-
Kidney diseases encompass a variety of progressive disorders that disrupt the structure and function of the kidneys because of diverse etiologies. Notable among these are kidney cancer, glomerular disease, tubulointerstitial nephritis, and kidney failure (1). These diseases significantly affect global health; notably, chronic kidney disease caused approximately 1.2 million deaths globally in 2017, reflecting a 41.5% increase in the global chronic kidney disease mortality rate from 1990 to 2017 (2). According to the 2019 GBD study, the mortality rate from kidney cancer in China was 2.79 per 100,000 persons in 2019, and the mortality rates of both kidney cancer and chronic kidney disease have been rising since 1990 (3). The aging population has further exacerbated the burden, making kidney diseases a progressively common cause of death. Remarkably, nearly one-fifth of all global chronic kidney disease patients are in China (4). Despite the significance of this issue, few studies have examined mortality due to major kidney diseases at a national level. Therefore, this study utilizes data from the National Cause of Death Surveillance System to assess the mortality trends associated with major kidney diseases among Chinese residents from 2014 to 2021, aiming to inform targeted prevention and control strategies.
-
This study sourced its data from 605 surveillance sites within the National Death Cause Surveillance System, covering the period from 2014 to 2021. Surveillance sites reporting an all-cause mortality rate below 5‰ were systematically excluded annually. Major kidney diseases were classified according to the International Classification of Disease 10th Revision (ICD-10) and included kidney cancer (C64–C65), glomerular disease (N00–N08), tubulointerstitial nephritis (N10–N16), and kidney failure (N17–N19). Standard population demographics were derived from the Yearbook of the Seventh National Census of 2020 published by the National Bureau of Statistics.
The study examined various mortality indicators concerning major kidney diseases from 2014 to 2021. These included the crude mortality rate, age-specific mortality rate, and age-standardized mortality rates (ASMRs) for kidney cancer, glomerular disease, tubulointerstitial nephritis, and kidney failure across different demographics (males and females), as well as urban versus rural settings and regional distinctions (Eastern, Central, and Western). These regions were further divided into 31 provincial-level administrative divisions (PLADs): 11 in the Eastern region (Beijing, Tianjin, Hebei, Liaoning, Shanghai, Jiangsu, Zhejiang, Fujian, Shandong, Guangdong, Hainan), 8 in the Central region (Shanxi, Jilin, Heilongjiang, Anhui, Jiangxi, Henan, Hubei, Hunan), and 12 in the Western region (Inner Mongolia, Guangxi, Chongqing, Sichuan, Guizhou, Yunnan, Xizang, Shaanxi, Gansu, Qinghai, Ningxia, Xinjiang). For analysis, SAS (version 9.4; SAS Institute Inc., Cary, USA) calculated the crude and ASMRs, excluding data from surveillance sites with an all-cause mortality rate below 5‰. Additionally, Joinpoint software (version 5.0.2, Applications Branch, National Cancer Institute, Bethesda, USA) was used to assess trends in ASMRs of major kidney diseases and to compute the average annual percent change (AAPC) with 95% confidence intervals (CI).
Personnel at each surveillance site undergo an annual training course on cause-of-death surveillance, which is organized by the China CDC. They must pass an examination to be registered. Additionally, the examination of cause-of-death registration and reporting is conducted regularly. Regular investigations into underreporting are also performed on a sample of reporting units to ensure data quality.
-
The crude mortality rates for major kidney diseases demonstrated an increasing trend in both males and females, with AAPCs of 1.8% (95% CI: 0.8%, 2.9%) in males and 0.7% (95% CI: 0%, 1.4%) in females, and these changes were statistically significant (P<0.05). Conversely, the ASMR for females declined from 6.9 per 100,000 to 5.7 per 100,000, with an AAPC of −3.0% (95% CI: −4.5%, −1.5%). However, this downward trend was not statistically significant in males (P>0.05).
The crude mortality rates for kidney cancer have risen in both males and females, with AAPCs of 4.9% (95% CI: 4.0%, 5.9%) and 5.1% (95% CI: 3.8%, 6.3%), respectively. In contrast, the ASMR for kidney cancer increased slightly in both genders, with AAPCs of 1.1% (95% CI: −0.5%, 2.8%) for males and 1.0% (95% CI: −0.6%, 2.6%) for females, though these changes were not statistically significant (both P>0.05). Significant declines in ASMR were noted for glomerular disease and kidney failure in females, with AAPCs of −2.9% (95% CI: −4.8%, −1.0%) and −3.6% (95% CI: −5.3%, −1.8%), respectively. Males displayed a significant reduction in the ASMR for tubulointerstitial nephritis, with an AAPC of −4.7% (95% CI: −7.0%, −2.5%) (Table 1).
Year Male Female Kidney cancer Glomerular disease Tubulointerstitial nephritis Kidney failure Total Kidney cancer Glomerular disease Tubulointerstitial nephritis Kidney failure Total CMR ASMR CMR ASMR CMR ASMR CMR ASMR CMR ASMR CMR ASMR CMR ASMR CMR ASMR CMR ASMR CMR ASMR 2014 1.1 1.4 4.4 5.5 0.4 0.6 2.4 3.0 8.2 10.4 0.6 0.7 3.5 3.8 0.3 0.4 1.8 2.0 6.2 6.9 2015 1.2 1.5 4.7 6.0 0.4 0.5 2.3 2.9 8.6 10.8 0.7 0.8 3.6 4.0 0.3 0.4 1.7 1.9 6.3 7.0 2016 1.3 1.5 5.0 6.0 0.4 0.5 2.2 2.6 8.8 10.6 0.7 0.8 3.7 3.9 0.4 0.4 1.6 1.7 6.4 6.8 2017 1.3 1.6 5.3 6.3 0.4 0.5 2.2 2.7 9.1 11.0 0.7 0.8 3.8 4.1 0.3 0.3 1.6 1.7 6.4 6.8 2018 1.4 1.6 5.1 5.9 0.4 0.5 2.3 2.7 9.1 10.6 0.8 0.8 3.8 3.9 0.3 0.3 1.7 1.7 6.5 6.7 2019 1.5 1.7 5.0 5.7 0.4 0.4 2.2 2.5 9.0 10.3 0.8 0.8 3.7 3.7 0.3 0.3 1.6 1.6 6.5 6.5 2020 1.5 1.6 4.8 5.3 0.4 0.4 2.3 2.5 9.0 9.8 0.8 0.8 3.6 3.3 0.3 0.3 1.6 1.5 6.3 5.9 2021 1.6 1.6 5.3 5.3 0.4 0.4 2.6 2.6 9.8 9.8 0.9 0.8 3.7 3.1 0.3 0.2 1.9 1.6 6.7 5.7 AAPC
(%)4.9 1.1 2.1 −1.1 −1.6 −4.7 1.6 −2.2 1.8 −1.1 5.1 1.0 0.6 −2.9 −2.4 −7.6 0.0 −3.6 0.7 −3.0 95% CI lower 4.0 −0.5 −1.7 −3.2 −3.4 −7.0 −1.5 −5.1 0.8 −2.7 3.8 −0.6 −0.6 −4.8 −6.9 −15.4 −2.5 −5.3 0.0 −4.5 95% CI upper 5.9 2.8 6.1 1.1 0.3 −2.5 4.9 0.8 2.9 0.5 6.3 2.6 1.8 −1.0 2.3 0.9 2.6 −1.8 1.4 −1.5 P 0.001 0.175 0.286 0.341 0.078 0.002 0.318 0.141 0.005 0.191 0.001 0.168 0.332 0.003 0.310 0.078 0.967 0.003 0.049 0.001 Abbreviation: CMR=crude mortality rate; ASMR=age-standardized mortality rate; AAPC=average annual percent change; CI=confidence intervals. Table 1. Mortality rate and age-standardized mortality rate (per 100,000) for major kidney diseases in China, 2014–2021.
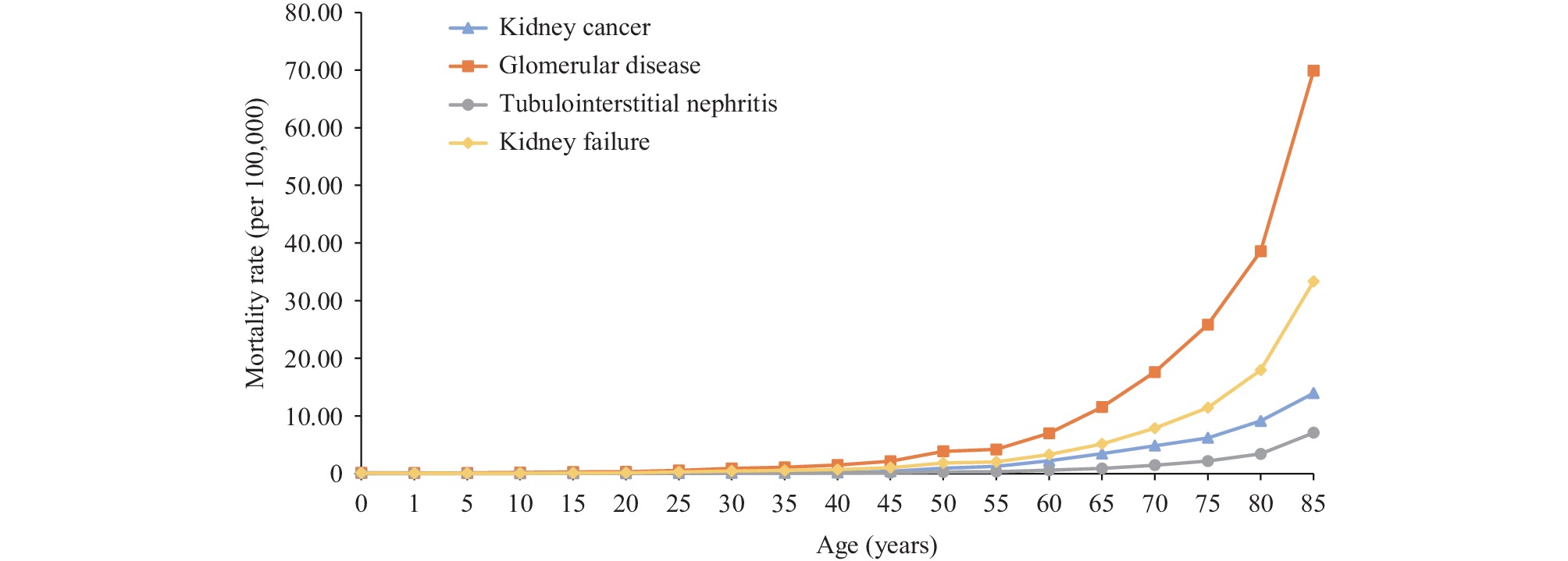
The age-specific mortality rates for the four principal kidney diseases demonstrated consistent trends, with low rates observed under the age of 35, a gradual rise between ages 35 and 60, a sharp increase after age 60, and peaking in the 85 and older age group. Among these conditions, glomerular diseases had the highest crude mortality rate, followed by kidney failure, kidney cancer, and tubulointerstitial nephritis (Figure 1).
The ASMR for all types of kidney disease demonstrated a decreasing trend in urban areas, with statistically significant reductions (P<0.05). The most notable decrease was observed in tubulointerstitial nephritis, which exhibited an AAPC of −7.3% (95% CI: −10.7%, −3.9%). Conversely, in rural areas, only the ASMR for tubulointerstitial nephritis followed a similar declining trend, with an AAPC of −4.9% (95% CI: −7.3%, −2.3%). The ASMRs for other kidney disease types remained stable (Table 2).
Year Urban Rural Kidney cancer Glomerular disease Tubulointerstitial nephritis Kidney failure Total Kidney cancer Glomerular disease Tubulointerstitial nephritis Kidney failure Total 2014 1.7 4.1 0.4 2.8 9.0 0.7 4.8 0.5 2.3 8.3 2015 1.7 4.4 0.4 2.5 9.0 0.9 5.2 0.4 2.3 8.7 2016 1.7 4.4 0.4 2.5 8.9 0.9 5.2 0.5 2.0 8.5 2017 1.7 4.4 0.4 2.6 9.1 0.9 5.5 0.4 1.9 8.7 2018 1.6 4.3 0.4 2.5 8.7 0.9 5.1 0.4 2.0 8.4 2019 1.6 4.0 0.3 2.3 8.2 1.0 5.0 0.4 1.9 8.3 2020 1.4 3.5 0.3 2.1 7.3 1.0 4.7 0.4 1.9 7.9 2021 1.4 3.3 0.2 2.1 7.1 1.0 4.5 0.3 2.1 7.9 AAPC (%) −2.7 −3.7 −7.3 −3.6 −3.7 4.1 −1.3 −4.9 −2.4 −1.1 95% CI (−5.1, −0.3) (−5.9, −1.4) (−10.7, −3.9) (−5.5, −1.7) (−5.4, −2.0) (−1.0, 9.4) (−2.9, 0.4) (−7.3, −2.3) (−6.0, 1.5) (−2.8, 0.6) P 0.028 0.002 0.002 0.004 <0.001 0.119 0.132 0.004 0.222 0.214 Abbreviation: AAPC=average annual percent change; CI=confidence intervals. Table 2. Differences in age−standardized mortality rates (per 100,000) for major kidney diseases between urban and rural areas in China, 2014–2021.
The highest ASMR for kidney cancer was found in the eastern region, surpassing rates in both the central and western regions. Notably, the central region experienced the most significant increase in ASMR for kidney cancer, with an AAPC of 2.1% (95% CI: 0.5%, 3.7%). In contrast, ASMRs for other kidney-related diseases have generally decreased across different regions. The eastern region recorded the steepest declines in ASMR for tubulointerstitial nephritis and glomerular disease, with AAPCs of −7.9% (95% CI: −9.5%, −6.3%) and −4.6% (95% CI: −8.0%, −1.0%), respectively. The central region saw significant reductions in ASMR for tubulointerstitial nephritis and kidney failure, with AAPCs of −8.9% (95% CI: −14.9%, −2.5%) and −2.8% (95% CI: −5.1%, −0.6%). Additionally, the western region exhibited the most rapid decrease in ASMR for kidney failure, with an AAPC of −2.3% (95% CI: −4.3%, −0.2%) (Table 3).
Year Eastern region Central region Western region Kidney cancer Glomerular disease Tubulointerstitial nephritis Kidney failure Total Kidney cancer Glomerular disease Tubulointerstitial nephritis Kidney failure Total Kidney cancer Glomerular disease Tubulointerstitial nephritis Kidney failure Total 2014 1.3 3.5 0.3 2.3 7.5 0.9 5.5 0.5 2.1 8.9 0.6 5.5 0.6 3.2 10.0 2015 1.5 3.4 0.3 2.3 7.5 1.0 5.9 0.5 1.8 9.2 0.8 6.2 0.6 3.0 10.5 2016 1.5 3.6 0.3 2.0 7.4 1.0 5.5 0.5 1.8 8.8 0.8 6.3 0.6 2.8 10.4 2017 1.5 3.6 0.3 2.2 7.5 1.0 6.0 0.5 1.8 9.2 0.8 6.7 0.5 2.7 10.7 2018 1.5 3.3 0.2 2.2 7.2 1.0 5.6 0.4 1.8 8.8 0.8 6.6 0.6 2.7 10.7 2019 1.5 3.1 0.2 2.2 7.0 1.1 5.7 0.4 1.6 8.8 0.8 6.0 0.6 2.6 9.9 2020 1.5 2.6 0.2 1.8 6.0 1.1 5.4 0.3 1.6 8.4 0.7 5.6 0.6 2.7 9.6 2021 1.5 2.6 0.2 2.0 6.2 1.0 5.2 0.3 1.7 8.2 0.7 5.4 0.5 2.8 9.4 AAPC (%) 1.2 −4.6 −7.9 −2.8 −3.0 2.1 −0.8 −8.9 −2.8 −1.2 0.7 −0.7 −1.4 −2.3 −1.1 95% CI lower −0.6 −8.0 −9.5 −5.1 −5.9 0.5 −4.0 −14.9 −5.1 −2.8 −4.7 −2.9 −4.0 −4.3 −2.6 95% CI upper 3.0 −1.0 −6.3 −0.5 0.1 3.7 2.5 −2.5 −0.6 0.5 6.3 1.6 1.3 −0.2 0.5 P 0.193 0.013 <0.001 0.025 0.054 0.018 0.635 0.007 0.023 0.154 0.810 0.550 0.254 0.035 0.174 Abbreviation: AAPC=average annual percent change; CI=confidence intervals. Table 3. Differences among regions in age−standardized mortality rate (per 100,000) for major kidney diseases in China, 2014–2021.
-
This study investigated the trends in mortality rates for major kidney diseases in China from 2014 to 2021. Overall, the ASMR was higher in males than females and higher in urban areas than in rural areas. Except for kidney cancer, the ASMR was higher in western regions than in the central and eastern regions. The crude mortality rate of all types of major kidney diseases gradually increased with age. In addition to an increase in the ASMR of kidney cancer in the central region, that of major kidney diseases decreased in most areas and populations.
The crude mortality rates for both male and female patients with kidney cancer and major kidney diseases have shown an upward trend. However, there is no significant increase in the ASMR for kidney cancer in either gender, likely reflective of the gradual aging of the population. This study highlights that, excluding kidney cancer, the ASMR for glomerular disease, tubulointerstitial nephritis, and kidney failure generally displays a decreasing trend across most regions and populations. Particularly in economically prosperous areas, notably urban and eastern regions, this decline can be attributed to advances in medical technology, enhancements in healthcare services, and greater access to health education. These factors contribute to more timely and effective diagnosis and treatment of kidney diseases, thereby improving the prognosis for those diagnosed.
A study encompassing 195 countries reported that higher Socio-demographic Index (SDI) levels correlate with an increased incidence of kidney cancer burden. Notably, the ASMR for this cancer is higher in affluent areas, including Latin America and Eastern Europe, with significant rises observed in Eastern and Southern Asia (5). Further studies in the Middle East and North Africa have confirmed these findings, establishing a positive correlation between SDI and kidney cancer ASMR (6). These results partially explain the observed disparities in kidney cancer ASMR worldwide. In China, data shows an upward trend in kidney cancer ASMR within the central region from 2014 to 2021. Studies using Global Burden of Disease 2019 data have shown that this pattern is similar evident in Japan, The Republic of Korea, Singapore, and other countries (7). Many studies have linked risk factors such as smoking, obesity, hypertension, and elevated fasting blood glucose levels to higher rates of deaths associated with kidney cancer (8–9). With socioeconomic growth and improved living standards in China, the prevalence of these risk factors has risen annually, potentially contributing to the continual increase in kidney cancer ASMR (10). In alignment with the Healthy China 2030 initiative, it is crucial to strengthen tobacco control, raise awareness about the risks of tobacco use, and promote physical activity to effectively mitigate kidney cancer risk factors and reduce its burden.
The ASMR for non-cancerous kidney diseases was observed to be higher in rural and western areas. Chronic conditions such as cardiovascular disease, diabetes, and hypertension, along with prolonged use of anti-inflammatory medications, are identified as risk factors for mortality due to chronic kidney disease (11). Regular physical examinations to detect and manage these risk factors could markedly improve outcomes for these vulnerable populations. Additionally, the availability of medical care influences kidney disease mortality rates (12). Since a significant portion of individuals in underdeveloped areas often seek medical treatment across different regions (13), it is crucial to enhance primary healthcare services, optimize the allocation of resources related to kidney disease, and ensure better access to medical services for residents in rural and western regions.
This study was subject to some limitations. First, the data were sourced from the national cause-of-death surveillance system, which may suffer from underreporting, consequently leading to a possible underestimation of kidney disease mortality rates. To mitigate the impact of this underreporting and improve data reliability, this study excluded data from regions where the all-cause mortality rate was under 5‰ during the data compilation process. Additionally, there is an inherent delay in death surveillance data, with the most current data available only up to 2021. Despite these limitations, the data presented can still lay the groundwork for developing preventive strategies for kidney diseases. Future research should incorporate data from various sources to more accurately analyze the mortality rates and causes of death due to kidney diseases.
In conclusion, the trends identified in this study suggest that future preventive strategies should be region- and population-specific. Enhanced focus is essential on the health of elderly populations, as well as on improving health education for males, rural communities, and western regions. Furthermore, there is a need for strengthened tobacco control, efficient allocation of health resources, and measures to decrease the societal burden of kidney diseases.
HTML
| Citation: |



 Download:
Download:




