-
Approximately 1,000 species of mushrooms are estimated to be poisonous worldwide (1). As many as 480 poisonous mushroom species have been reported in China (2). However, foraging, trading, and consuming wild mushrooms is a tradition in China. Poisonous and edible mushrooms with highly similar morphologies often grow in the same wild habitats, increasing the risk of accidental ingestion. Following a suspected poisoning, collecting and effectively detecting and identifying residual mushroom specimens or human biological samples (blood, urine, vomit, gastric lavage, etc.) during epidemiological investigations is crucial for diagnosis and treatment.
Between 2012 and 2023, the “Public Health Emergency Reporting and Management Information System” of the China CDC documented 653 mushroom poisoning incidents, including 3,229 poisoning cases and 710 deaths, which accounted for 21.87% (653/2,986) of reported foodborne poisoning incidents, 4.33% (3,229/74,586) of the poisonings, and 54.20% (710/1,310) of foodborne poisoning deaths. The fatality rate was 21.99% (710/3,229). From 2012 to 2020, the fatality rate showed minor fluctuations, peaked in 2020, and decreased significantly after 2022. Among all incidents, 551 (84.38%) lacked laboratory evidence of mushroom species identification, with causation determined through epidemiological investigation and clinical manifestations of poisoning. Detection and identification of poisonous mushrooms were conducted in 102 incidents (15.62%); however, 10 of these lacked test and identification results in their final reports, leaving 92 incidents (14.08% of total cases) with complete toxicological test or identification results.
Between 2012 and 2023, detection and identification results of poisonous mushroom incidents were available for all years except 2014. The number of mushroom poisoning incidents with detection and identification results was lowest in 2013 with only 1 incident, and highest in 2017, accounting for 22.83% (21/92) (Figure 1). A total of 13 provincial-level administrative divisions (PLADs) participated in detection and identification, with the top 5 PLADs by number of detection incidents being Hunan, Yunnan, Guangdong, Sichuan, and Guizhou, reporting 25 (27.17%), 22 (23.91%), 17 (18.48%), 9 (9.78%), and 6 (6.52%) incidents, respectively. Additionally, Guangxi and Fujian PLADs each reported 3 incidents with detection and identification results; Zhejiang PLAD reported 2; and Chongqing, Shandong, Hubei, Hebei, and Hainan PLADs reported 1 for each.
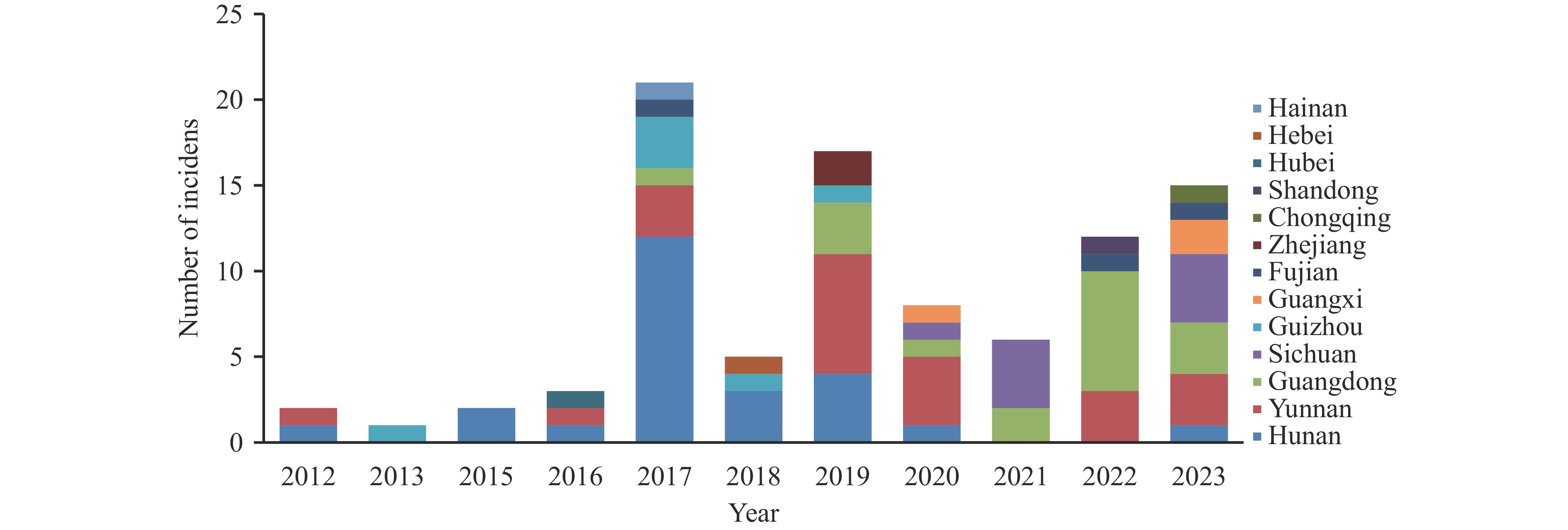 Figure 1.
Figure 1.The years and PLADs distribution of detection and identification for mushroom poisoning reported incidents in China, 2012–2023.
Abbreviation: PLAD=provincial-level administrative division.The departments involved in the detection and identification of mushroom poisoning incidents were CDCs, universities, multi-department collaborations (including public security and agriculture), scientific research institutes, and hospitals, with composition ratios of 63.04%, 16.30%, 9.78%, 6.52%, and 4.35%, respectively. The detection methods included morphological identification, molecular biology detection, toxin detection, acute toxicity tests on animals, and combinations of these methods. Morphological identification, including that of high-definition photographs, was the most common (3), accounting for 60.87% of mushroom poisoning incidents with detection and identification results. This was followed by molecular biology detection and toxin detection, accounting for 13.04% and 11.96%, respectively (Table 1).
Detection methods Number of incidents Proportion (%) Morphological identification 31 33.70 Morphological identification of mushroom’s photograph 25 27.17 Molecular biology detection 12 13.04 Toxin detection 11 11.96 Morphological identification and toxin detection 4 4.35 Morphological identification and molecular biology detection 3 3.26 Toxin detection and molecular biology detection 2 2.17 Acute toxicity tests on animals 2 2.17 Morphological identification of mushroom’s photograph and toxin detection 1 1.09 Morphological identification of mushroom’s photograph and acute toxicity tests on animals 1 1.09 Total 92 100.00 Table 1. Distribution of toxicant detection methods with identification results from 2012 to 2023.
The distribution of detection and identification methods varied among the top 5 PLADs. In Hunan, 22 (88.00%), 2 (8.00%), and 1 (4.00%) incidents were identified by morphological identification, methods with two detection types, and acute toxicity tests on animals, respectively. In Yunnan, the numbers of incidents identified by morphological identification, toxin detection, molecular biology detection, and methods with two detection types were 8 (36.36%), 6 (27.27%), 4 (18.18%), and 4 (18.18%), respectively. In Guangdong, the numbers identified by morphological identification, methods with two detection types, and toxin detection were 10 (58.82%), 4 (23.53%), and 3 (17.65%), respectively. In Sichuan, the numbers identified by morphological identification and molecular biology tests were 5 (55.56%) and 4 (44.44%), respectively. In Guizhou, the numbers identified by morphological identification, molecular biology detection, and methods with two detection types were 3 (50.00%), 2 (33.33%), and 1 (16.67%), respectively.
Among the 92 mushroom poisoning incidents that reported toxicological detection and identification results (4–5), the most frequent incidents and poisonings involved acute liver failure, rhabdomyolysis, gastroenteritis, psycho-neurological disorders, and acute renal failure. Acute liver failure caused the most deaths, accounting for 55.17% (64/116) of all clinical types of mushroom poisoning. Twenty-five species were involved in the 92 mushroom poisoning incidents. Amanita exitialis and Russula subnigricans were responsible for the most incidents, both of which accounted for 17.39% (16/92) of all species. Amanita exitialis is the most prevalent type of mushroom with acute liver failure. The number of poisonings and the deaths attributed to A.exitialis accounted for 13.32% (55/413) and 16.38% (19/116) of all identified mushroom poisonings, respectively. Amanita fuliginea caused the largest number of deaths, accounting for 18.10%(21/116) (Table 2).
Clinical classifications Mushroom (or toxin) species Number of incidents Number of patients Deaths Fatality (%) Acute liver failure 41 162 64 39.51 Amanita exitialis 16 55 19 34.55 Amanita fuliginea 13 50 21 42.00 Amanita rimosa 4 13 6 46.15 Anmanita fuligineoides 2 18 8 44.44 Amanita sp. 2 5 3 60.00 Anmanita subpallidorosea 1 8 4 50.00 Galerina autumnalis 1 6 1 16.67 Galerina sp. 1 4 1 25.00 Galerina sulciceps 1 3 1 33.33 Rhabdomyolysis 16 52 20 38.46 Russula subnigricans 16 52 20 38.46 Gastroenteritis 9 44 4 9.09 Chlorophyllum molybdites 3 9 1 11.11 Russula japonica 2 17 0 0.00 Scleroderma 1 9 2 22.22 Chlorophyllum globosum 1 5 0 0.00 Russula laurocerasi 1 2 1 50.00 Scleroderma cepa 1 2 0 0.00 Psycho-neurological disorder 7 33 4 12.12 Amanita subglobosa 3 17 2 11.76 Amanita subfrostiana 1 7 1 14.29 Amanita parvipantherina 1 3 1 33.33 Amanita sychnopyramis 1 3 0 0.00 Gymnopilus dilepis 1 3 0 0.00 Acute renal failure 2 25 4 16.00 Amanita pseudoporphyria 2 25 4 16.00 Psycho-neurological disorder
and acute renal failure1 2 1 50.00 Amanita oberwinklerana and
Psathyrella candolleana1 2 1 50.00 Mixed class 3 21 3 14.29 More than 2 clinical types 3 21 3 14.29 Amatoxins 11 67 12 17.91 Unclassified 2 7 4 57.14 Unknown species that
causes animal death2 7 4 57.14 Total 92 413 116 28.09 Table 2. Distribution of species in poisonous mushroom incidents with poison detection and identification results from 2012 to 2023.
-
China CDC’s “Public Health Emergency Reporting Management Information System” is a national public health emergency network direct reporting data platform based on public health event reporting. According to mushroom poisoning incidents reported by the platform, the number of incidents showed an upward trend from 2012 to 2017 and decreased significantly in 2018. A downward trend after an increase from 2019 to 2020, and an increase from 2021 to 2023. From 2012 to 2023, these incidents accounted for 21.87% of all foodborne poisoning incidents and 4.33% of all foodborne poisonings, but 54.20% of all foodborne poisoning deaths, indicating that poisonous mushrooms are a major cause of deaths in foodborne poisoning incidents. Meanwhile, the case fatality rate for mushroom poisoning incidents is as high as 21.99%. This differs from the 2.17% case fatality rate in mushroom poisoning cases collected by platforms using multiple communication methods, such as WeChat, phone, and email (6), and the 2.0% case fatality rate in China’s Foodborne Disease Outbreak Surveillance System between 2010 and 2020 (7). This discrepancy arises because the public health emergency network direct reporting data platform only reports incidents involving more than 3 people or deaths, resulting in a smaller denominator for calculating the case fatality rate than the actual number of poisoning cases. Regardless of the surveillance method, deaths from mushroom poisoning incidents accounted for the highest proportion of deaths among foodborne poisonings.
The number of mushroom poisoning incidents with confirmed species identification followed the same trend as the total number of incidents from 2012 to 2019, but the trend increased after 2021. This may be related to increasing numbers of poisonous mushrooms being sent to laboratories with testing capabilities via the WeChat platform (3).
Because CDCs are responsible for the epidemiological investigation of incidents, they can obtain remaining mushroom samples or biological samples (such as vomitus). CDCs are the primary organizations for detecting and identifying mushroom poisoning incidents. Scholars in universities and research institutes conducting fundamental research on fungal classification can provide technical support for mushroom species determination. The advantages of different detection and identification institutions vary, but current data show that multi-department cooperation accounts for only 9.78%. Multi-department cooperation can serve as a future direction for poisonous mushroom detection and identification.
According to the report, 84.38% of mushroom poisoning incidents lacked laboratory testing evidence of the poison type, while before 2014, this figure was 92.59% (8). Besides the objective difficulties in specimen collection, the severe lack of detection capacity is another important factor. Although numerous methods exist for detecting poisonous mushrooms, such as morphological identification, molecular biology identification, toxin detection, and animal toxicity testing, each has its own scope, advantages, and disadvantages. Morphological identification requires experienced fungal taxonomists to identify macro and micro structures, and the morphology needs to remain intact. At the incident scene, collecting incomplete poisonous mushrooms or edible residues is common. Molecular biology methods can identify damaged poisonous mushroom samples but struggle with samples subjected to high-temperature cooking. Toxin detection can directly reflect the toxic exposure of poisoned patients, but many poisonous mushroom toxins remain undiscovered, and detection requires expensive, specialized equipment. Animal toxicity testing can elucidate toxicity mechanisms; acute toxicity tests can quickly reflect toxicity levels but cannot confirm the poison type. Many poisonous mushrooms and toxins remain unknown, necessitating continued development of rapid detection and identification methods for poisonous mushrooms and toxins, and further toxication-related research.
In Hunan Province, morphological identification was the predominant method (88.00%) among the 13 PLADs. Yunnan Province had the highest proportion of toxin detection (27.28%). However, Sichuan and Guizhou provinces used molecular biology detection rather than toxin detection. Yunnan Province employed the widest variety of detection and identification methods, possibly correlating with its higher incidence of mushroom poisoning.
Determining the species of poisonous mushroom allows early understanding of its pathogenic characteristics, enabling appropriate symptomatic treatment. For example, after ingesting a mushroom causing acute liver failure, symptoms may resolve after initial treatment, creating a "false healing period." This can lead patients, their families, and clinicians to underestimate the severity of the condition and miss the optimal window for life-saving interventions. Species identification enables early targeted organ support, reduces toxin absorption, and promotes toxin elimination.
As morphological identification is the most common method, factors such as whether the remaining mushrooms and the ingested mushrooms are the same species, the morphological integrity of the mushrooms, and the cooking method affect detection and identification. Therefore, the public should take high-resolution photographs before consumption. Furthermore, morphological identification requires extensive professional training, molecular biology detection requires specialized facilities, and toxin detection necessitates advanced instrumentation and expertise. Clinical doctors should collaborate and undergo regular training and exchanges with professionals in mushroom detection and identification to improve detection, identification, and control.
Some scholars analyzed poisonous mushroom species reported in 98 poisoning incidents from 2004 to 2011, identifying 22 species (9). This paper analyzed incident reports from 2012 to 2023, with 25 species identified in 92 incidents. Both analyses showed acute liver failure and rhabdomyolysis as the primary lethal types. Amanita exitialis,Amanita fuliginea and Russula subnigricans require particular attention. Gastroenteritis and neuropsychiatric types have also resulted in fatalities, despite rarely being lethal. This may be related to complications during treatment, underlying patient conditions, or ingestion of other undetected, highly toxic species.
The study has the following limitations: First, the mushroom poisoning incident in the Public Health Emergency Reporting Management Information System did not include data on mushroom poisoning cases, and many sporadic cases of hospital visits were not collected. In addition, during the epidemiological investigation of suspected mushroom poisoning, there were no remaining mushrooms, and the inability to carry out detection restricted the discovery of the types of poisoned mushrooms. Finally, testing to see if the mushrooms identified are the same species as those eaten by the patient adds complexity to the analysis.
Concurrently, the clinical manifestations of mushroom poisoning are complex and diverse, and no standard treatment exists (10). Prevention remains the most economical and straightforward control measure. Increased health education and public awareness initiatives are necessary.
HTML
| Citation: |



 Download:
Download:




