-
Acute respiratory infections (ARIs) are a major cause of illness and death in children under the age of five, particularly in developing countries, contributing significantly to the global burden of disease (1). The coronavirus disease 2019 (COVID-19) pandemic has changed the epidemiology of respiratory viruses and Mycoplasma pneumoniae (MP) (2–3). In response to the severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2) outbreak in Wuhan, China implemented a comprehensive and evolving zero-COVID policy to control the pandemic, which continued until December 2022. Since the relaxation of pandemic control measures, there has been a noticeable shift in the prevalence of respiratory viruses and MP. On November 22, 2023, the World Health Organization (WHO) reported clusters of undiagnosed pneumonia in children in China based on media and ProMED reports (4), which was later attributed to known pathogens such as the influenza virus and MP. However, the increase in ARIs and associated pathogens in Chinese children has garnered global attention (5). Therefore, this study aimed to determine the prevalence patterns of respiratory viruses and MP among children with ARIs in the Wuhan region from September 1 to November 30, 2023. Our findings demonstrate a persistent prevalence of MP and a growing trend of influenza.
We conducted a retrospective study at Wuhan Children’s Hospital, enrolling children with ARIs between September 1, 2023, and November 30, 2023. Specimens collected included nasopharyngeal aspirates/throat swabs or peripheral blood samples. These samples were analyzed using various methods such as real-time polymerase chain reaction (RT-PCR), targeted next-generation sequencing (tNGS), colloidal gold immunochromatographic tests, or direct immunofluorescence to detect microorganisms such as MP, respiratory syncytial virus (RSV), adenovirus (ADV), influenza A virus (IAV), influenza B virus (IBV), and parainfluenza virus (PIV). Demographic and clinical data were extracted from electronic medical records. Statistical analyses were performed using R (version 4.0.3, R Foundation for Statistical Computing, Minnesota, US) in RStudio (version 1.4.1103, RStudio, Inc., Minnesota, US) and GraphPad Prism (version 9.1.1.1, San Diego, CA). It is important to note that this study relied solely on the retrospective analysis of deidentified data. Ethical approval for this study was obtained from the Ethics Committee of Wuhan Children’s Hospital (No. 2023R016-E02).
From September 1, 2023, to November 30, 2023, a total of 70,016 patients sought consultation at Wuhan Children’s Hospital for ARIs, with 10,012 individuals requiring hospitalization. In the outpatient setting, 51,700 (73.8%) children provided peripheral blood samples for colloidal gold immunochromatographic tests to detect RSV, MP, and ADV. Nasopharyngeal aspirates from 8,977 (12.8%) children were tested for IAV and IBV. The average age of the children was 4.86 (3.27, 7.31) years, with the highest proportion belonging to the preschool age group (3–6 years) at 40.8%. The majority of the participants were male (56.2%). Out of the 51,700 outpatients included, 19,085 (36.9%) were infected with a single pathogen and 220 (0.4%) had co-infections. MP (36.2%) was the most commonly detected pathogen, followed by IAV (16.8%). Among the hospitalized patients, 7,568 (75.6%) children were included in the study for the simultaneous detection of MP, RSV, ADV, IAV, IBV, and PIV. Of the hospitalized children, 4,298 (56.7%) were male and 8,280 (38%) were school-age children (>6 years old), with an average age of 5.01 (3.12, 8.03) years. Across all tested settings, a total of 4,302 (56.8%) patients were infected with a single pathogen, while 373 (4.9%) were infected with multiple pathogens. Consistent with the findings in outpatients, MP (46.6%) showed the highest pathogen detection rate, followed by RSV (7.6%), PIV (5.9%), ADV (3.8%), and IAV (2.4%) (Table 1). During the study period, the enrollment of outpatients peaked during the second half of October, coinciding with an increase in MP detection. Additionally, the detection rate of MP remained consistently high throughout the study period. IAV continued to be detected, with a detection rate of approximately 10%, and peaked at the end of November (with a detection rate exceeding 30%). Furthermore, IBV started to be detected in late October but remained at low levels (Figure 1).
Variable
Inpatients
(n=7,568)
Outpatients
(n=51,700)Sex (male) 4,298 (56.7) 29,070 (56.2) Age (years) 5.01 (3.12, 8.03) 4.86 (3.27, 7.31) ≤1 669 (8.8) 2,958 (5.7) 1–3 1,546 (20.4) 7630 (14.8) 3–6 2,485 (32.8) 2,1087 (40.8) >6 2,868 (37.9) 20,025 (38.7) Virus detection rate 4,675 (61.8) 19,085 (36.9) Single virus 4,302 (56.8) 18,865 (36.5) Multiple viruses 373 (4.9) 220 (0.4) MP 3,532 (46.6) 18,755 (36.2) ADV 294 (3.8) 234 (0.4) IAV 182 (2.4) 1,510/8,977* (16.8) IBV 36 (0.4) 114/8,977* (1.2) RSV 576 (7.6) 324 (0.6) PIV 451 (5.9) - Note: Data are presented as mean and variance or numbers (%).
‘-’ in the last line means that in outpatient settings, PIV was not tested in detection methods.
Abbreviation: MP=Mycoplasma pneumoniae; ADV=adenovirus; IAV=influenza virus A; IBV=influenza virus B; RSV=respiratory syncytial virus; PIV=parainfluenza virus.
* In outpatient settings, 8,977 children were tested for IAV and IBV.Table 1. Demographic and clinical data of patients enrolled.
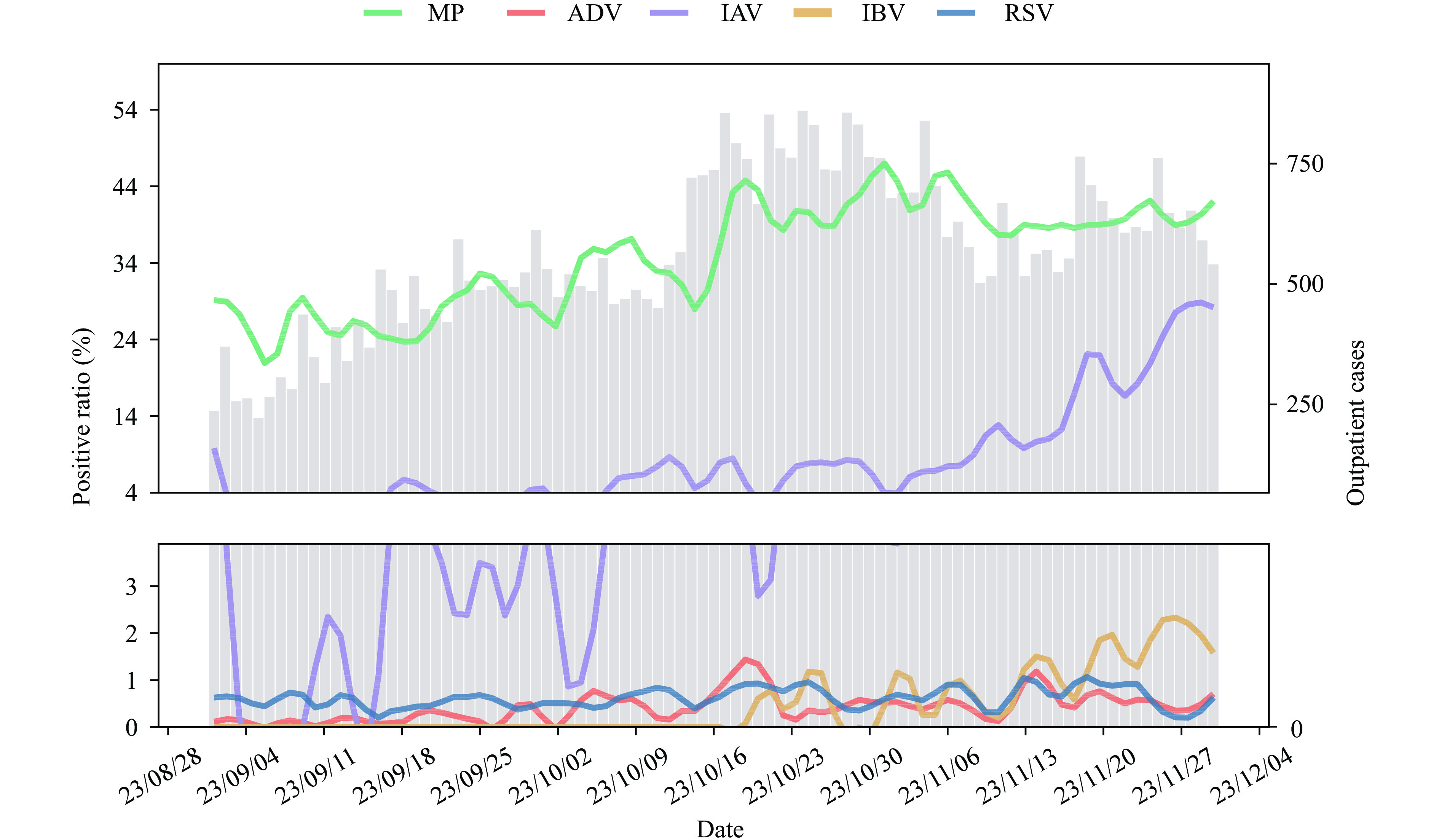 Figure 1.
Figure 1.Respiratory virus detections among enrolled children in outpatient settings. Colored lines represent the positive rate of MP and viruses over time, and the gray bar represents the number of enrolled children.
Note: Smoothed curves were generated using loess regression to enhance the visualization of trends (span=0.1).
Abbreviation: MP=Mycoplasma pneumoniae; ADV=adenovirus; IAV=influenza virus A; IBV=influenza virus B; RSV=respiratory syncytial virus.
In hospitalized patients, the detection rate of MP remains consistently high throughout the year, ranging from 30% to 60%, with the highest rates observed in October. IAV reached its peak in late November, while intermittent detections of IBV occur during this period. RSV and PIV were detected in September and October, but their numbers declined in November. ADV was consistently detected at levels below 10%. Interestingly, influenza typically peaked in late fall and winter, but the seasonal trends observed for MP and RSV in hospitalized patients differ from the expected patterns seen prior to the COVID-19 pandemic in this study (6–7) (Figure 2).
 Figure 2.
Figure 2.Respiratory virus detections among enrolled children in inpatient settings. Colored lines represent the positive rate of MP and viruses over time, and the gray bar represents the number of enrolled children.
Note: Smoothed curves were generated using loess regression to enhance the visualization of trends (span=0.1).
Abbreviation: MP=Mycoplasma pneumoniae; ADV=adenovirus; IAV=influenza virus A; IBV=influenza virus B; RSV=respiratory syncytial virus; PIV=parainfluenza virus.
-
During the period of September to November 2023, we retrospectively enrolled 51,700 outpatients and 7,568 inpatients with ARIs in our study. Children aged over 3 years accounted for more than 70% of the enrolled population, with those over 6 years comprising more than one-third of the hospitalized group. Notably, the age distribution differed from our previous study (8), which may be attributed to variations in the pathogens. For instance, MP tends to infect school-age children and was the most frequently detected pathogen across all settings, with a consistently high detection rate. This finding contradicts the seasonal prevalence trends observed prior to the COVID-19 pandemic. In contrast, the circulation of IAV aligns with previous patterns, starting in late autumn and early winter.
After the COVID-19 pandemic outbreak, several respiratory viruses experienced a significant decrease in transmission. However, unlike these other viruses, MP showed a different pattern. Initially, MP incidence decreased along with other respiratory pathogens in the first year, but in the second year, while other respiratory pathogens were resurging, the incidence of MP further decreased, indicating a decline in community transmission. Global surveillance data support this observation, showing the re-emergence of MP in Europe and Asia more than three years after the implementation of COVID-19 restrictions (9). Our findings demonstrate a notable increase in MP cases in Wuhan, which is unusual and distinct from the re-emergence pattern of other pathogens and warrants further attention.
We observed a significant decrease in the detection rate of IAV in Wuhan, with nearly 0 detection by April 2022 (8). This decline in cases resulted in the accumulation of immune debt (10). However, in the 2023–24 season, there was a rapid increase in influenza cases among outpatients, potentially indicating high activity and elevated hospitalization rates due to immune debt. Thus, it is crucial for children to receive seasonal influenza vaccinations as they are the most effective means of safeguarding against influenza and its related complications.
The findings in this report have several limitations. First, the data are restricted to individuals who underwent comprehensive pathogen testing, which may not be representative of all children seeking healthcare. Additionally, we only reported on a limited number of pathogens. While the prevalence of MP, RSV, and influenza is currently important, it would be beneficial to expand surveillance to include other respiratory pathogens. Lastly, the study was retrospective and conducted at a single center. Therefore, the establishment of a multicenter, prospective ARI surveillance system is needed.
Our study examined the epidemiological patterns of common respiratory viruses and MP, revealing the continuing prevalence of MP and a growing trend in influenza. This study emphasizes that the circulation of respiratory viruses and MP has not returned to pre-pandemic levels, highlighting the importance of enhancing surveillance for respiratory pathogens. These findings underscore the need for implementing policies to safeguard children from pathogens such as MP, influenza, and RSV.
No conflicts of interest.
-
No conflicts of interest.
HTML
| Citation: |



 Download:
Download:




