-
The new conceptual framework, small and vulnerable newborns (SVN), encompasses preterm birth, small for gestational age (SGA), and low birth weight (LBW). This framework identifies these high-risk infants, who share a markedly increased risk of short-term and long-term adverse consequences, as a single group (1). There are two primary reasons for adopting this framework: first, using any of the three individual definitions would underestimate the number of high-risk newborns by 50% (2); and second, because the three definitions are not mutually exclusive, assessing the total burden on a region or country becomes difficult. This study aimed to assess the burden trends of high-risk newborns in Beijing from 2013 to 2022 under this new SVN conception, using data collected from the Maternal and Children Information System in Beijing Municipality, China. The study among 2,005,408 newborns found an increasing incidence of SVN in Beijing, with rates rising from 9.82% of births in 2013 to 10.96% in 2022. Additionally, the average incidence over the ten years for SVN, preterm birth, SGA, and LBW were 9.94%, 6.35%, 4.51%, and 4.80%, respectively. Notably, while the incidence of preterm-SGA and preterm-nonSGA showed a significant rising trend, the incidence of term-SGA decreased significantly. It is essential for public health practitioners to adopt this new conceptual framework to better estimate the total burden of high-risk newborns. Considering the increasing trends over the past decade, more interventions should be implemented to reduce the burden on high-risk newborns, especially for preterm infants, regardless of SGA status.
SVN include preterm, SGA, and LBW infants. Since these three definitions are not mutually exclusive, SVN births can be classified into three mutually exclusive types: 1) preterm-SGA: newborns who are both preterm and SGA, 2) preterm-nonSGA: newborns who are preterm but not SGA, and 3) term-SGA: newborns who are born at term but are SGA (1).
This study utilized data from the Maternal and Children Information System in Beijing, a registry for births. All midwifery agencies in Beijing are required to register birth information, including birth weight and gestational age. SVN were defined as newborns who were preterm (<37 weeks of gestational age), had LBW (<2,500 g at any gestational age), or had a birth weight less than the 10th percentile for gestational age according to the “Reference Standards for Fetal Weight Estimation at different gestational age in Chinese Population” in the Expert Consensus on Fetal Growth Restriction (2019 edition). This classification can be divided into three mutually exclusive types: term-SGA, preterm-SGA, and preterm-nonSGA. Non-live births and births with a gestational age of less than 28 weeks were excluded.
A linear regression model, implemented in R software (version 4.4.0; The R Foundation for Statistical Computing, Vienna, Austria), was used to analyze the trend between year and incidence of SVN. Logistic regression, also conducted in R software, was used to estimate the association between biological characteristics and SVN and its subtypes. Results were expressed as adjusted odds ratios (aORs) with 95% confidence intervals (CIs). P values equal to or less than 0.05 (two-tailed) were considered statistically significant.
Between 2013 and 2022, a total of 2,005,408 births were recorded. Of these, 96,236 (4.80%) were LBW babies, 127,422 (6.35%) were preterm births, and 90,508 (4.51%) were SGA babies. Using the new definition, 199,254 (9.94%) were SVN babies. The basic characteristics of the births are displayed in Table 1.
Variable Total, N (%) Preterm, N (%) LBW, N (%) SGA, N (%) SVN, N (%) Sexual Boy 1,042,072 (51.96) 70,629 (6.78) 46,368 (4.45) 34,715 (3.33) 97,001 (9.31) Girl 963,038 (48.02) 56,750 (5.89) 49,813 (5.17) 55,743 (5.79) 102,179 (10.61) Gender ambiguity 298 (0.01) 43 (14.43) 54 (18.12) 49 (16.44) 73 (24.5) Number of birth Single birth 1,940,193 (96.75) 97,382 (5.02) 66,841 (3.45) 76,613 (3.95) 161,920 (8.35) Multiple births 65,215 (3.25) 30,040 (46.06) 29,395 (45.07) 13,895 (21.31) 37,334 (57.25) Mode of delivery Vaginal delivery 1,162,877 (57.99) 48,965 (6.75) 33,665 (2.89) 46,251 (3.98) 91,077 (7.83) Cesarean section 842,435 (42.01) 78,447 (5.81) 62,563 (7.43) 44,250 (5.25) 108,164 (12.84) Total 2,005,408 (100.00) 127,422 (6.35) 96,236 (4.80) 90,508 (4.51) 199,254 (9.94) Abbreviation: LBW=low birth weight; SGA=small for gestational age; SVN=small and vulnerable newborns. Table 1. Basic characteristics of births in Beijing Municipality, China, from 2013 to 2022 (N=2,005,408).
Figure 1 illustrates the trends in incidence for each subtype between 2013 and 2022. Over this period, the incidence of SVN demonstrated an increasing trend, rising from 9.82% in 2013 to 10.96% in 2022 (Linear Regression, t=4.597, P=0.002). The incidence of both preterm-SGA and preterm-nonSGA also manifested upward trends. Preterm-SGA incidence climbed from 0.80% in 2013 to 1.11% in 2022 (Linear Regression, t=8.905, P=0.000), while preterm-nonSGA incidence rose from 4.43% to 6.34% (Linear Regression, t=5.674, P=0.000). In contrast, the incidence of term-SGA decreased from 4.60% in 2013 to 3.51% in 2022 (Linear Regression, t=−2.582, P=0.033).
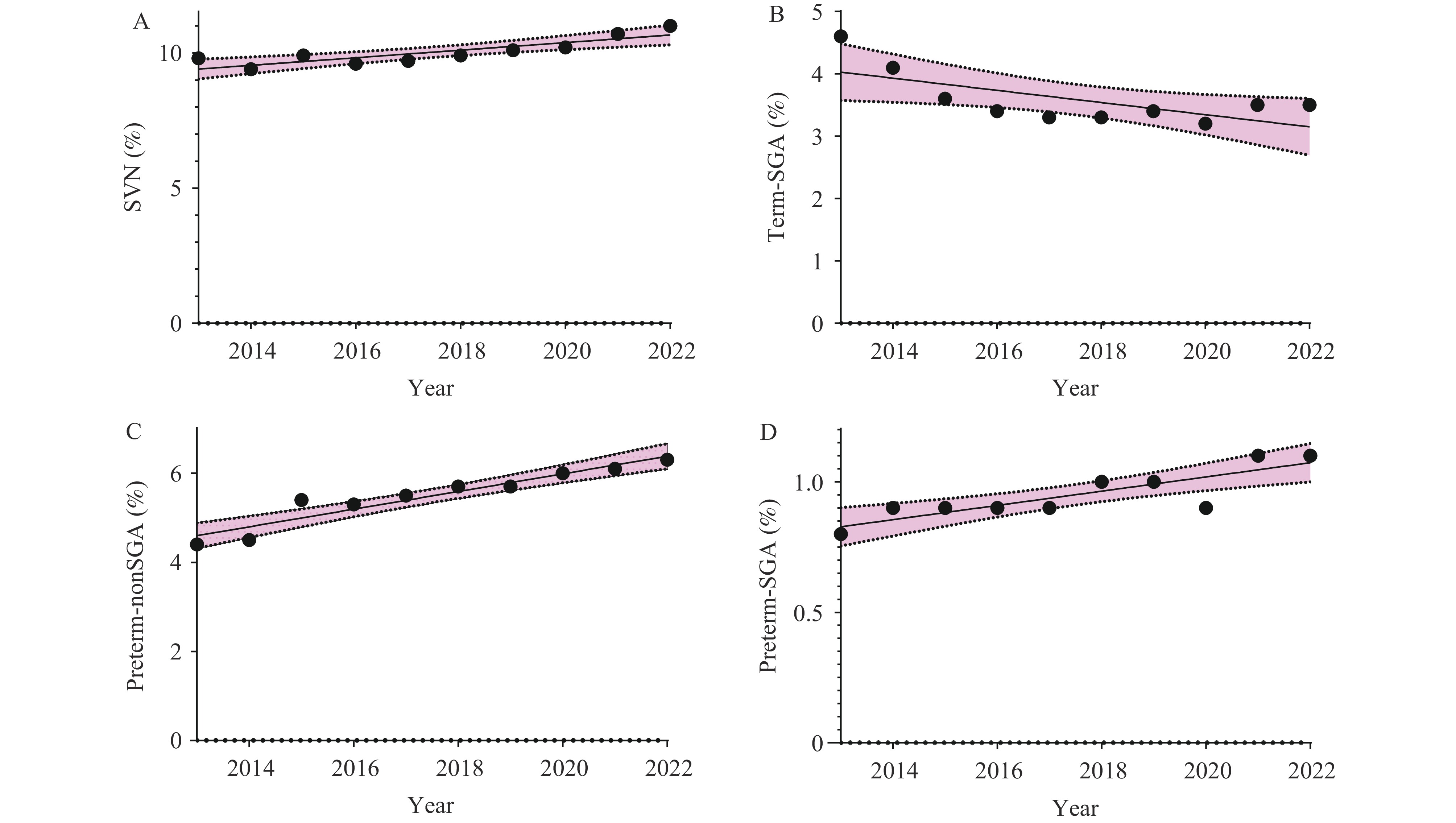 Figure 1.
Figure 1.Trends between years and incidence of high-risk newborns by linear regression, in Beijing, China, from 2013 to 2022 (%). (A) The trend between years and incidence of SVN (t=4.597, P=0.002). (B) The trend between years and incidence of term-SGA (t=−2.582, P=0.033). (C) The trend between years and incidence of preterm-nonSGA (t=5.674, P=0.000). (D) The trend between years and incidence of preterm-SGA (t=8.905, P=0.000).
Abbreviation: SVN=small and vulnerable newborns; Preterm-SGA=preterm newborns also small for gestational age; Preterm-nonSGA=preterm newborns but not small for gestational age; Term-SGA=term newborns but small for gestational age.Table 2 presents the associations between biological characteristics and SVN subtypes, as estimated by logistic regression. Maternal age, parity, and number of births were adjusted for in the model. Maternal age was not associated with term-SGA newborns. However, multiple pregnancies (aOR=6.98, 95% CI: 6.79, 7.17) and primiparity (aOR=2.11, 95% CI: 2.07, 2.15) were associated with an increased risk of term-SGA newborns. Multiple pregnancies were also a significant predictor for both preterm-nonSGA (aOR=17.15, 95% CI: 16.83, 17.48) and preterm-SGA newborns (aOR=32.75, 95% CI: 31.70, 33.84).
Variable Term-SGA*
(N=71,832)Preterm-SGA *
(N=18,676)Preterm-nonSGA*
(N=108,746)SVN*
(N=199,254)aOR (95% CI) aOR (95% CI) aOR (95% CI) aOR (95% CI) Parity Multipara Reference Reference Reference Reference Primipara 2.11 (2.07, 2.15) 1.43 (1.44, 1.54) 0.97 (0.96, 0.98) 1.31 (1.29, 1.32) Age, years <35 Reference Reference Reference Reference 35–40 0.92 (0.90, 0.94) 1.41 (1.36, 1.47) 1.40 (1.38, 1.42) 1.23 (1.22, 1.25) ≥40 1.01 (0.95, 1.06) 2.17 (2.01, 2.33) 1.88 (1.82, 1.95) 1.60 (1.56, 1.65) Number of births Single birth Reference Reference Reference Reference Multiple birth 6.98 (6.79, 7.17) 32.75 (31.70, 33.84) 17.15 (16.83, 17.48) 14.10 (13.91, 14.38) Abbreviation: SVN=small and vulnerable newborns; Preterm-SGA=preterm newborns also small for gestational age; Preterm-nonSGA=preterm newborns but not small for gestational age; Term-SGA=term newborns but small for gestational age; aOR=adjusted odds ratio; CI=confidence interval.
* Comparison of the study group with the normal newborn group by logistic regression, adjusting for parity, maternal age, and number of births.Table 2. Risk of SVN and its subtypes in pregnant women with different biological characteristics in Beijing, China.
-
This study is the first to apply a new conceptual framework to evaluate the incidence of high-risk newborns in Beijing. Data from the Beijing Maternal and Children Information System indicate an overall SVN incidence of 9.94% over the past decade. The system also reveals incidences of 4.51% for SGA, 4.80% for LBW, and 6.35% for preterm births over the same period. Using any subtype of SVN to assess the number of high-risk newborns would lead to an underestimation of 40%–50%, a finding similar to a Brazilian study (2). The new definition encompasses SGA, LBW, and preterm birth under the umbrella term SVN. In this study, routine individual-level data collection in midwifery hospitals allows for accurate assessment of the burden associated with being born small or preterm. Because these three definitions are not mutually exclusive, a new SVN classification method is used: term-SGA, preterm-SGA, and preterm-non-SGA. Although this new classification covered 95.43% (88,355/92,586) of LBW babies in our study, slightly lower than in previous studies (1), public health practitioners are advised to use SVN when assessing the number of high-risk newborns. This recommendation is based on the new conceptual framework’s ability to better estimate the total burden of high-risk newborns.
The incidence of SVNs in this study was markedly lower than the 26.2% reported for 195 countries and areas in 2020. The global study indicated that of all SVNs, 1.1% were preterm-SGA, 8.8% were preterm-nonSGA, and 16.3% were term-SGA (3). Over the past ten years in Beijing, the incidences of SVNs (9.94%), preterm-nonSGA (5.42%), and term-SGA (3.58%) were significantly lower than global data, while the incidence of preterm-SGA (0.93%) was slightly lower. While few studies have used this new conceptual framework, previous research has shown that the incidences of preterm birth, LBW, and SGA vary significantly between countries (4–6). Similarly, preterm birth incidence varies by region within China (7). Regional differences in economic development, maternal demographic characteristics, and antenatal care capabilities should be considered when comparing SVN incidence.
The incidence of term-SGA decreased from 4.60% in 2013 to 3.51% in 2022 (linear regression, t=−2.582, P=0.033). This decrease may be partially attributed to Beijing’s status as one of the most economically developed areas in China, with a higher level of antenatal care compared to most other areas. Increasing the quantity and quality of antenatal contact with healthcare providers can reduce or prevent the birth of SVN (8). The Chinese government’s implementation of the Basic Public Health Service project in 2009, which included establishing annual maternal health records and prenatal examinations, can further improve maternal health services and reduce maternal mortality (9). Furthermore, an analysis of maternal and child healthcare quality in 31 Chinese provincial-level administrative divisions (PLADs) from 2010 to 2020, using 6 indicators (maternal mortality rate, maternal health record establishment rate, pregnancy systematic management rate, prenatal examination rate, postpartum visit rate, and hospital delivery rate), ranked Beijing among the top areas for maternal and child health quality (10). Despite the decrease in term-SGA incidence, this condition remains a concern as it accounted for 26.4% of SVN-associated neonatal deaths (1).
Despite some progress, a significant health concern remains. This study found no decrease in the incidence of SVN, with preterm-SGA and preterm-nonSGA births increasing over the past 10 years. This suggests a need for improved interventions, particularly those targeting preterm infants. Our study found a strong association between multiple pregnancies and preterm birth (preterm-SGA: aOR=32.75, 95% CI: 31.70, 33.84; preterm-nonSGA: aOR=17.15, 95% CI: 16.83, 17.48). Interventions aimed at reducing SVN should prioritize women of advanced maternal age, primiparous women, and those with multiple pregnancies.
This study is among the first to group preterm birth, SGA, and LBW together under the umbrella term SVN. This study has several additional strengths. First, the Maternal and Children Information System in Beijing collects birth data from all midwifery hospitals in the city and uses all data for birth registration, allowing it to accurately represent the occurrence of SVN in Beijing without sampling bias. Second, the diagnostic criteria for SVN are relatively objective. These criteria are based on the newborn’s birth weight and gestational age, eliminating potential diagnostic access bias due to inconsistent criteria among different midwifery hospitals.
This study was subject to some limitations. The occurrence of SVN is influenced by economic and cultural conditions. While this study offers a comprehensive representation of SVN occurrence in Beijing, it is important to note the significant variations in economic levels, basic demographic characteristics, and antenatal care quality across different regions of China. Consequently, these findings may not accurately reflect the overall SVN situation in China. In addition, the study did not take into account pregnancy-related diseases. As far as we are aware, pregnancy complications and comorbidities are among the crucial factors that significantly impact pregnancy outcomes. This study investigates the applicability of the new concept for assessing high-risk newborns in Beijing and offers insights for interventions. However, this study did not consider maternal health status; therefore, further research is needed to develop more precise interventions.
-
No conflicts of interest.
-
All the participants in this study; and all the public health practitioners involved in Maternal and Children Information System in Beijing for their great efforts in data collection.
HTML
| Citation: |



 Download:
Download:




