-
Myopia is a widespread visual condition affecting individuals worldwide, with a notably high prevalence among Chinese students. In regions with a high prevalence of myopia, such as China, utilizing highly sensitive indicators for precise myopia prediction among non-myopic populations has significant public health implications. The prevalence of myopia in Chinese children and adolescents is alarmingly high, with rates of 72% and 81% among middle school (ages 11–13 years) and high school (ages 14–17 years) students, respectively, resulting in an overall prevalence of approximately 54%. Myopia not only causes various vision-threatening ocular complications, such as cataracts, glaucoma, and blindness, but also detrimentally affects children’s physical fitness, mental health, and academic performance (1). The prevalence of myopia and vision impairment is high among school students in Eastern China, and by the year 2050, the estimated population of myopic individuals will be 8,568,305 [95% confidence interval (CI): 8,398,977, 8,737,633] for those aged 7–12 years and 15,766,863 (95% CI: 15,744,826, 15,788,900) for those aged 13–18 years (2). Precise myopia prediction and tailored health intervention reminders can encourage parents and schools to take a serious stance on myopia (3). A percentage-based approach has previously been adopted to establish alert thresholds for non-myopic children (4). A cross-sectional and cohort study was initiated in Jiangsu Province in 2018 among non-myopic students. Previous research has found that the incidence of myopia decreases with increasing baseline hyperopic reserve, suggesting that intervention for pre-myopic children with alert refraction errors (or insufficient hyperopia reserve) is important in reducing the incidence of myopia (5). To further enhance the accuracy and effectiveness of preventive measures, establishing more accurate alert thresholds (refraction error values) to prevent the onset of childhood myopia is necessary (6).
A surveillance study was conducted using data from the Student Health Surveillance program in Jiangsu Province. Data, including the 25th–95th percentiles of refractive error, were collected from multiple cities during three occasions spanning the 2018–2019 to 2022–2023 academic years. Two to three cities from three tiers of economic development in Jiangsu Province were selected: Southern (Suzhou City, Zhenjiang City), Central (Nantong City, Yangzhou City, Taizhou City), and Northern (Xuzhou City, Yancheng City). Subsequently, two to four elementary schools were chosen from each selected city. The study included all students, including non-myopic students, whose parents provided informed consent. More than 3,000 non-myopic students aged 6–12 years were included in each sampling instance using a stratified sampling method to ensure representation. Inclusion criteria were: 1) Chinese Han nationality students, aged 6 to 10 years from grades 1 to 3; 2) no other severe diseases, such as hepatitis, nephritis, and eye disease; 3) provision of informed consent from parents/guardians; and 4) school-based participant to prevent loss to follow-up. Students with baseline myopia were excluded. A total of 11,013 non-myopic students received ophthalmic examinations pre- and post-dilation. The study protocol was approved by the Institutional Review Board of Ethics committee of Jiangsu Provincial Center for Disease Control and Prevention (JSJK2021-B08-02) (4).
A cohort study was conducted to validate the myopia prediction model using data from the Eastern China Student Cohort study in Pei County, Changshu City, Yizheng City, and Dongtai City. This prospective implementation study gradually included project points in stages and levels (7). In total, 3,204 non-myopic students were included: 1) 1,176 students from a four-year cohort study in Pei County; 2) 740 students from a three-year cohort study in Changshu City; and 3) 312 and 976 students, respectively, from two-year cohort studies in Yizheng City and Dongtai City. Data were collected through physical examinations [axial length (AL), corneal curvature (CC), and post- and pre-cycloplegic refractive error] and parental questionnaires [behaviors (parental myopia, near work, outdoor activity, sleep, and sugar consumption) and basic profiles]. Statistically significant differences (P<0.05) were observed between students with myopia onset after one year of follow-up and those without influencing factors such as gender, AL, parental myopia, and near work (homework duration). These statistically significant variables were then applied to the machine learning model. Model 1 included age, gender, parental myopia, near work, and follow-up years. Model 2 included the same variables as Model 1 with the addition of AL and CC (Figure 1 and Table 1).
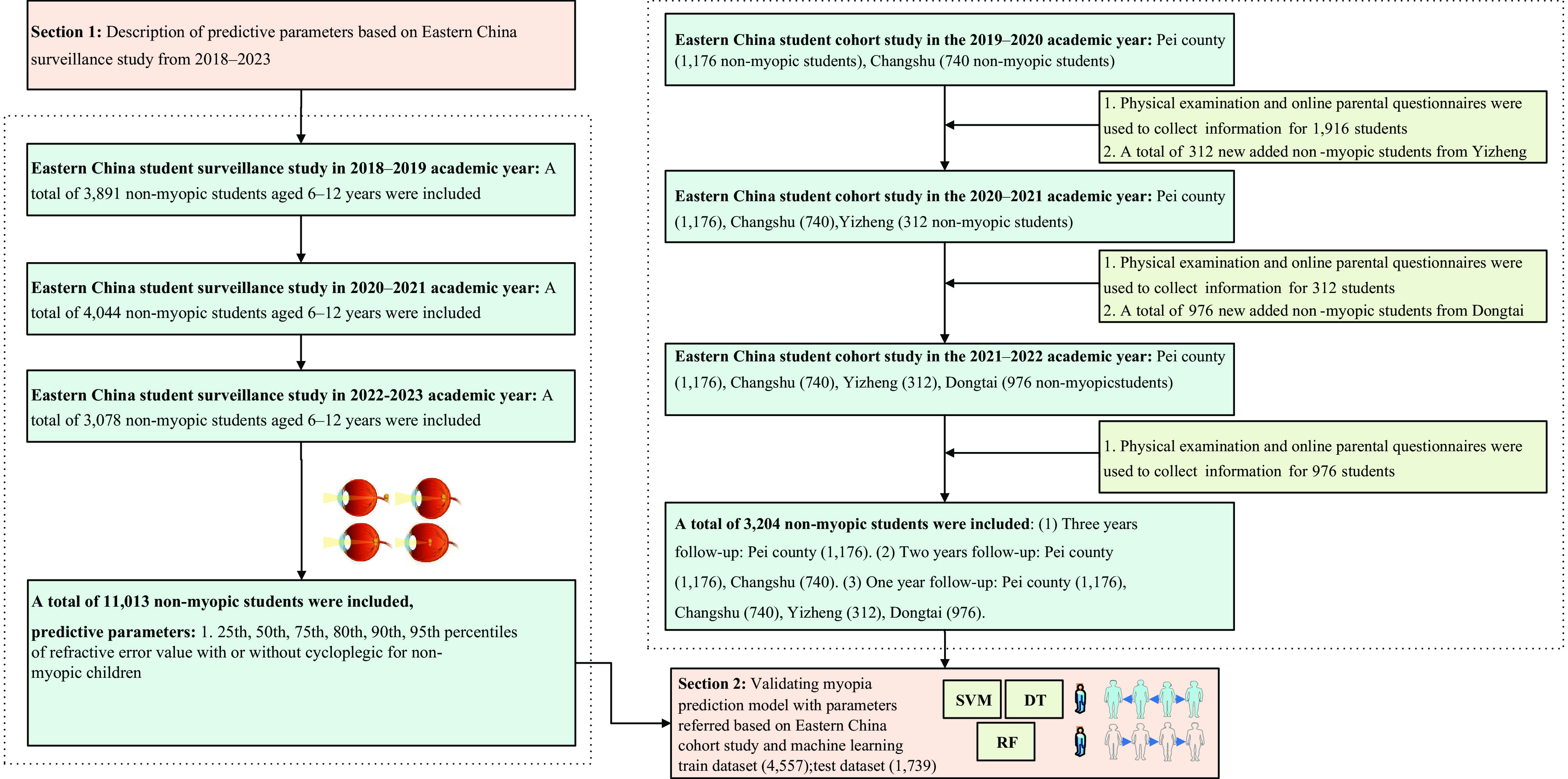 Figure 1.
Figure 1.Flowchart of student surveillance and cohort study in Jiangsu Province spanning the academic years from 2018–2019 to 2022–2023.
Variable Non-myopic students after one year follow-up (n=2,327) Students with myopia onset after one year follow-up (n=877) χ2/T/Z P Age 8.0±1.0 8.0±1.0 1.39 0.166 Female students, n (%) 989 (42.5) 445 (50.7) 17.49 <0.001 Vision (R) 5.0±0.1 5.0±0.1 1.53 0.126 Axial length (R), mm 22.9±0.8 23.2±0.7 10.20 <0.001 Cycloplegic SE (R), D 0.9 (0.5–1.1) 0.1 (−0.1–0.5) 27.81 <0.001 Corneal curvature (R), D 43.0±1.5 43.1±1.4 2.07 0.039 Height, cm 129.2±7.9 129.2±7.8 0.07 0.945 Weight, kg 29.8±8.1 30.0±8.0 0.49 0.623 Parental myopia, n (%) Father myopia 593 (25.5) 307 (35.0) 28.59 <0.001 Mother myopia 714 (30.7) 384 (43.8) 48.54 <0.001 Near work, n (%) Sitting posture (the chest is one fist distance away from the desk) 1,500 (64.5) 567 (64.7) 0.10 0.920 Sitting posture (the eyes are one foot away from the textbook) 1,432 (61.5) 510 (58.2) 3.06 0.080 Sitting posture (the fingertips are one inch away from the pen tip) 1,142 (49.1) 429 (48.9) 0.01 0.936 Duration of monocular usage (<1 h) 1,522 (65.4) 568 (64.8) 0.12 0.735 Duration of homework (<2 h) 1,933 (83.1) 694 (79.1) 6.68 0.010 Eye exercise twice per day 2,206 (94.8) 829 (94.5) 0.10 0.758 Outdoor activity (>2 h), n (%) 262 (11.3) 95 (10.8) 0.12 0.732 Sleep duration (h) 9.2±0.8 9.2±0.8 0.05 0.957 Sugar drink per week, n (%) 688 (29.6) 278 (31.7) 1.38 0.241 Sugar food per week, n (%) 185 (8.0) 60 (6.8) 1.11 0.292 Abbreviation: SE=spherical equivalent. Table 1. Distribution of baseline characteristics among non-myopic students from a cohort study (n=3,204).
Ophthalmic examinations were conducted by skilled nurses and doctors. Students participating in the myopia screening underwent refractive examinations using a fully automated computerized refractometer (TOPCON RM800/KR800) following pupil dilation with compound tropicamide eye drops to determine their refractive status. AL and CC were assessed using NIDEK AL-Scan Quality Control for the survey supervised by a dedicated professional. The screening equipment and refractometer conformed to ISO-10342 standards for ophthalmic instruments (8–9). Myopia was defined as cycloplegic spherical equivalent refraction (SER) ≤−0.50 D (10). Non-myopic students were defined as students with cycloplegic SER >−0.50 D. Refraction error percentiles were calculated using data on cycloplegic and non-cycloplegic refraction error from the survey, stratified by gender and age among non-myopic students. This calculation was performed for the 25th, 50th, 75th, 80th, 90th, and 95th percentiles. The Z-score was calculated for each data set, taking into account location (median), scale (approximate coefficient of variation), skewness (power transformation for symmetry), and kurtosis (degrees of freedom or power exponential parameter) to represent the distribution of each age–gender group (11). For machine learning analysis, 70% of the dataset was dedicated to model training, with the remaining 30% reserved for evaluating model performance. This study evaluated four prominent machine learning models: support vector machine (SVM), random forest (RF), and decision tree (DT). The key performance metric was the area under the curve (AUC) derived from the receiver operating characteristic (ROC) curve. To improve result reliability, a 95% CI for AUC was computed.
The 50th percentile refractive error values with cycloplegia for non-myopic boys were 0.63 D at age 6 years, decreasing to 0.50 D at 7 years, 0.38 D at 8 years, and 0.25 D at 10 years, and 0.16 D by age 12 years. This value remained consistent at 0.38 D between ages 8 and 9 years and at 0.25 D between ages 10 and 11 years. Without cycloplegia, the 50th percentile refractive error values for non-myopic boys were 0.0 at ages 6 and 7 years, decreasing to −0.13 D at ages 8 and 9 years, −0.25 D at age 10 years, and −0.38 D at ages 11 and 12 years. Detailed information is shown in Table 2.
Age, years Percentiles of cycloplegic refractive error Male, D Female, D Percentiles of non-cycloplegic refractive error Male, D Female, D 6 25th 0.13 0.13 25th −0.25 −0.25 50th 0.63 0.63 50th 0.00 0.00 75th 1.00 1.13 75th 0.38 0.38 80th 1.13 1.25 80th 0.38 0.50 90th 1.38 1.50 90th 0.63 0.75 95th 1.75 1.88 95th 0.88 1.00 7 25th 0.13 0.13 25th −0.38 −0.38 50th 0.50 0.63 50th 0.00 0.00 75th 0.88 1.00 75th 0.35 0.25 80th 1.00 1.13 80th 0.38 0.38 90th 1.25 1.38 90th 0.63 0.63 95th 1.50 1.63 95th 0.88 0.88 8 25th 0.00 0.00 25th −0.50 −0.50 50th 0.38 0.38 50th −0.13 −0.13 75th 0.75 0.75 75th 0.13 0.13 80th 0.88 0.88 80th 0.25 0.25 90th 1.13 1.13 90th 0.50 0.50 95th 1.50 1.50 95th 0.75 0.71 9 25th 0.00 0.00 25th −0.50 −0.50 50th 0.38 0.38 50th −0.13 −0.18 75th 0.75 0.72 75th 0.13 0.13 80th 0.88 0.80 80th 0.25 0.13 90th 1.13 1.12 90th 0.50 0.38 95th 1.50 1.38 95th 0.75 0.63 10 25th −0.13 −0.13 25th −0.50 −0.50 50th 0.25 0.25 50th −0.25 −0.38 75th 0.63 0.63 75th 0.13 0.00 80th 0.63 0.75 80th 0.13 0.13 90th 1.00 1.00 90th 0.44 0.38 95th 1.25 1.36 95th 0.63 0.63 11 25th −0.13 −0.13 25th −0.50 −0.50 50th 0.25 0.13 50th −0.38 −0.38 75th 0.50 0.63 75th 0.00 0.00 80th 0.63 0.75 80th 0.13 0.13 90th 0.88 1.00 90th 0.38 0.38 95th 1.25 1.33 95th 0.38 0.63 12 25th −0.13 −0.13 25th −0.50 −0.50 50th 0.16 0.13 50th −0.38 −0.50 75th 0.50 0.44 75th 0.00 −0.13 80th 0.63 0.63 80th 0.13 0.00 90th 0.88 0.88 90th 0.38 0.25 95th 1.25 1.19 95th 0.38 0.54 Table 2. Percentiles of refractive error value with and without cycloplegia for non-myopic children sorted by age and gender from a surveillance study in Jiangsu Province, China, 2018–2023.
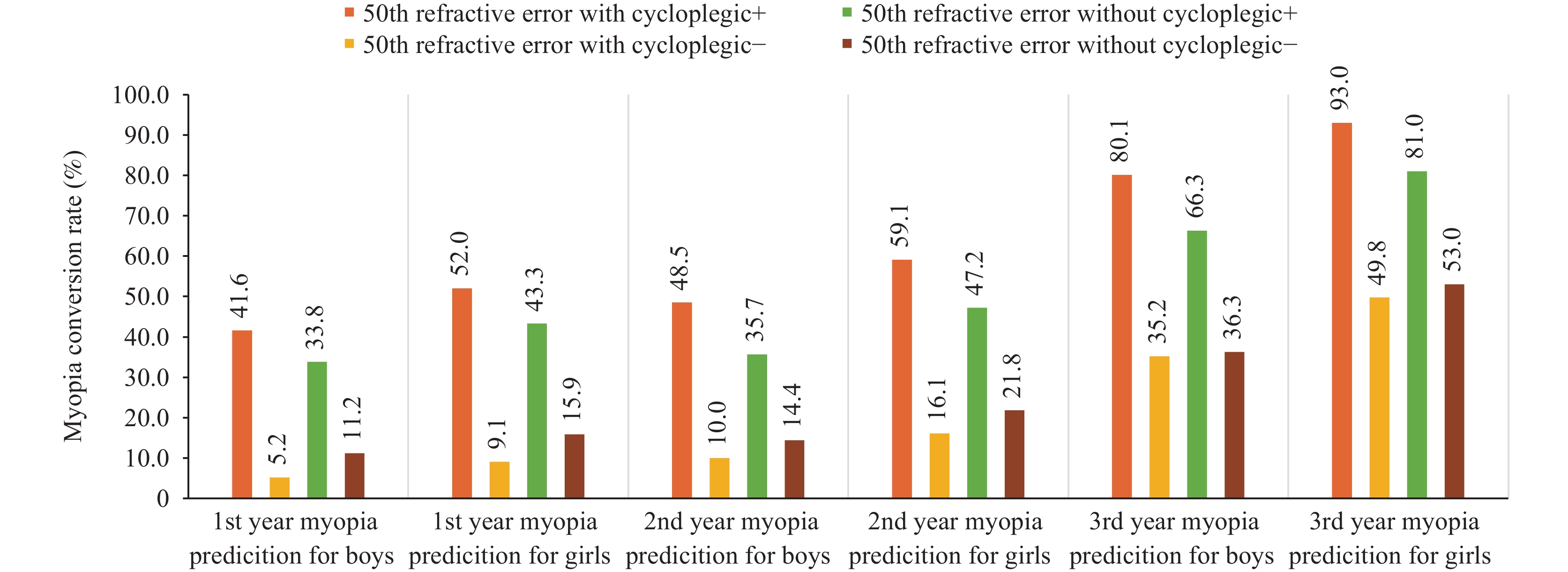
Myopia prediction performance based on machine learning: First, for students in Jiangsu Province, the amalgamated predictive model encompassing the “50th percentile of refractive error with cycloplegic,” “questionnaire (age, gender, parental myopia, and near work),” and “AL and CC” demonstrated superior predictive efficacy, yielding an AUC of 0.83, 0.85, and 0.80. The 50th percentile of AUC values across the three machine learning models (SVM, RF, and DT) surpassed those of Model 1 and Model 2, and these differences were statistically significant (P<0.05). Second, the AUC values for the combination of “50th percentile of refractive error without cycloplegic” + “questionnaire” across the three machine learning models (SVM, RF, and DT) all outperformed that of Model 1 (P<0.05). Furthermore, Model 2 demonstrated higher AUC values than Model 1 for SVM, RF, and DT (P<0.05) (Table 3). If a student attained the 50th percentile refractive error with cycloplegia, the likelihood of developing myopia within the subsequent year was 7-fold higher for boys and 4.7-fold higher for girls compared with students who did not reach the 50th percentile refractive error (Figure 2).
Predictive parameters (Train∶Test=7∶3) AUC (SVM)* AUC (RF)* AUC (DT)* Model 1* 0.66 (0.63–0.68) 0.72 (0.69–0.74) 0.63 (0.61–0.65) Model 1+0th refractive error with cycloplegic 0.68 (0.65–0.71) 0.72 (0.69–0.74) 0.63 (0.61–0.65) Model 1+25th refractive error with cycloplegic 0.78 (0.75–0.80) 0.81 (0.79–0.84) 0.77 (0.74–0.79) Model 1+50th refractive error with cycloplegic 0.80 (0.78–0.82) 0.84 (0.82–0.86) 0.80 (0.77–0.82) Model 1+75th refractive error with cycloplegic 0.75 (0.72–0.77) 0.78 (0.76–0.81) 0.77 (0.74–0.79) Model 1+0th refractive error without cycloplegic 0.68 (0.65–0.71) 0.72 (0.69–0.74) 0.63 (0.61–0.65) Model 1+25th refractive error without cycloplegic 0.70 (0.68–0.73) 0.75 (0.73–0.77) 0.64 (0.62–0.66) Model 1+50th refractive error without cycloplegic 0.72 (0.69–0.74) 0.77 (0.75–0.79) 0.70 (0.68–0.73) Model 1+75th refractive error without cycloplegic 0.70 (0.68–0.73) 0.77 (0.74–0.79) 0.64 (0.61–0.66) Model 2† 0.78 (0.75–0.80) 0.78 (0.75–0.80) 0.69 (0.67–0.72) Model 2+0th refractive error with cycloplegic 0.78 (0.75–0.80) 0.78 (0.76–0.81) 0.69 (0.67–0.72) Model 2+25th refractive error with cycloplegic 0.81 (0.79–0.84) 0.84 (0.82–0.86) 0.77 (0.74–0.79) Model 2+50th refractive error with cycloplegic 0.83 (0.81–0.85) 0.85 (0.83–0.86) 0.80 (0.77–0.82) Model 2+75th refractive error with cycloplegic 0.80 (0.78–0.82) 0.81 (0.79–0.83) 0.77 (0.74–0.79) Model 2+0th refractive error without cycloplegic 0.78 (0.75–0.80) 0.78 (0.76–0.81) 0.69 (0.67–0.72) Model 2+25th refractive error without cycloplegic 0.78 (0.76–0.80) 0.80 (0.78–0.82) 0.71 (0.69–0.74) Model 2+50th refractive error without cycloplegic 0.78 (0.76–0.81) 0.80 (0.78–0.83) 0.70 (0.67–0.72) Model 2+75th refractive error without cycloplegic 0.78 (0.76–0.80) 0.80 (0.78–0.82) 0.71 (0.69–0.74) Abbreviation: SVM=support vector machine; RF=random forest; DT=decision tree; AUC=area under the curve; AL=axial length.
* Model 1: Baseline information from questionnaires: age, gender, parental myopia, near work, follow-up years (1 to 3);
† Model 2: Model1+ biometric parameters including AL and corneal curvature.Table 3. Myopia prediction performance based on machine learning.
-
When conducting myopia screenings using pupil dilation for non-myopic populations, the cycloplegic 50th percentile refractive error emerges as a more precise predictive indicator. A series of age- and gender-based SE threshold values were established to predict myopia in Chinese children aged 6 to 12 years. This aligns with the findings of a previous cross-sectional study (4), in which the 50th prediction model (RF, SVM, DT) achieved the best AUC values. When non-myopic students reach the 50th percentile cycloplegic refractive error value, the likelihood of myopia onset in the subsequent year increases 7-fold for boys and 4.7-fold for girls, compared to the control group. The proposed precise refractive error values aim to encourage schools and parents to heighten their awareness to prevent myopia onset. Targeted public intervention measures will also be promptly directed at these children. In China, non-dilated screening methods are widely deployed in large-scale population screenings due to their practicality and efficiency. This study advocates for incorporating AL and CC as supplementary indicators in screenings, augmenting the sole use of noncycloplegic refractive error.
The 50th reference value for non-myopic individuals determined in this study has practical utility for subsequent precision interventions in Jiangsu Province. Myopia prediction using baseline refraction or biometric data dates back to 1999, when Zadnik et al. (12–13) attempted to forecast the onset of juvenile myopia. This study incorporated behavioral factors such as parental myopia and near work; nevertheless, their predictive effectiveness was less than satisfactory. Using SCORM data, Chua et al. (14) found that the age of myopia onset alone can effectively predict high myopia (AUC=0.85). Incorporating additional factors, such as school attendance and weekly book reading, only slightly improved the prediction accuracy (AUC=0.87).
In China, the governmental approach to school screening predominantly relies on noncycloplegic refractions, and the Chinese Ministry of Health derives myopia prevalence reports from these school-screening assessments. Widely adopted in large-scale population screenings due to their practicality and efficiency, nondilated screening methods have inherent limitations, particularly in evaluating refractive errors such as myopia. With the SVM machine learning model, the predictive performance (AUC=0.78) significantly surpasses that of the 50th percentile noncycloplegic refractive error (AUC=0.72) (P<0.05). Hence, incorporating AL and CC in nondilated screenings warrants consideration. However, significant biases exist in current screening programs when evaluating younger students. This study provides objective data on two screening modes: dilated and nondilated. In areas where feasible, such as economically developed regions, large-scale implementation of dilated screening may be possible.
This study was subject to some limitations. First, the influence of gene-environment interactions on myopia prediction was not explored. Second, because of limitations in longitudinal data collection, this study only made predictions for 1–3 years. Follow-up with this cohort is planned for the later stages.
-
No conflicts of interest.
-
Professor Genming Zhao, Professor Fengyun Zhang, Professor Jun Ma, Professor Fangbiao Tao, Professor Hu Liu, and Professor Hongsheng Bi; We also thank to over 100 on-site collaborators and educators from various centers of this project.
HTML
| Citation: |



 Download:
Download: