-
China maintains a highly sophisticated HIV surveillance and reporting system that enables real-time monitoring of epidemic trends. In the early 2000s, the epidemic was characterized by three distinct phases: sporadic cases (1985–1988), localized spread (1989–1994), and localized with local generalized epidemic (1995–present) (1). Since then, the epidemic has undergone significant transformations, including a shift in the primary transmission route from blood to sexual transmission, persistently high annual diagnosis rates, and a notable increase in the proportion of elderly cases (2-3). By the end of 2023, China reported nearly 1.3 million people living with HIV, representing a significant portion of the estimated 39.9 million cases globally (4).
The formulation of evidence-based strategies to advance high-quality HIV prevention and control is crucial for addressing evolving epidemic patterns both domestically and internationally (5). This study analyzed national surveillance data from 1989 to 2023 to provide a comprehensive historical review and current assessment of HIV epidemiology in China. Through a detailed examination of epidemic phenomena and emerging prevention challenges, this research establishes a foundation for developing future policies and strategic interventions.
-
Data were extracted from the Comprehensive Response Information Management System (CRIMS) database of China, using the cumulative database as of June 2024 for cases reported between 1989 and 2023. CRIMS is a real-time online database that allows personal information updates during follow-up, which may result in discrepancies with previously published data. Although 22 cases were reported between 1985 and 1988, these were all foreigners or related to imported blood products (6). Therefore, this study's analysis begins in 1989, when the first indigenous case was reported.
Non-marital and non-commercial heterosexual contact (NMNCHC) refers to heterosexual behavior between individuals who are neither married nor in a regular relationship and where no monetary or material transaction occurs. This includes sexual encounters between temporary partners and casual heterosexual contacts (7). NMNCHC was incorporated into the online case report form as an HIV contact history category in August 2014 (8).
For this study, the general population is defined as individuals without HIV-positive spouses or immediate family members who have not engaged in high-risk behaviors such as injecting drug use, male same-sex behavior, or commercial sex work (either selling or buying). These individuals’ HIV exposure risk is exclusively through non-marital, non-commercial heterosexual contact.
The analysis employed descriptive statistics and stacked area charts to illustrate transmission patterns across different phases. Geographical correlations between transmission routes were examined using scatter plots and Pearson correlation coefficients. The extent and trends of HIV spread among the general population were assessed using Venn diagrams and the Cochran-Armitage test. All statistical tests were two-sided, with significance set at P<0.05. Analyses were conducted using Microsoft Excel (Microsoft Corp 2016, Redmond, Washington USA) and R (version 4.4.0, R Foundation for Statistical Computing, Vienna, Austria).
-
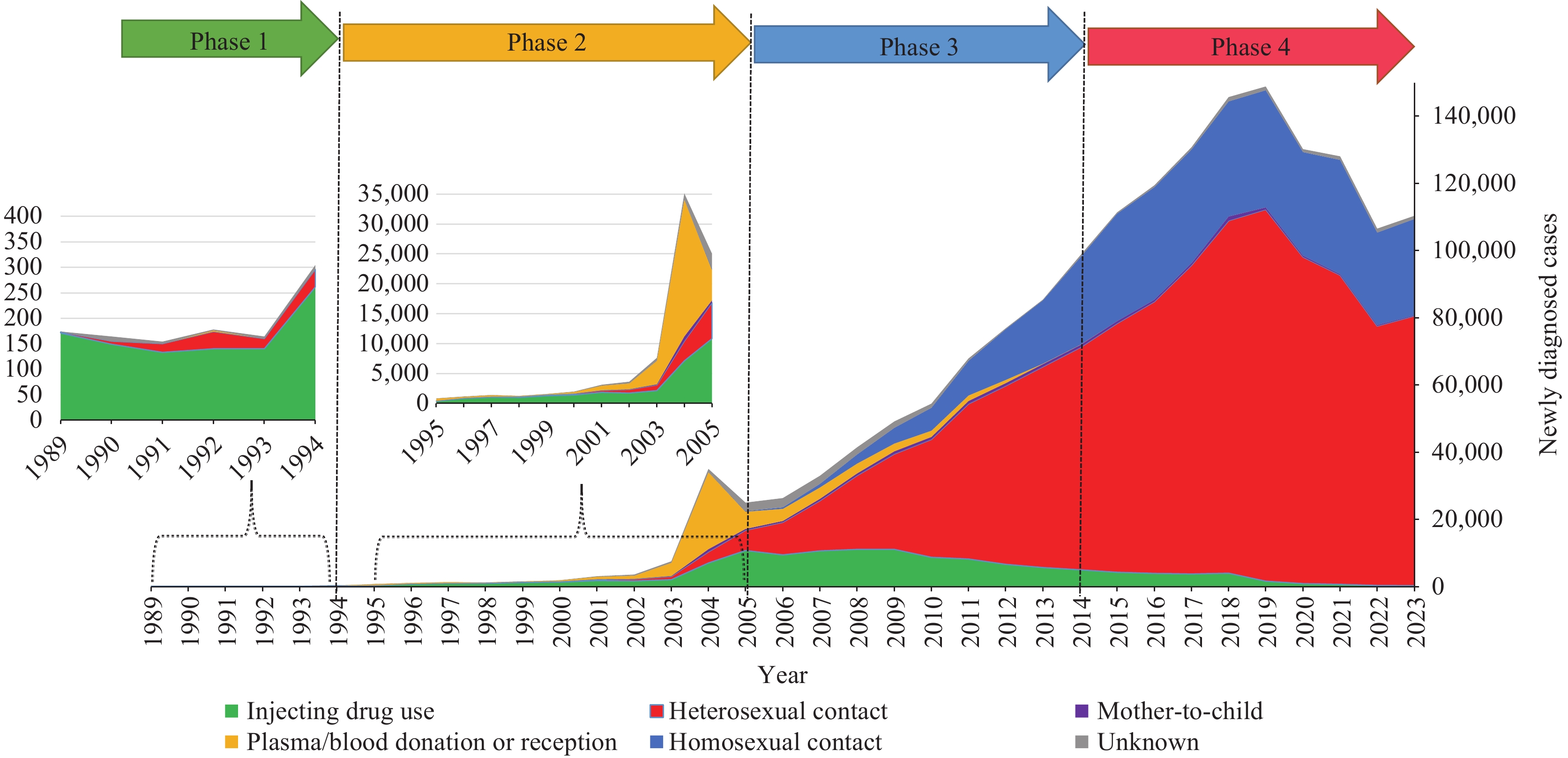
The HIV epidemic in China can be categorized into four distinct phases based on transmission patterns. Phase 1 (1989–1994) began with the first indigenous outbreak among injecting drug users (IDUs) in 1989, accompanied by sporadic cases of heterosexual transmission. During this initial phase, 1,138 infections were reported, with 87.3% attributed to drug injection and 10.0% to heterosexual contact.
Phase 2 (1995–2005) witnessed continued growth in both injection drug use and heterosexual transmission. Additionally, infections among former plasma donors (FPD) emerged and peaked at approximately 23,000 cases following the national HIV testing campaign in 2004. Of the 82,674 total infections reported during this phase, injection drug use accounted for 35.7%, heterosexual contact for 14.4%, and plasma/blood-product donation and reception for 42.3%.
Phase 3 (2006–2014) marked a significant shift as heterosexual contact surpassed injection drug use as the predominant transmission route. This period also saw a rapid increase in homosexual transmission, while infections from plasma/blood-product donation and reception declined until elimination. Among the 533,374 reported infections during this phase, injection drug use represented 14.4%, heterosexual contact 62.8%, and homosexual contact 16.1%.
Phase 4 (2015–present) is characterized by the sustained dominance of heterosexual transmission, leading to substantial spread within the general population — a phenomenon analyzed in detail in the third section. Of the 1,131,464 infections reported during this phase, heterosexual and homosexual contact accounted for 72.0% and 25.2%, respectively (Figure 1).
-
Analysis of transmission route patterns across different epidemic phases revealed that HIV spread in China was primarily driven by injecting drug use, plasma/blood donation and reception, and sexual contact (both heterosexual and homosexual). Previous research has demonstrated that multiple high-risk behaviors among infected individuals facilitated HIV transmission across different population groups (8).
Our geographical analysis of these four transmission routes revealed their presence across all 31 provincial-level administrative divisions (PLADs) in China. A strong positive linear correlation (r=0.88, P<0.001) emerged between the cumulative number of injection drug users and heterosexually transmitted cases at the provincial level. However, no significant correlations were observed among other transmission routes (Figure 2).
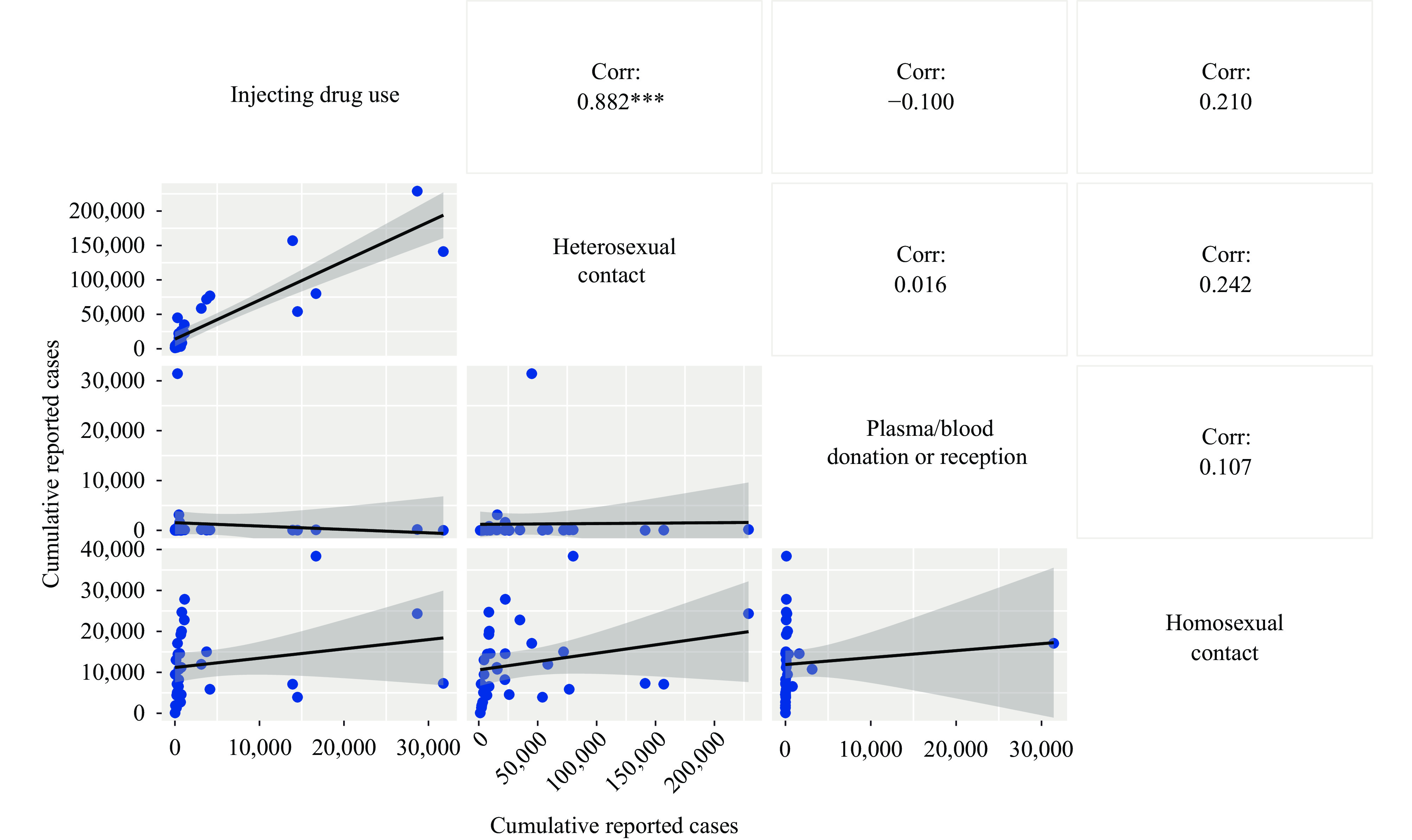 Figure 2.
Figure 2.Scatter plot and correlation coefficient matrix diagram of the cumulative numbers of individuals infected with HIV through four transmission routes in 31 PLADs, by 2023.
Note: Asterisk indicates statistical significance.
Abbreviation: Corr=correlation coefficient; PLADs=provincial-level administrative divisions.
-
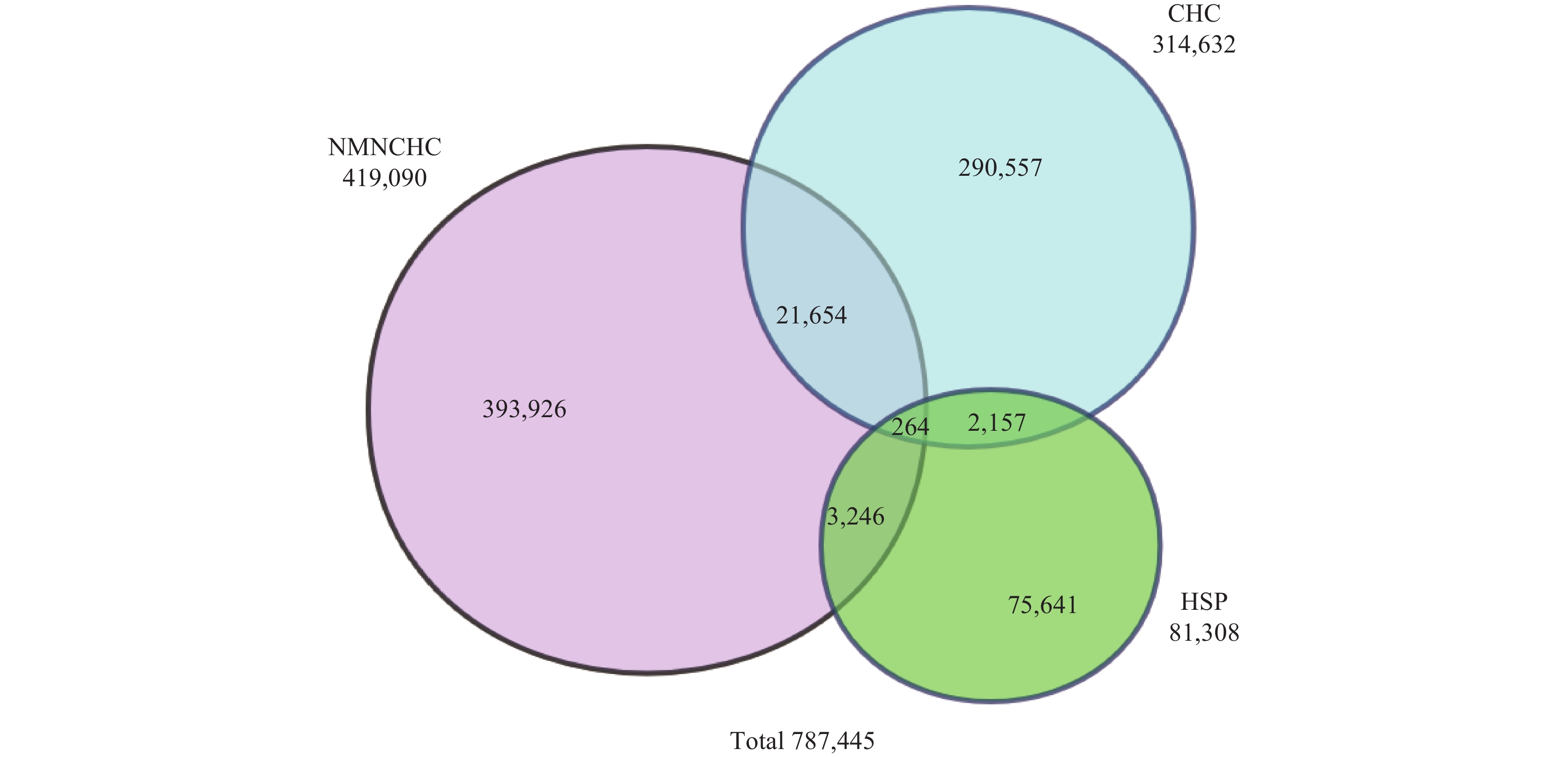
HIV exposure through heterosexual contact can occur through three distinct pathways: NMNCHC, commercial heterosexual contact (CHC), and contact with an HIV-positive spouse/regular partner (HSP).
Between 2015 and 2023, 787,445 individuals (97.3%) out of 808,978 cases of heterosexual HIV transmission provided detailed contact histories. Among these cases, 393,926 (50.0%) were from the general population with NMNCHC as their sole risk factor, 290,557 (36.9%) reported only CHC, 75,641 (9.6%) had an HSP without other non-marital heterosexual contact, and 27,321 (3.5%) reported multiple contact histories. These distributions are detailed in Table 1 and Figure 3. The proportion of general population cases among heterosexual transmissions showed a significant upward trend, increasing from 46.2% to 55.7% (Z=42.7, P<0.001), while all other contact history categories exhibited declining trends, as shown in Table 1.
Year Total cases NMNCHC CHC HSP Multiple
contact histories2015 72,686 33,577 (46.2) 28,259 (38.9) 8,200 (11.3) 2,650 (3.6) 2016 79,198 37,585 (47.5) 30,469 (38.5) 8,509 (10.7) 2,635 (3.3) 2017 89,593 43,609 (48.7) 33,628 (37.5) 9,055 (10.1) 3,301 (3.7) 2018 102,145 51,032 (50.0) 37,096 (36.3) 10,168 (10.0) 3,849 (3.8) 2019 107,520 52,684 (49.0) 40,371 (37.5) 10,339 (9.6) 4,126 (3.8) 2020 95,368 46,766 (49.0) 36,290 (38.1) 8,973 (9.4) 3,339 (3.5) 2021 89,218 45,925 (51.5) 32,684 (36.6) 7,781 (8.7) 2,828 (3.2) 2022 74,318 39,649 (53.4) 26,044 (35.0) 6,335 (8.5) 2,290 (3.1) 2023 77,399 43,099 (55.7) 25,716 (33.2) 6,281 (8.1) 2,303 (3.0) Z 42.737 −23.83 −27.598 −9.4913 P <0.001 <0.001 <0.001 <0.001 Abbreviation: NMNCHC=non-marital and non-commercial heterosexual contact; CHC=commercial heterosexual contact; HSP=HIV-positive spouse/regular partner. Table 1. Contact histories of individuals with heterosexual HIV transmission in China by year, 2015 –2023.
-
Based on our analysis, the HIV epidemic in China evolved through four distinct phases, each characterized by a predominant transmission mode. While detection rates and delayed diagnosis patterns varied across populations, previous research has confirmed that these variations do not invalidate our phase classification (2). At the provincial level, we observed a strong correlation (r=0.88, P<0.001) between the geographical distribution of injection drug use (prevalent in the initial phase) and heterosexual transmission (dominant in the final two phases). This correlation likely stems from HIV-infected injecting drug users being the primary source of transmission to heterosexual populations (8), resulting in their profound influence on subsequent heterosexual transmission patterns. This suggests that regions with earlier epidemic emergence may experience higher rates of heterosexual transmission.
The elimination of transmission through plasma/blood donation and reception, along with the successful containment of drug injection and mother-to-child transmission, demonstrates the effectiveness of targeted interventions for well-defined populations. Traditional control strategies, such as the Blood Donation Law of 1998 and the needle exchange program initiated in 2000, effectively blocked blood-related transmission routes. The 2004 implementation of active testing campaigns targeting high-risk populations, particularly former plasma donors (9), successfully identified transmission sources while accounting for the marked increase in case numbers within these populations.
Sexual transmission presents unique challenges due to the large, widely distributed populations involved, making traditional identification approaches less effective. Previous research estimates that men who engage in homosexual behavior comprise approximately 1.7% of adult males (10), while female sex workers represent 0.19% to 0.75% of women in corresponding age groups, with male clients numbering 2.4 to 5.8 times higher (11-12). The general population engaging in non-marital and non-commercial heterosexual contact represents the largest demographic, facilitating ongoing HIV transmission from high-risk populations to the general population.
Our findings reveal significant HIV spread within the general population, with nearly 0.4 million general individuals diagnosed with HIV infection over the past 9 years, representing more than 50% of all heterosexual transmissions since 2019. This substantial infection rate through casual sexual encounters and temporary relationships reflects both evolving social norms (13) and improved testing accessibility. Most heterosexual transmission cases are identified through medical institutions during non-AIDS-related care, primarily due to challenges in targeted detection and low testing awareness. While expanded provider-initiated HIV testing has increased case identification, this approach often fails to detect infections promptly (14), potentially allowing secondary transmission before effective intervention.
The general population’s heterogeneity across age, gender, occupation, and education levels poses significant challenges for developing unified health education strategies, particularly compared to more concentrated high-risk populations. Furthermore, since non-marital and non-commercial heterosexual contact typically occurs in contexts of trust or sexual impulse, a significant disconnect exists between knowledge and behavior (15).
This study has two primary limitations. First, the general population estimates may be inflated due to the relatively low sensitivity of non-marital and non-commercial heterosexual contact history reporting. Second, transmission route misclassification may occur due to reliance on self-reported contact histories, particularly regarding homosexual transmission potentially being misclassified as heterosexual transmission.
In conclusion, HIV has significantly penetrated the general population through heterosexual contact, necessitating the development of distinct, tailored prevention strategies for both high-risk and general populations to address these emerging challenges.
-
The contributions of staff members at provincial, prefectural, and county-level CDC.
HTML
Transmission Modes in Different Phases
Correlations in the Geographical Distribution of Different Transmission Routes
The Spread of HIV to the General Population
| Citation: |



 Download:
Download: