-
Vaginitis, a prevalent infectious gynecological condition, is primarily caused by bacterial pathogens, Trichomonas vaginalis, and Candida species. While highly treatable, it exhibits significant incidence and recurrence rates (1). Chronic infections can adversely affect menstrual health, fertility, and pregnancy outcomes, impacting women’s physical and mental well-being, quality of life, and intergenerational health (2–3). Despite these implications, comprehensive epidemiological data on vaginitis remains limited. A large-scale survey across five provinces, encompassing 37,353 participants, revealed a vaginitis prevalence of 32.2% (12,029 cases), with 88.8% of affected individuals seeking treatment from professional medical institutions. The highest prevalence was observed among women aged 35–54 years and those reporting poor self-rated health, indicating a substantial disease burden. Notably, awareness of cervical cancer screening policies emerged as a potential protective factor against vaginitis. Conversely, women who participated in screenings for common gynecological diseases demonstrated higher vaginitis prevalence, suggesting that screening programs facilitate improved detection and diagnosis. These findings underscore the importance of enhancing health literacy and implementing targeted interventions for both prevention and early detection of gynecological conditions to advance women’s health outcomes.
A cross-sectional survey was conducted in July 2023 across five provinces (Sichuan, Yunnan, Hubei, Fujian, and Shandong), selected from western, central, and eastern China and successful implementation of women’s health screening programs. Using multi-stage stratified random sampling, 12 communities or villages were selected from each province, yielding 60 study sites. Local grid managers, who possessed detailed knowledge of resident populations, were trained as surveyors and administered questionnaires to women aged 18–74 years after obtaining informed consent. The structured online questionnaire captured data on sociodemographic characteristics, behavioral habits, self-rated health status, awareness of screening policies, and participation in common disease screenings. Vaginitis cases were identified through participant-reported clinical diagnoses from medical institutions. From 37,917 collected questionnaires, 37,353 were deemed valid (98% validity rate) after excluding duplicates and low-quality responses.
Statistical analysis comprised descriptive statistics for variable characterization and chi-squared tests to evaluate associations between biobehavioral factors and vaginitis infection. Variables demonstrating significance (P<0.01) in chi-squared analysis, along with demographic variables, were incorporated into multivariable logistic regression models to control for potential confounding factors. To ensure robust assessment of factor impacts on vaginitis infection, two sensitivity analysis models were developed: Model 1 analyzed diagnosed vaginitis cases (n=12,029) as the outcome variable, while Model 2 focused on cases treated at professional medical institutions (n=10,682). All analyses were performed using RStudio (version 2023.06.2+561, Posit, PBC, Boston, MA, USA).
Among the study participants, 54% were urban residents (Table 1). The sample demonstrated broad representation across educational backgrounds, occupations, and income levels. Based on established research, data collection encompassed pregnancy history, smoking status, alcohol consumption, physical and mental health status, awareness of cervical cancer screening policies, and participation in women’s common disease screening programs. Chi-squared analyses revealed significant associations (P<0.001) between all examined factors and vaginitis prevalence. Sensitivity analysis using Model 2 (patients receiving professional treatment) validated the findings from Model 1 (diagnosed vaginitis cases).
Characteristics Total Model_1_Vaginitis Diagnosis Model Model_2_Medical Institution Treatment Model Disease group (%)
n=12,029Non-disease group
(%) n=25,324P Disease group (%)
n=10,682Non-disease group
(%) n=26,671P* Age (year) <0.001 <0.001 18–34 13,641 23.1 42.9 23.8 41.6 35–54 19,902 67.3 46.6 67.0 47.8 55–74 3,810 9.6 10.5 9.3 10.6 BMI (kg/m2) <0.001 <0.001 <18.5 2,691 4.3 8.6 4.5 8.3 18.5–24 26,399 71.7 70.2 71.9 70.2 24–28 7,047 20.7 18.0 20.5 18.2 ≥28 1,216 3.2 3.3 3.1 3.3 Region <0.001 <0.001 Shandong 7,933 17.3 23.1 16.6 23.1 Fujian 7,235 16.2 20.9 16.8 20.4 Hubei 6,945 23.8 16.1 23.7 16.5 Sichuan 7,565 20.2 20.3 20.2 20.3 Yunnan 7,675 22.4 19.6 22.7 19.7 Area type <0.001 <0.001 Rural 16,976 43.8 46.2 42.8 46.5 Urban 20,377 56.2 53.8 57.2 53.5 Marital Status <0.001 <0.001 Unmarried 7,748 9.1 26.3 8.9 25.5 Married 29,605 90.9 73.7 91.1 74.5 Education background <0.001 <0.001 Bachelor and above 8,658 19.2 25.1 20.1 24.4 Junior college 8,095 20.6 22.2 21.1 21.9 High school 7,785 23.2 19.7 23.2 19.9 Middle school 9,946 29.7 25.2 28.7 25.8 Primary school 2,869 7.3 7.9 6.9 8.0 Career <0.001 <0.001 Government officials 6,451 18.5 16.7 19.0 16.6 Private enterprise personnel 2,948 8.4 7.7 8.6 7.6 Managers in non-civil service system 1,552 4.7 3.9 4.7 3.9 Individual Merchants/freelancers 11,593 31.1 31.0 31.5 30.8 Farmers/migrant workers 8,813 23.8 23.5 22.8 23.9 Unemployed 3,165 9.2 8.1 9.2 8.2 Retired 464 1.9 0.9 1.8 1.0 Student 1,765 0.7 6.6 0.6 6.4 Other 602 1.7 1.6 1.7 1.6 Annual household income <0.001 <0.001 <30 thousand 16,339 41.6 44.8 40.2 45.2 30–80 thousand 12,596 34.8 33.2 35.2 33.1 ≥80 thousand 8,418 23.6 22.0 24.5 21.7 Number of pregnancies <0.001 <0.001 0 7,430 5.1 26.9 5.1 25.8 1–2 20,404 55.4 54.3 55.3 54.4 ≥3 9,519 39.5 18.8 39.5 19.9 Smoking <0.001 <0.001 No 36,079 96.0 96.9 96.0 96.8 Yes 1,274 4.0 3.1 4.0 3.2 Drinking <0.001 <0.001 No 25,893 61.2 73.2 60.9 72.7 Yes 11,460 38.8 26.8 39.1 27.3 Self-assessed physical health <0.001 <0.001 Good 25,204 55.8 73.0 56.1 72.0 Ordinary 11,248 40.5 25.2 40.2 26.1 Poor 901 3.7 1.8 3.6 1.9 Self-assessed mental health <0.001 <0.001 Good 28,349 68.1 79.6 68.2 79.0 Ordinary 8,357 29.5 19.0 29.5 19.5 Poor 647 2.4 1.4 2.3 1.5 Family cancer status <0.001 <0.001 No 37,090 98.9 99.5 98.8 99.5 Yes 263 1.1 0.5 1.2 0.5 Aware of cervical cancer screening policies No 6,601 14.1 19.4 13.8 19.2 Yes 30,752 85.9 80.6 86.2 80.8 Participated in cervical examination No 14,664 19.5 48.7 18.7 47.5 Yes 22,689 80.5 51.3 81.3 52.5 Participated in examinations for common women’s diseases <0.001 <0.001 Never participated 8,650 10.7 29.1 10.4 28.2 Free inspection 5,469 10.7 16.5 10.4 16.4 Inspection at own expense 4,647 16.1 10.7 16.4 10.9 Self-paid & free 18,587 62.5 43.7 62.8 44.5 *Note: P-values are from Pearson chi-square tests.
Abbreviation: BMI=body mass index.Table 1. Characteristics of women with vaginitis aged 18–74 years in five provinces, China (N=37,353).
Figure 1 presents the multivariable logistic regression analysis results. Women aged 35–54 years demonstrated a moderately elevated risk of vaginal infections compared to those aged 18–34 years [odds ratio (OR)=1.183, 95% confidence interval (CI): 1.109, 1.262]. After covariate adjustment, women aged 55–74 showed reduced risk relative to the 18–34 age group (OR=0.851, 95% CI: 0.767, 0.944). Infection rates were significantly higher among women from Hubei and Yunnan provinces compared to Shandong Province. Married status was associated with increased infection risk (OR=1.17, 95% CI: 1.062, 1.29). A strong dose-response relationship emerged between pregnancy number and infection risk, with women reporting three or more pregnancies showing the highest risk (OR=4.835, 95% CI: 4.255, 5.495). Both smoking (OR=1.186, 95% CI: 1.036, 1.357) and alcohol consumption (OR=1.606, 95% CI: 1.52, 1.697) emerged as significant risk factors. Additionally, participants reporting poor physical and mental health status demonstrated substantially higher infection rates compared to those reporting good health.
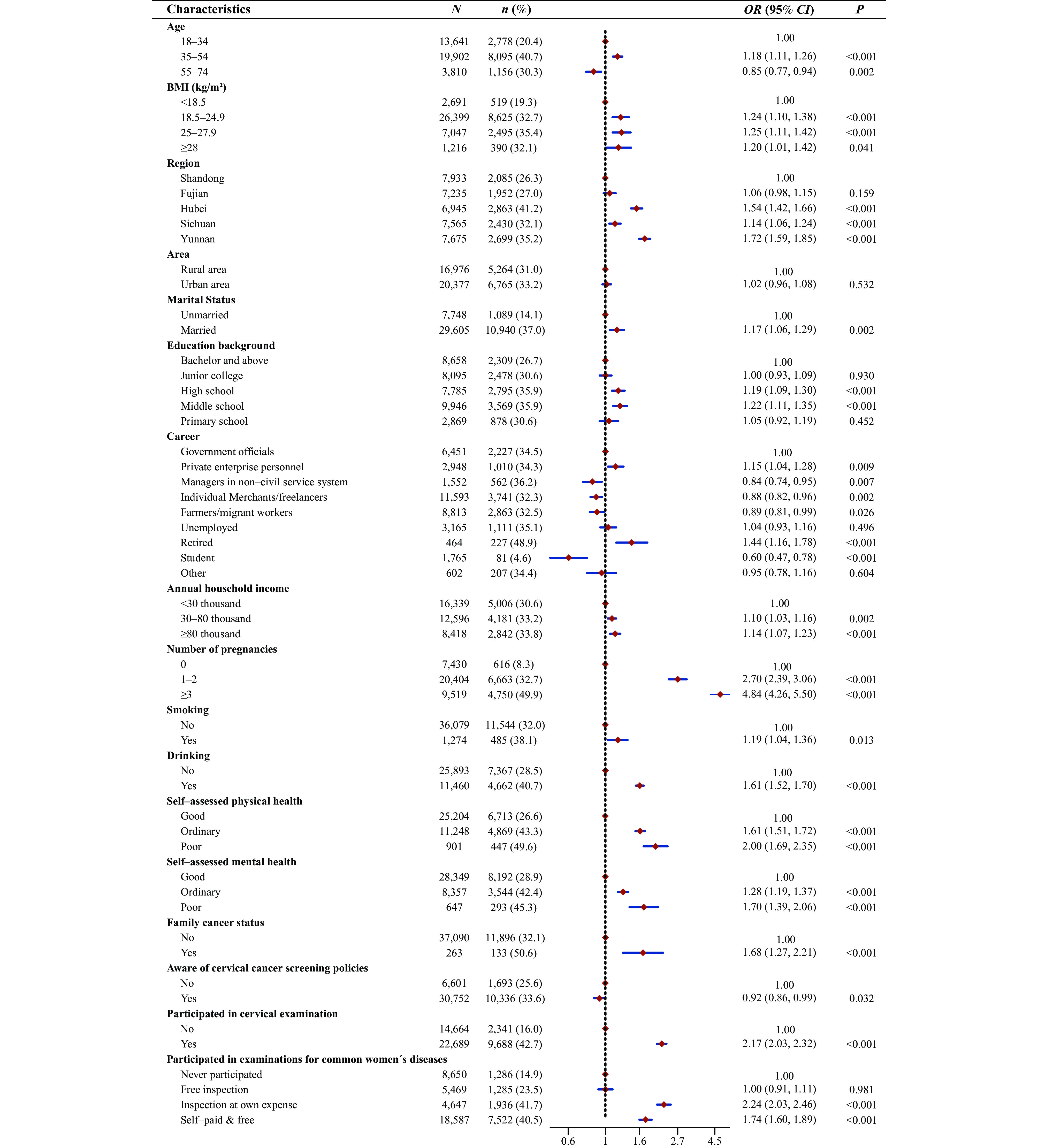 Figure 1.
Figure 1.Multivariable logistic regression analysis of vaginitis epidemiology among women aged 18–74 years across five provinces in China (N=37,353, n=12,029).
Abbreviation: OR=odds ratio; CI=confidence interval; BMI=body mass index.After controlling for confounding variables, awareness of cervical cancer screening policies emerged as a protective factor against vaginal infections (OR=0.922, 95% CI: 0.856, 0.993). Women with familial cervical cancer history showed increased infection susceptibility (OR=1.677, 95% CI: 1.274, 2.207). Notably, cervical screening participation was associated with significantly higher infection detection rates compared to non-participation (OR=2.170, 95% CI: 2.033, 2.315). Higher infection prevalence was observed among women who participated in gynecological disease screening, particularly those who accessed paid screening services or both paid and free screening programs. Even participants utilizing only free screening services showed elevated infection rates compared to non-participants. Sensitivity analysis (Figure 2) demonstrated consistent epidemiological patterns between diagnosed cases and treated patients, with risk factor associations remaining stable across both analytical models.
-
While existing vaginitis research predominantly focuses on clinical diagnostics and treatment (4), this study provides comprehensive epidemiological data on vaginitis among Chinese women, revealing a prevalence rate of 32.2%. Since the study included only clinically confirmed cases, undiagnosed infections may have been overlooked, potentially underestimating the true prevalence and suggesting an even greater disease burden. Evidence indicates a potential association between vaginitis and cervical cancer, characterized by shared risk factors and frequent co-occurrence (5-6). China’s cervical cancer screening program incorporates comprehensive gynecological examinations, including medical history assessment, external and vaginal examinations, pelvic examinations, and vaginal discharge analysis, effectively integrating vaginitis detection into routine health assessments. Our findings identify women aged 35–54 as a high-risk group for vaginitis, aligning with China’s cervical cancer screening program’s target age range of 35–64 years. While experts advocate for expanding screening to younger and older age groups to address broader health needs, current resource constraints necessitate focusing on high-risk populations, a strategy supported by our findings.
Women aged 18–34 represent a particularly vulnerable population for vaginitis, often experiencing stigma and hesitancy toward gynecological consultations, resulting in delayed care-seeking behavior (7). Limited reproductive health knowledge frequently leads to inappropriate hygiene practices, either insufficient or excessive, disrupting vaginal microbiota and increasing infection risk (8). Given the rising prevalence in this demographic, local governments should consider prioritizing screening programs to enhance awareness and promote preventive behaviors. Moreover, married women with multiple pregnancies, particularly those with three or more, require special attention due to the significant impact of maternal health on both individual well-being and future generations, emphasizing the necessity for targeted health education initiatives (9).
This study demonstrated that poor physical and mental health status significantly increased vaginitis risk, emphasizing the interconnected nature of systemic and reproductive health (10). Risk-associated behaviors, including smoking and alcohol consumption, were linked to higher infection rates (8). The presence of familial cervical cancer history suggested potential genetic or shared environmental influences on vaginal health susceptibility. Notable regional variations in prevalence, likely attributable to environmental factors and healthcare policy differences, underscore the necessity for geographically tailored gynecological healthcare interventions.
The findings indicate that cervical cancer screening policies may serve as an effective mechanism for enhancing women’s health literacy, contributing to improved awareness and detection of both vaginitis and other gynecological conditions. The higher incidence rates observed among women participating in gynecological screening programs highlight these initiatives’ crucial role in early detection and clinical management. These results emphasize that regular screening programs represent a fundamental strategy for both vaginitis prevention and comprehensive reproductive health improvement.
This study has several limitations. First, the absence of detailed classifications by vaginitis type and severity may limit the specificity of our findings. Second, the cross-sectional design precludes definitive causal inferences. Third, data collection constraints prevented recording the precise timing of infections, potentially introducing temporal bias. Longitudinal studies are needed to elucidate temporal relationships and establish causality.
This investigation advances the epidemiological understanding of vaginitis while demonstrating the significant role of cervical cancer screening policies in disease prevention and management. The integration of regular screenings, encompassing both cervical cancer and common gynecological examinations, is crucial for early detection of conditions like vaginitis. National health policies should maintain cervical cancer screening as a priority while expanding its scope to include surveillance and management of common gynecological conditions. To address regional healthcare disparities and improve women’s health outcomes, enhanced disease surveillance systems are essential. Furthermore, targeted health education initiatives should focus on high-risk reproductive-aged women and populations with lower educational or employment levels. These comprehensive strategies are fundamental to achieving equitable reproductive healthcare and improving overall women’s health outcomes.
-
The partner organizations: the All-China Women’s Federation and the Women’s Federations in Shandong, Sichuan, Hubei, Yunnan, and Fujian Provinces, along with grassroots Women’s Federation officials; and all study participants.
HTML
| Citation: |



 Download:
Download:





