-
Depression is a pressing global health concern affecting populations worldwide. By 2015, the number of individuals affected globally reached 320 million, with a prevalence rate of 4.4% (1). Recent research in China (2) reported an 8.29% prevalence of moderate to severe depression in 2021, indicating a significant burden. While studies worldwide have linked depression to increased mortality rates (3–4), limited evidence exists specifically for China. This study utilized a population-based cohort in China to assess the 12-year mortality risk for individuals with depression in 2010. The findings revealed a notable positive correlation between depression and all-cause and cause-specific mortality among the Chinese population, indicating diverse effects across various demographics such as gender, age, and education level. Our results emphasize the necessity for enhanced physical and psychological support for all individuals with depression, with particular attention to males, urban residents, younger individuals (below 60 years), and those with higher education levels.
The China Chronic Disease and Risk Factor Surveillance (CCDRFS) is an enduring national survey overseen by the National Centre for Chronic and Non-communicable Disease Control and Prevention. The CCDRFS 2010 survey was conducted in 162 disease surveillance points (DSP) across China. It included over 100,000 participants aged 18 years and above. This study was ethically reviewed and approved by the institutional review board of China CDC under approval number 201010, with written consent obtained from all participants.
Individual data was collected from the CCDRFS 2010 and was cross-referenced with the National Mortality Surveillance System (NMSS) records until 2022 using unique ID numbers, establishing a 12-year cohort. The recorded death data contained the date of death and causes classified according to the ICD-10 system. Causes of death were grouped into categories including cardiovascular diseases (I21-I25, I60-I69), cancers (C00-C97), suicide (X60-X84), non-suicide injuries (V01-X59, X85-Y89), and other causes.
In the CCDRFS 2010 study, depression was evaluated using the Patient Health Questionnaire-9 (PHQ-9), comprising 9 questions on depression symptoms experienced in the previous two weeks, scoring from 0 (not at all) to 3 (nearly every day). Individuals with over 4 missing responses in the 9 questions were excluded, and multiple imputation was used to manage these missing values. Depression severity was classified into three levels: none (PHQ-9≤5), mild to moderate (5<PHQ-9≤15), and severe (PHQ-9>15). Additionally, various covariates such as demographic, behavioral, metabolic factors, and medical history were considered.
To ensure comparability, we standardized the proportion of baseline characteristics based on the age distribution of the total studied population, as the age distribution varied among individuals with different levels of depression. We utilized the cumulative incidence function (CIF) and performed a log-rank test. Hazard ratios (HRs) and 95% confidence intervals (CI) were calculated through three Cox models adjusting for various covariates. Subgroup analyses were carried out using Cox models in different subgroups. HRs for cause-specific mortality were determined using a competitive risk model. Statistical analyses were conducted using SAS (version 9.4; SAS Institute Inc., Cary, USA) and R (version 4.1.2; the R Core Team, R Foundation for Statistical Computing, Vienna, Austria).
Out of the total 98,658 participants, 288 were excluded due to having more than 4 missing values in the PHQ-9. Among the remaining 98,370 individuals, 5,683 (5.78%) had mild to moderate depression, while 341 (0.35%) had severe depression. The baseline characteristics can be found in Table 1.
Characteristics PHQ-9 score Men Women 0–5 years 6–15 years >15 years 0–5 years 6–15 years >15 years Number (n, %) 42,895 (95.35) 1,984 (4.41) 108 (0.24) 49,451 (92.63) 3,699 (6.93) 233 (0.44) Age (mean, s) 46.40 (15.24) 47.38 (16.24) 50.15 (15.49) 46.38 (14.63) 48.94 (15.16) 52.70 (15.16) Urban (%) 43.85 47.67 53.46 46.73 47.00 52.63 Education level (%) Less than primary 16.81 18.83 23.75 31.68 35.19 33.38 Primary 20.62 22.13 21.68 20.35 18.52 22.66 Junior secondary 36.60 29.30 26.11 27.92 24.42 20.17 Senior secondary 17.80 17.93 20.85 14.02 14.94 18.17 University and above 8.17 11.81 7.61 6.02 6.93 5.62 Marital status (%) Unmarried 5.90 8.72 15.93 3.17 4.86 6.23 Married 88.59 81.29 71.11 88.28 83.14 79.82 Divorced 1.68 4.41 8.55 1.41 2.31 4.79 Widowed 3.56 5.43 4.40 6.94 9.50 9.17 Other 0.27 0.16 <0.01 0.20 0.19 <0.01 Smoking (%) Current smoking, everyday 50.48 50.08 61.14 2.65 3.85 6.55 Current smoking, not everyday 5.29 6.62 1.24 0.53 1.00 0.93 Past smoking 11.20 15.75 14.93 0.77 1.52 1.85 Never smoking 33.02 27.55 22.69 96.05 93.63 90.67 Alcohol consumption (%) Frequent drinking 27.58 25.13 24.73 2.93 3.06 2.60 Light drinking 31.24 35.09 30.26 12.54 18.19 17.99 No drinking 41.18 39.78 45.01 84.53 78.75 79.41 Diet (%) Excessive intake of red meat 30.78 27.00 32.34 20.97 17.24 19.57 Insufficient intake of vegetable 42.90 41.64 40.90 43.13 43.15 43.54 Insufficient intake of fruit 90.19 89.54 88.05 86.11 85.67 87.64 Physical activity (%) Low 28.42 33.31 37.83 26.52 24.97 32.39 Medium 37.76 34.05 32.70 46.53 43.28 37.58 High 33.82 32.64 29.47 26.95 31.76 30.03 Insufficient sleep 17.20 28.79 46.83 17.02 31.33 39.55 BMI (%) Low weight 3.08 4.26 5.92 3.16 3.94 6.89 Normal 49.90 51.05 59.38 48.10 49.64 50.38 Overweight 34.23 31.21 26.88 33.97 31.62 27.81 Obesity 12.78 13.48 7.82 14.77 14.80 14.92 Note: All characteristics were age-standardized except number of participants and age.
Abbreviation: PHQ=patient health questionnaire; BMI=body mass index.Table 1. Baseline characteristics of participants with and without depression, by sex.
After a mean follow-up of 11.60 years, the study identified 7,333 deaths. Participants with depression had a higher cumulative mortality compared to those without (Figure 1). Table 2 presents overall and subgroup results for all-cause mortality. After adjusting for covariates, individuals with mild to moderate depression (HR=1.12, 95% CI: 1.03, 1.23) and severe depression (HR=1.88, 95% CI: 1.46, 2.43) showed increased risks. Among those with severe depression, males (2.60 vs. 1.49), urban dwellers (2.34 vs. 1.56), younger individuals (<60 years, 2.02 vs. 1.79), highly educated individuals (2.98 vs. 1.57), and those with low weight (2.16 vs. 1.62) had higher HRs. Mild to moderate depression also significantly affected most subgroups. Additionally, age-standardized mortality among men with severe depression was three times higher than that among women (25.98 vs. 8.66 per 1,000 person-years) (Table 2).
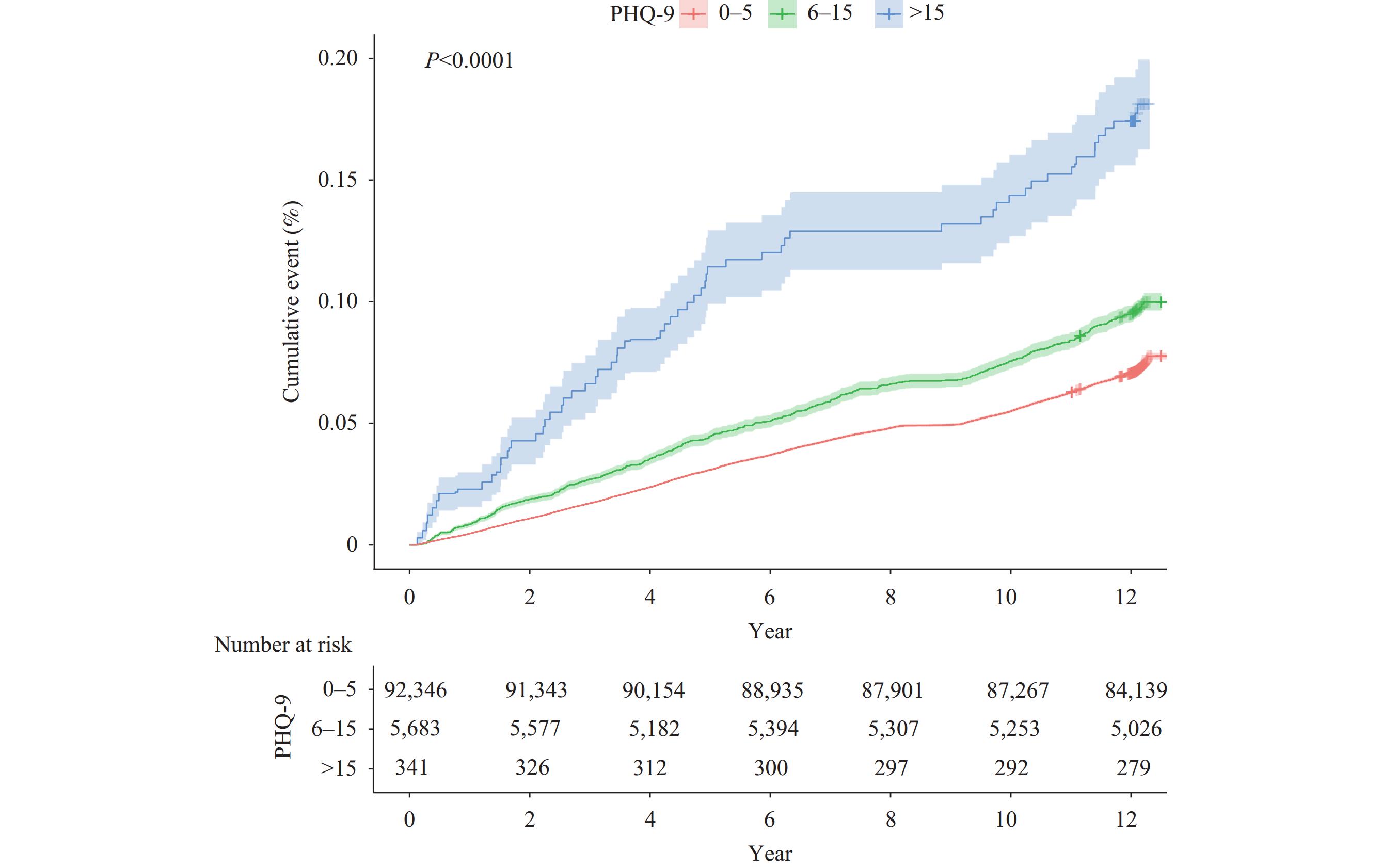 Figure 1.
Figure 1.Cumulative mortality rate (%) throughout the study period, categorized by level of depression.
Subgroups Number of death (n) ASMR (per 1,000 person-year) Model 1 (HR, 95% CI) Model 2 (HR, 95% CI) Model 3 (HR, 95% CI) Overall PHQ≤5 6,716 6.61 1.00 1.00 1.00 5<PHQ≤15 556 7.84 1.20 (1.10, 1.31) 1.18 (1.08, 1.29) 1.12 (1.03, 1.23) PHQ>15 61 12.64 2.05 (1.59, 2.64) 2.00 (1.55, 2.58) 1.88 (1.46, 2.43) Sex Men PHQ≤5 3,863 8.10 1.00 1.00 1.00 5<PHQ≤15 242 10.40 1.19 (1.04, 1.35) 1.17 (1.03, 1.34) 1.09 (0.95, 1.24) PHQ>15 29 25.98 2.89 (2.00, 4.17) 2.75 (1.90, 3.97) 2.60 (1.80, 3.77) Women PHQ≤5 2,853 5.33 1.00 1.00 1.00 5<PHQ≤15 314 6.63 1.20 (1.07, 1.35) 1.19 (1.05, 1.34) 1.15 (1.02, 1.30) PHQ>15 32 8.66 1.59 (1.11, 2.26) 1.56 (1.09, 2.22) 1.49 (1.05, 2.13) Urban-rural Urban PHQ≤5 2,727 5.61 1.00 1.00 1.00 5<PHQ≤15 209 6.65 1.22 (1.06, 1.41) 1.21 (1.05, 1.39) 1.16 (1.01, 1.35) PHQ>15 34 13.86 2.61 (1.86, 3.66) 2.56 (1.82, 3.60) 2.34 (1.66, 3.31) Rural PHQ≤5 3,987 7.51 1.00 1.00 1.00 5<PHQ≤15 348 8.85 1.19 (1.07, 1.33) 1.19 (1.06, 1.33) 1.12 (1.00, 1.26) PHQ>15 28 11.08 1.66 (1.14, 2.42) 1.61 (1.11, 2.35) 1.56 (1.06, 2.28) Age (year) ≤60 PHQ≤5 2,916 3.31 1.00 1.00 1.00 5<PHQ≤15 242 4.37 1.41 (1.24, 1.61) 1.40 (1.23, 1.60) 1.31 (1.14, 1.50 PHQ>15 20 6.33 2.13 (1.37, 3.30) 2.14 (1.37, 3.32) 2.02 (1.29, 3.15) >60 PHQ≤5 3,799 21.41 1.00 1.00 1.00 5<PHQ≤15 315 23.37 1.07 (0.96, 1.20) 1.05 (0.93, 1.18) 1.01 (0.90, 1.14) PHQ>15 41 40.63 1.99 (1.46, 2.70) 1.89 (1.39, 2.57) 1.79 (1.31, 2.44) Education Less than lower secondary PHQ≤5 4,522 7.53 1.00 1.00 1.00 5<PHQ≤15 424 9.05 1.19 (1.07, 1.31) 1.17 (1.06, 1.30) 1.12 (1.01, 1.25) PHQ>15 42 10.80 1.71 (1.26, 2.33) 1.64 (1.21, 2.24) 1.57 (1.15, 2.13) Lower secondary
and abovePHQ≤5 2,194 5.19 1.00 1.00 1.00 5<PHQ≤15 132 5.74 1.26 (1.06, 1.51) 1.26 (1.05, 1.50) 1.17 (0.97, 1.40) PHQ>15 19 17.14 3.47 (2.21, 5.44) 3.47 (2.21, 5.45) 2.98 (1.88, 4.70) BMI (kg/m2) <24.0 PHQ≤5 3,789 7.17 1.00 1.00 1.00 5<PHQ≤15 282 7.48 1.05 (0.93, 1.18) 1.03 (0.91, 1.17) 0.97 (0.86, 1.10) PHQ>15 37 14.37 2.30 (1.64, 3.21) 2.22 (1.59, 3.11) 2.16 (1.55, 3.02) ≥24.0 PHQ≤5 2,927 6.00 1.00 1.00 1.00 5<PHQ≤15 274 8.30 1.41 (1.24, 1.59) 1.38 (1.22, 1.57) 1.33 (1.16, 1.51) PHQ>15 24 10.94 1.74 (1.16, 2.61) 1.70 (1.14, 2.56) 1.62 (1.07, 2.44) Note: Model 1: adjusted by demographic factors (sex, age, urbanity, marital status, and education). Model 2: adjusted by behavioral factors (smoking status, alcohol intake, diet, physical activity, and sleep time) based on model 1. Model 3: adjusted by metabolic factors (BMI, blood pressure, lipids, and glucose) and history of diseases (myocardial infarction, stroke, chronic obstructive pulmonary disease, and cancer) based on model 2.
Abbreviation: PHQ=patient health questionnaire; HR=hazard ratio; CI=confidence interval.Table 2. HRs and 95% CI for the risk of all-cause mortality by depression level: overall and in different subgroups.
Severe depression was linked to an increased risk of death from suicide (HR=5.13, 95% CI: 1.15–22.81), non-suicide injuries (HR=3.23, 95% CI: 1.21, 8.60), and cardiovascular diseases (HR=1.71, 95% CI: 1.14, 2.55) as shown in Table 3.
Cause 5<PHQ≤15 PHQ>15 Vascular 1.09 (0.94, 1.25) 1.71 (1.14, 2.55) Cancer 1.12 (0.94, 1.34) 1.19 (0.63, 2.25) Non-suicide injury 0.92 (0.58, 1.46) 3.23 (1.21, 8.60) Suicide 1.03 (0.44, 2.37) 5.13 (1.15, 22.81) Other 1.16 (0.98, 1.39) 1.84 (1.12, 3.01) Note: HRs was adjusted by demographic factors (sex, age, urbanity, marital status and education), behavioral factors (smoking status, alcohol intake, diet, physical activity, and sleep time), metabolic factors (BMI, blood pressure, lipids and glucose) and history of diseases (myocardial infarct, stroke, chronic obstructive pulmonary disease and cancer).
Abbreviation: ASMR=age-standardized mortality rate; BMI=body mass index; PHQ=patient health questionnaire; HR=hazard ratio; CI=confidence interval.Table 3. HRs and 95% CI for the risk of cause-specific mortality based on depression level, in comparison to individuals with no depression (PHQ≤5).
-
Utilizing data from a population-based cohort, we discovered a direct correlation between depression and mortality. This association was particularly significant among males, urban residents, younger individuals, and those with higher education levels. Individuals with depression faced an elevated risk of mortality from both injuries and cardiovascular diseases.
The results aligned with a prior UK Biobank (UKB) study (4) that found a correlation between lifetime depression and overall mortality (HR=1.46, 95% CI: 1.40, 1.52). Additionally, a US study (3) indicated that a 5-point rise in PHQ-9 score was associated with increased mortality in individuals with and without CVD risk (HR=1.33, 95% CI: 1.14, 1.55; HR=1.26, 95% CI: 1.02, 1.56, respectively).
One potential explanation for the impact of depression is its correlation with unhealthy habits like smoking and limited physical activity (6). Additionally, we observed a similar association in the baseline characteristics. Another plausible mechanism is depression's influence on metabolic functions, particularly lipid metabolism, which may contribute to the development of ischemic heart disease (7).
It is concerning that among individuals with severe depression, the mortality rate for men was three times higher than that of women despite a higher prevalence of depression among women. Urban, younger, and highly educated individuals were more significantly impacted by depression despite belonging to relatively advantaged subgroups that have been less studied in the past. These disparities may stem from distinct psychological and behavioral responses to depression among different subgroups; for instance, men were less likely to seek help compared to women (8), and younger individuals experienced higher levels of depression-related stigma than older individuals (9). Our findings highlight the importance of addressing the mental health needs of these individuals, even though they may be perceived as having better physical and socio-economic circumstances.
Depression is significantly linked to mortality from cardiovascular diseases and injuries, indicating the need for tailored interventions. While prior research has mainly concentrated on the connection between depression and suicide, it is essential to recognize that depression influences non-suicidal injuries as well. Individuals with depression face an elevated risk of fatalities due to accidents and interpersonal violence (10).
The findings suggest strategies to mitigate negative health consequences in individuals with depression. It is recommended to offer psychological interventions to all individuals with depression, regardless of symptom severity. Specifically, increased physical and psychological support is advised for men, urban residents, younger individuals, and those with higher education levels. Moreover, beyond averting suicide and cardiovascular issues, implementing safety precautions is crucial for the prevention of accidental injuries.
This study is subject to some limitations. First, self-reported depression may introduce reporting bias. Second, using PHQ-9 for depression screening is less reliable than clinical diagnosis, though a PHQ-9 score >15 showed 95% specificity in depression diagnosis (5). Third, the limited number of individuals with depression led to wide confidence intervals in some subgroups. Additionally, the survey lacked data on medication usage and genetic factors.
In conclusion, our study identified a direct correlation between depression and mortality rates. This association was notably stronger among male individuals residing in urban areas, younger age groups, and those with higher education levels. Moreover, the impact was particularly significant concerning fatalities from injuries and cardiovascular conditions. Enhanced physical and psychological support should be prioritized for individuals with depression, with a heightened attention to those belonging to high-risk subgroups.
HTML
| Citation: |




 Download:
Download:




