-
Mpox is a zoonotic viral infection transmitted through contact with bodily fluids, skin, or mucosal lesions, respiratory droplets, and contaminated objects (1). By the end of 2023, the 2022–2023 global mpox outbreak had resulted in 93,030 laboratory-confirmed cases (2). The first imported case in China was reported in Chongqing municipality in September 2022 (3). In response to emerging local transmission, the National Disease Control and Prevention published the Guideline on Mpox Prevention and Control in July 2023, and subsequently classified mpox as a category B notifiable communicable disease in September.
People with human immunodeficiency virus (PWH) have been disproportionately affected by mpox, with the World Health Organization (WHO) reports that 52.1% of mpox cases with known HIV status were PWH (2). This association stems from two key factors. First, sexual contact has been frequently implicated in mpox transmission (4). Men who have sex with men (MSM), who constitute the predominant affected population in the current global mpox outbreak (5), are also a key population in HIV transmission. Second, PWH may be more vulnerable to mpox infection and experience more severe symptoms and clinical outcomes due to immunological deficiency (6). Given these overlapping transmission routes and the potential for adverse prognosis, coordinated efforts to control HIV and mpox coinfection warrant particular attention. This study aimed to analyze the epidemiological characteristics and clinical symptoms of mpox cases reported in China during 2023, compare outcomes between those with and without HIV, and provide evidence to support integrated prevention and control strategies for both infections.
-
This study encompassed all laboratory-confirmed mpox cases reported in China during 2023. Data were collected from two primary sources: the internet-based National Infectious Diseases Reporting System and the National HIV/AIDS Case Reporting System. Cases were linked across systems a using unique identification numbers, with all personally identifiable information removed during data processing. The collected data included demographic characteristics (gender, occupation, age), residence code (categorized into eastern, central, and western regions based on geographical distribution and economic development), and reporting dates for both mpox and HIV diagnoses. For HIV-positive cases, additional clinical parameters were collected, including antiretroviral therapy (ART) status, recent HIV RNA copies/mL, and CD4+T lymphocytes (CD4) count within 6 months before or after mpox diagnosis, as recorded by the end of 2023. Clinical symptoms at diagnosis and behavioral information was extracted from epidemiological investigations. Participants who reported male homosexual behaviors in either mpox or HIV investigations were classified as MSM. Statistical analyses were performed using SPSS (version 24.0, IBM Corp., Armonk, NY, USA) and Excel 2019 (Microsoft Corp., WA, USA). Differences between HIV-positive and HIV-negative groups were assessed using t-test and chi-square test, with statistical significance set at P<0.05.
-
Among the 1,712 confirmed mpox cases reported in 2023, 802 (46.8%) were PWH. Of the 10 reported female cases, none were HIV positive. Among the 1,702 male cases, 94.0% self-identified as MSM. The mean age of male cases was 33.0±7.2 years, with 83.7% under 40 years old. PWH was significantly older than those without HIV (34.6±6.9 years vs. 31.7±7.2 years, t=8.419, P<0.001). The proportion of PWH among mpox cases was lower in the Eastern region compared Central and Western regions (Table 1).
Variable Total
(N=1,702)With HIV
(N=802)Without HIV
(N=900)Comparisons between those with and without HIV Chi-square P MSM, n (%) Yes 1,600 (94.0) 780 (97.3) 820 (91.1) 28.432 <0.001 No 102 (6.0) 22 (2.7) 80 (8.9) Age group, n (%) 15–29 652 (38.3) 226 (28.2) 426 (47.3) 69.542 <0.001 30–39 774 (45.5) 411 (51.2) 363 (40.3) 40–49 238 (14.0) 143 (17.8) 95 (10.6) ≥50 38 (2.2) 22 (2.7) 16 (1.8) Geographical, n (%) Eastern 1,157 (68.0) 515 (64.2) 642 (71.3) 14.025 <0.001 Central 268 (15.7) 153 (19.1) 115 (12.8) Western 277 (16.3) 134 (16.7) 143 (15.9) Detection routes, n (%) Hospital visits 1,528 (89.8) 718 (89.5) 810 (90.0) 0.705 0.703 Close contacts 84 (4.9) 38 (4.7) 46 (5.1) Other 90 (5.4) 46 (5.6) 44 (4.9) Risk behaviors most likely to cause infection during 21 days preceding symptom onset, n (%) Sex activities with men 1,421 (83.5) 658 (82.0) 763 (84.8) 5.209 0.157 Sex activities with women 19 (1.1) 7 (0.9) 12 (1.3) Non-sexual close contacts 4 (0.2) 1 (0.1) 3 (0.3) Declined to disclose 258 (15.2) 136 (17.0) 122 (13.5) Abbreviation: HIV=human immunodeficiency virus; MSM=men who have sex with men. Table 1. Demographics and epidemiological characteristics of male mpox cases with and without HIV in China.
Hospital-based detection accounted for 93.0% of male mpox cases, with no significant differences between HIV-positive and HIV-negative groups. Among 1,444 cases with available exposure history data, sexual contact with men within 21 days before symptom onset was reported by 98.7% of PWH and 98.1% of HIV-negative cases, though some participants also reported heterosexual contact. Of the 1,274 individuals who provided information about sexual partners, 69.7% reported one partner, 26.7% reported two to four partners and 3.6% reported five or more partners. HIV-negative individuals were more likely to report multiple sexual partners compared to PWH (32.9% vs. 27.1%, χ2=4.925, P=0.026).
The predominant clinical manifestations at diagnosis included rash (92.2%), fever (53.2%), lymphadenopathy (24.7%), headache (9.6%), and proctitis (8.3%). The Anogenital rash was reported in 53.1% of cases. No significant differences were observed in cardinal symptoms between individuals with and without HIV, including rash (90.9% vs. 93.4%, χ2=3.845, P=0.050), fever (52.5% vs. 53.8%, χ2=0.281, P=0.596), and lymphadenopathy (23.8% vs. 25.4%, χ2=0.605, P=0.437) (Figure 1).
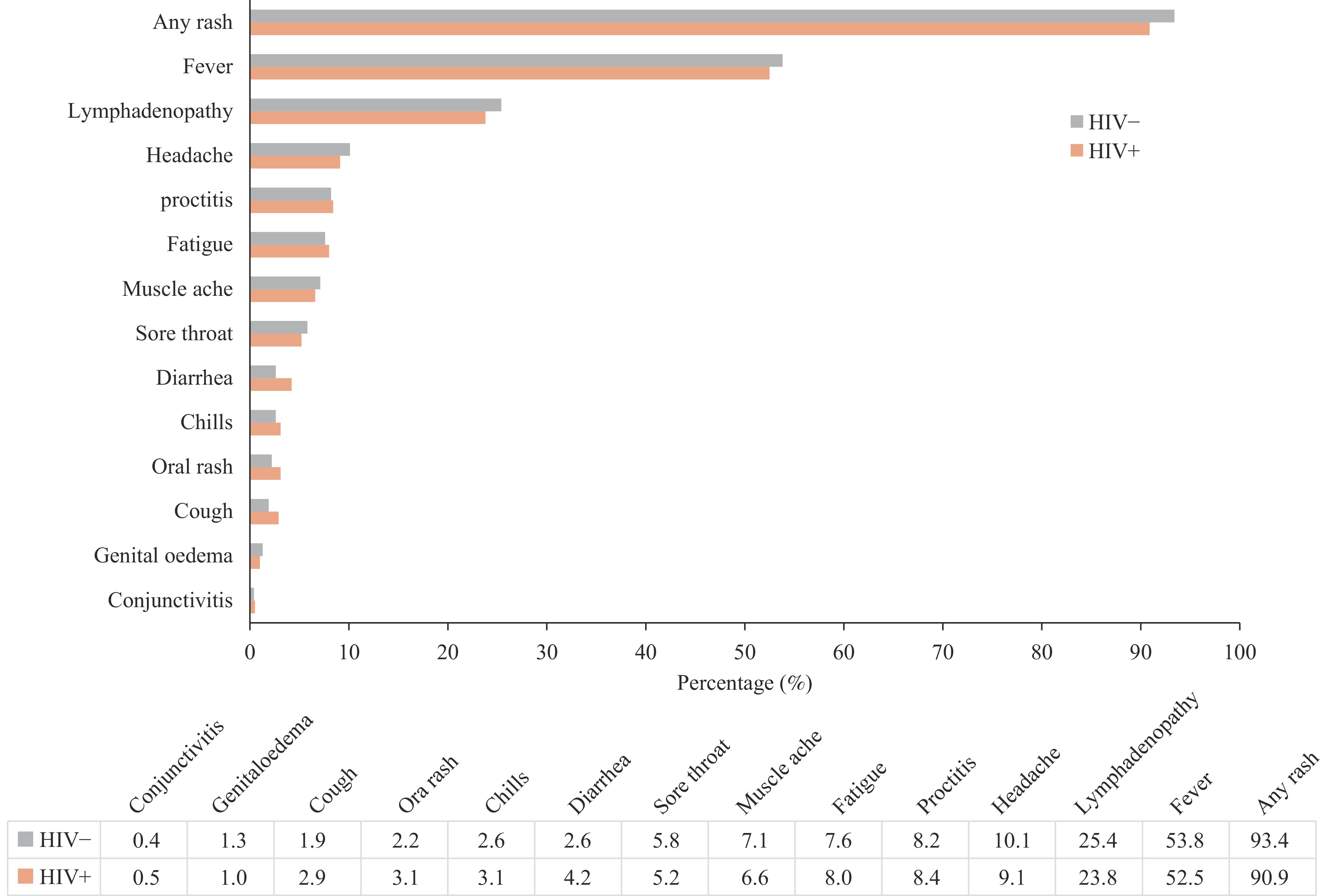 Figure 1.
Figure 1.Clinical symptoms at diagnosis among male mpox cases with and without HIV. (n=1,702)
Abbreviation: HIV=human immunodeficiency virus.Analysis of clinical characteristics among mpox and HIV coinfections were stratified by time from HIV to mpox diagnosis (Table 2). Among 802 coinfected cases, 673 (98.4%) were diagnosed with mpox more than one year after HIV diagnosis, 61 (7.6%) within one year following HIV diagnosis, and 57 (7.1%) were diagnosed with HIV after mpox. By the end of 2023, ART coverage reached 96.6% (775/802) among coinfected patients; however, the initiation rate was markedly lower (78.9%) among those diagnosed with HIV after mpox. Of those on ART, 606 (78.2%) had recent viral load results available, with 517 (85.3%) achieving viral suppression (VL<50 copies/mL). Notably, viral suppression rates were substantially lower among those diagnosed with HIV after mpox (24.3%) or within one year before mpox (65.4%). Among 652 cases with recent CD4 count data, 77 (11.8%) exhibited severe immunodeficiency (CD4 count <200 cells/μL). The proportion of severe immunodeficiency was notably higher in cases where HIV was diagnosed after mpox or within one year before mpox.
Variable Total (n=802) Time from HIV diagnosis to mpox diagnosis >1 year (n=684) ≤1 year (n=61) HIV after mpox (n=57) Antiretroviral therapy Yes 775 (96.6) 673 (98.4) 57 (93.4) 45 (78.9) No 27 (3.4) 11 (1.6) 4 (6.6) 12 (21.1) Recent HIV load (copies/mL) 1–50 517 (85.3) 474 (91.7) 34 (65.4) 9 (24.3) 50–1,000 32 (5.3) 20 (3.9) 6 (11.5) 6 (16.2) >1,000 57 (9.4) 23 (4.4) 12 (23.1) 22 (59.5) Recent CD4 count (cells/μL) 0–199 77 (11.8) 43 (7.9) 20 (36.4) 14 (28.0) 200–349 92 (14.1) 63 (11.5) 15 (27.3) 14 (28.0) 350–500 141 (21.6) 121 (22.1) 8 (14.5) 12 (24.0) >500 342 (52.5) 320 (58.5) 12 (21.8) 10 (20.0) Note: Data on HIV viral load and CD4 count were not available for all cases.
Abbreviation: HIV=human immunodeficiency virus.Table 2. Clinical characteristics of HIV and mpox coinfected cases by time of HIV diagnosis.
-
MSM represent the predominant demographic affected by mpox in China, aligning with global epidemiological patterns (7). National representative studies conducted in 2022 revealed significant knowledge gaps regarding mpox among both HIV-positive and general MSM populations, particularly concerning transmission routes, susceptible populations, and preventive measures (8-9). This combination of limited awareness and frequent high-risk behaviors have rendered MSM particularly vulnerable to mpox infections. However, the risk of mpox infection is not exclusive to males, as evidenced by ten confirmed female cases and reports of heterosexual transmission among male cases.
The 15–39 age group bears the highest burden of mpox infections, attributable to both their sexual activity patterns and lack of smallpox vaccination following its global eradication.
The absence of significant differences in cardinal symptoms at diagnosis between individuals with and without HIV is likely attributed to China’s high ART coverage among PWH. This finding parallels the research from Poland, where no significant clinical differences or complication rates were observed between mpox cases with and without HIV, with 97.7% of HIV-coinfected cases receiving ART (10). Previous research indicates that PWH is experiencing severe disease typically were either not receiving ART or presented with late-stage HIV (5,11). However, symptom analysis in this study was limited to the initial patient complaints at diagnosis, lacking comprehensive follow-up data on disease progression and detailed clinical examinations. Analysis of hospitalized mpox patients in Beijing revealed that some PWH developed severe complications, including pneumonia, bacterial peritonitis, and intestinal obstruction (12). Additionally, Nigerian reports indicate that PWH typically experience longer disease duration compared to HIV-negative individuals (13).
The epidemiological analysis yields several critical implications for mpox epidemic control. First, targeted knowledge dissemination regarding mpox prevention among key populations, particularly MSM, is essential. This can be achieved through expanded educational initiatives utilizing social media platforms and innovative communication channels to enhance understanding of self-prevention measures. Additionally, given that mpox transmission occurs through close contact, broader public health awareness campaigns are equally crucial. Second, surveillance and case detection capabilities require further strengthening. While this study found that most mpox cases were identified through hospital visits, research indicates that only 49.3% of cases are diagnosed during initial hospital presentation (14). Therefore, focused training for healthcare professionals in dermatology, anorectal medicine, and genitourinary departments could significantly improve case identification and diagnosis rates.
The coinfected cases reveal concerning patterns of late HIV diagnosis and ongoing transmission risk. The finding that approximately 3% of coinfected patients were unaware of their HIV status at mpox diagnosis, combined with low CD4 counts indicating late presentation, suggests persistent gaps in HIV testing awareness and utilization among sexually active MSM. Current HIV sentinel surveillance data shows that only 61.2% of MSM in China had undergone HIV testing and knew their status in the past year (15). These findings underscore the urgent need to expand HIV testing coverage and improve early detection strategies among MSM populations in China. For mpox cases with HIV coinfection, prioritizing ART initiation and adherence is crucial, particularly for those who have not yet achieved viral suppression.
The findings underscore the necessity of integrating HIV and mpox surveillance and prevention efforts among high-risk populations, particularly MSM. This integration should occur across three key domains: First, health promotion and behavioral interventions for both mpox and HIV should be combined to enhance risk perception among key populations. Mpox education and intervention strategies can be effectively incorporated into existing HIV services, including voluntary counseling and testing, follow-up care, and ART for PWH. Second, HIV screening should be prioritized for individuals being evaluated for mpox with unknown HIV status, with appropriate follow-up testing to exclude window period infections when initial results are negative. Third, when PWH is diagnosed with mpox, comprehensive consultations should address ongoing HIV transmission risk through strategies such as promoting consistent condom use, ensuring ART adherence, and facilitating timely HIV screening or post-exposure prophylaxis for sexual partners.
This research presents the first national epidemiological profile of mpox and HIV coinfection in China, documenting both epidemiological characteristics and clinical symptoms. However, several limitations warrant consideration. First, the analysis relies on surveillance system data, and mpox cases may be underreported due to its typically self-limiting nature and mild symptomatology. Second, exposure history and symptom data were collected through self-reporting at diagnosis, introducing potential information bias. Despite these limitations, this research provides valuable insights for developing integrated approaches to prevent and control both infections.
-
The authors would like to thank all the staff who participated in the prevention and control of AIDS and mpox. Especially, efforts of Qianqian Qin is appreciated, who has made equal contributions with the first author of this article.
HTML
| Citation: |



 Download:
Download:




