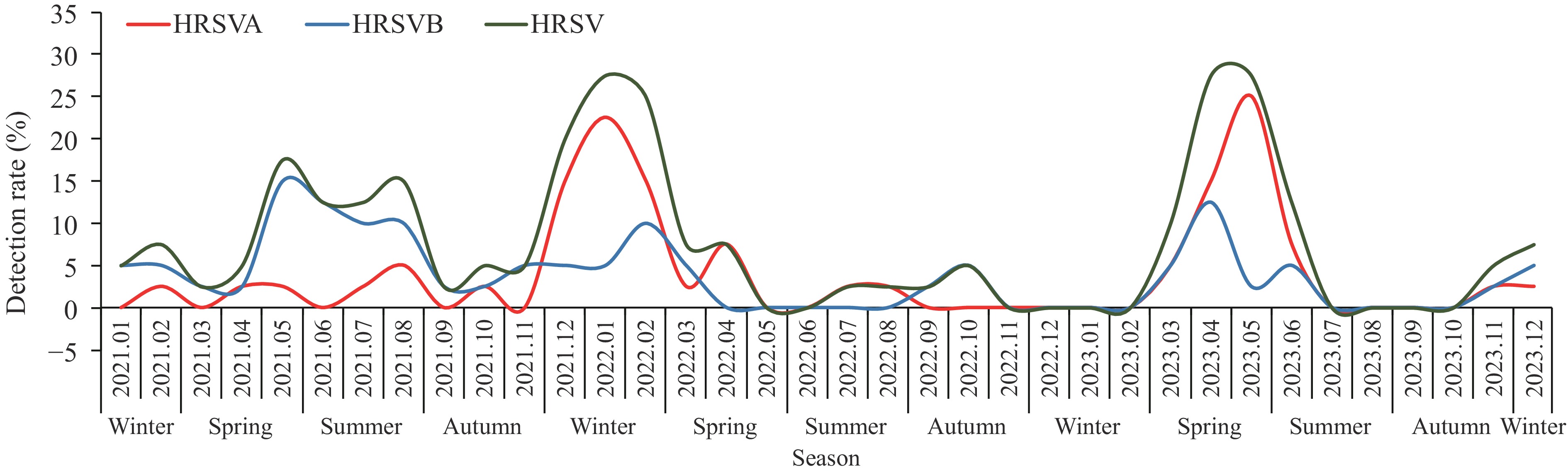 Figure 1.
Figure 1.Seasonal distribution of human respiratory syncytial virus subtypes in children with acute respiratory tract infections in Shijiazhuang City, Hebei Province, China.
Abbreviation: HRSV=Human respiratory syncytial virus; HRSVA/B=Human respiratory syncytial virus A/B.As age increased, the HRSV detection rate gradually decreased, with the highest detection rate in the 0–1 year group (13.9%), followed by the >1 to 2 years group (11.0%). The detection rate in the >2 to 5 years group is 9.5%, while the detection rate in the age group over 5 years old is the lowest (4.1%) (P<0.05). Additionally, the detection rate of lower RTIs in children in 0–2 years group (18.1%, 25/138) was much higher than the detection rate of upper RTIs in the same age group (8.1%, 18/223) (P<0.05). In patients who were in 0–2 years group, there was no significant difference in the detection rate of the HRSVA and HRSVB subtype in upper vs. lower (Table 4).
Age group (year) Detection rate Upper RTIs
(%)Lower RTIs
(%)HRSV-A HRSV-B Upper RTIs (%) Lower RTIs (%) Upper RTIs (%) Lower RTIs (%) 0 to 1 13.9 (16/115)* 9.2 (6/65)† 20.0 (10/50)† 6.62 (4/65)§ 12 (6/50)§ 3.1 (2/65)¶ 8 (4/50)¶ >1 to 2 11.0 (27/246)* 7.6 (12/158)† 17.5 (15/88)† 3.2 (5/158)** 6.8 (6/88)** 4.4 (7/158)†† 10.2 (9/88)†† >2 to 5 9.5 (44/463)* 8.8 (25/284) 10.6 (19/179) 5.6 (16/284) 4.5 (8/179) 3,2 (9/284) 6.1 (11/179) >5 to 14 4,1 (25/616)* 3.3 (7/213) 4.5 (18/403) 1.9 (4/213) 2.0 (8/403) 1.4 (3/213) 2.5 (10/403) * χ2=23.344, P<0.001;
† Total data for 0 to 1 year and >1 to 2 years groups: χ2=8.196, P=0.004;
§ χ2=0.592, P=0.442;
¶ χ2=0.568, P=0.451.
** χ2=1.015, P=0.314;
†† χ2=3.123, P=0.077.Table 4. Age distribution of HRSV in children with ARTIs in Shijiazhuang City, Hebei Province, China, 2021–2023.
-
This study analyzed 1,440 specimens collected from children under 14 years of age with ARTI in Shijiazhuang City, Hebei Province, China, between 2021 and 2023. The overall HRSV detection rate was 7.8% (112 positive specimens). A clear pattern of subtype dominance emerged, with HRSVB predominating throughout 2021, followed by HRSVA dominance during 2022 and the first half of 2023, demonstrating alternating subtype prevalence. While HRSV typically exhibits winter and spring seasonality, we observed an unusual summer epidemic in 2021. This out-of-season outbreak aligns with a globally observed phenomenon where HRSV cases initially decreased during the coronavirus disease in 2019 (COVID-19) pandemic restrictions but subsequently increased during non-typical seasons after the restriction relaxation (6-9). This pattern may be attributed to two key factors: the attenuation of pre-existing immunity to respiratory viruses during containment measures, and reduced maternal antibody transfer due to decreased maternal HRSV exposure, potentially increasing infant and young child susceptibility (10-11). Additionally, virus-virus interactions may influence HRSV’s epidemic dynamics and seasonality, highlighting the critical importance of maintaining continuous surveillance and early warning systems for effective HRSV prevention and control.
Our results demonstrated that HRSV detection rates were significantly higher in children under 5 years old (10.6%, 87/824) compared to those over 5 years old (4.1%, 25/616). Notably, in the 0–2 years age group, the detection rate was markedly higher in lower RTIs (18.1%) than upper RTIs (8.1%), indicating that infants and young children represent the primary susceptible population for HRSV infection. No significant differences were observed in the detection rates between HRSVA and HRSVB subtypes across upper and lower RTIs. Following HRSV infection, infants and young children are particularly prone to developing severe complications such as bronchiolitis and pneumonia. Compared to single HRSV infections, children with poly-viral RTIs exhibited more severe clinical manifestations, including higher fever incidence, prolonged fever duration, and extended hospital stays. The observation that HRSV coinfections with other viruses were exclusively detected in lower RTI cases suggests that viral coinfections may significantly influence disease severity and progression, warranting careful monitoring of pediatric HRSV cases. Non-pharmacological interventions (NPIs) during HRSV seasons, including social distancing, mask-wearing, and hand hygiene, remain crucial strategies for preventing pediatric RTIs (12). The implementation of NPIs during the COVID-19 pandemic substantially altered HRSV epidemiological patterns in Hebei Province. Pre-pandemic HRSV detection rates of approximately 17% dropped to less than 1% following strict NPI implementation. The traditional autumn-winter prevalence pattern shifted, with an unusual summer outbreak occurring in 2021. Following the relaxation of NPIs in 2022, the epidemic peak showed significant temporal displacement, appearing during winter and spring, demonstrating the strong correlation between HRSV prevalence and NPI measures. This study revealed that HRSV predominantly affects children under 5 years old in the Shijiazhuang area, with peak prevalence during spring and winter. The 0–2 years age group showed higher detection rates in the lower respiratory tract specimens compared to upper respiratory specimens. For effective HRSV prevention, particularly in high-risk infants and young children, comprehensive measures are essential: maintaining proper hand hygiene, implementing respiratory isolation protocols, promoting breastfeeding, avoiding exposure to tobacco smoke, and improving living conditions. Additionally, children should avoid crowded spaces and wear masks in public settings. Healthcare providers should wear masks when exhibiting upper RTI symptoms, and strict adherence to hand hygiene protocols and personal protective equipment use in medical facilities is crucial to prevent nosocomial transmission. While vaccination represents a critical preventive strategy against HRSV, currently no approved vaccines exist in China for pediatric HRSV prevention. However, with vaccines becoming available internationally, active immunization against HRSV in children aged 0–2 years represents a promising future prevention strategy.
-
Received ethics approval from the Institutional Ethics Committee for Research of Institutional Review Board of the Institute for Viral Disease Control and Prevention, Chinese Center for Disease Control and Prevention (No.IVDC2018(012)).
HTML
| Citation: |



 Download:
Download:




