-
Acquired immunodeficiency syndrome (AIDS), which is caused by the human immunodeficiency virus (HIV), represents a significant threat to both global public health and societal progress, as this infectious disease imperils the well-being and development of human populations (1–3). In China, the HIV/AIDS epidemic remains a critical concern, with the burden of prevention and control presenting a substantial and ongoing challenge (4). While policy and regulation serve as crucial tools for governmental and administrative bodies tasked with managing AIDS, the literature has not adequately provided a systematic analysis of China’s national HIV/AIDS prevention and control policies across various stages of their implementation.
Prior research has tended to concentrate on aspects such as epidemiology, antiviral strategies, sentinel surveillance, key demographics, and legal frameworks. Studies that address HIV/AIDS policy frequently employ a traditional chronological analysis, which often suffers from issues of timeliness and scope. Consequently, a deeper investigation into the underlying patterns and logical progression of policy evolution in the context of HIV/AIDS prevention and control is warranted.
A comprehensive review and analysis of the development of HIV/AIDS prevention and control policies in China over the last four decades would not only facilitate a retrospective assessment of policy efficacy but also assess the scientific rigor and practicality of their implementation. Such an analysis could provide an invaluable foundation for the ongoing advancement and sustainability of HIV/AIDS prevention and control strategies at both the national and regional levels.
-
The dataset for this study was acquired from a comprehensive review of China’s State Council’s policy document archive, PKULAW.com (an aggregator of Chinese legal statutes, regulatory measures, and policy records), the repositories of Chinese political journals, and other authorized governmental portals. This review spanned materials from 1984 to 2022 and focused on records embedded with keywords pertinent to AIDS and HIV. A meticulous secondary filtration process was undertaken to align with the research objectives, scrutinizing the relevance, context, and applicability of the documents. Our inclusion criteria were delineated as follows: 1) issuing entities: preeminent departments within the China State Council and their directly subordinate agencies; 2) policy classifications: encompassing a spectrum from laws and regulations to advisory opinions, procedural guidelines, standards, notifications, resolutions, strategic blueprints, and synopses; 3) thematic relevance: policy narratives intrinsically connected to HIV/AIDS discourse.
Conversely, our exclusion criteria eliminated: 1) redundant iterations of policy documents; 2) records elicited by keyword searches yet devoid of substantial linkage to HIV/AIDS thematic elements; 3) ancillary documents including, but not limited to, journalistic coverage of policies, event-based orations, administrative reports, exegeses of policy frameworks, procedural advisories, staffing rosters, and commendatory citations.
-
Grounded theory is a qualitative research methodology that employs a bottom-up, empirical data-driven approach, offering systematic protocols for the collection, comparison, induction, synthesis, analysis, and conceptualization of qualitative data to formulate theories (5). This study utilized NVivo12 software (Release 1.2, QSR International, Massachusetts of USA) in conjunction with grounded theory to perform word frequency analysis, co-word cluster analysis, text content mining, coding categorization, and visual analysis of the policy text. Furthermore, this combination facilitated the construction of a policy network model and elucidated the evolutionary trajectory of HIV/AIDS prevention and control policies in China.
-
Initially, the textual data was segmented into discrete units, and one hundred open codes were generated to categorize these elements. Subsequently, cluster analysis was performed on these open codes to derive forty-six axial codes, which facilitated a detailed examination of the features and relationships between the principal categories. Ultimately, four core codes — namely “knowledge-attitude-practice (KAP),” “support,” “guarantee,” and “guidance” — were identified and synthesized (Table 1 and Figure 1). This process culminated in the development of a solar-inspired model of the HIV/AIDS prevention and control policy network (Figure 2).
Core category Main category Key concept Number of references KAP Publicity and education
Target population
Behavioral intervention
Team building and personal trainingMake relevant knowledge about HIV/AIDS prevention and control understandable to the public so that they can develop positive and correct prevention and control beliefs, attitudes, and behavioral habits that are conducive to HIV/AIDS prevention and control. 1,760 Support Care and assistance
Treatment and services
Coordinating mechanism
Legal meansBased on the soft means of humanistic care and medical services and the hard means of legal protection against illegal and criminal activities, all government departments and social organizations work together to directly promote the successful implementation of AIDS prevention and control. 626 Guarantee Monitoring and detection
Supervision
Evaluation and assessment
Funding and subsidies
Nosocomial infection and protectionHIV/AIDS prevention and control also includes the attention of the government, the clear division of labor among functional departments, the enhancement of technical level, and the improvement of the supervision and assessment mechanisms and so on, which can indirectly affect the efficiency and quality of AIDS prevention and control work. 698 Guidance Consolidated guidelines These are systematic policy texts that contain two or three types of content from the other three core categories an overall guiding meaning. 82 Abbreviation: HIV=human immunodeficiency virus; AIDS=acquired immunodeficiency syndrome; KAP=knowledge-attitude-practice. Table 1. The selective codes of HIV/AIDS prevention and control policies in China.
-
Beginning with the 1984 Joint Notice on Restricting the Import of Blood Products to Prevent the Spread of HIV/AIDS in China, issued by China’s General Administration of Customs, the former Ministry of Health, and the Ministry of Foreign Trade and Economic Cooperation, our research traced the trajectory of national policy texts. We observed an initial increase in the number of these documents over the years, followed by a subsequent decline. Upon review, a total of 192 national-level policy texts pertaining to HIV/AIDS prevention and control have been issued to date. The zenith of policy issuance occurred in 2004, with a total of 29 texts (representing 15.10% of the sample), followed by a secondary peak in 2006 with 19 texts (9.90%). Since then, the issuance of related policies has remained relatively stable (Figure 3).
 Figure 3.
Figure 3.Distribution of HIV/AIDS prevention and control policies in China, 1984 to 2022.
Abbreviation: HIV=human immunodeficiency virus; AIDS=acquired immunodeficiency syndrome.The evolution, distribution, and conceptual transformation of HIV/AIDS prevention and control policies in China, when analyzed in conjunction with the findings of previous scholars (6–9), suggest that the development of these policies can be segmented into four distinct phases: (1) intense monitoring to prevent the introduction of HIV/AIDS (1984–1988), (2) enhanced public awareness and proactive prevention measures (1989–1998), (3) a government-led, comprehensive approach to prevention and control (1999–2005), (4) the adoption and reinforcement of scientifically-informed prevention strategies (since 2006). Reflecting upon these stages, changes in the frequency of keywords associated with HIV/AIDS prevention and control policies are presented in Table 2. For clarity, Table 2 lists only the top ten keywords for each phase, excluding common stop-words as filtered by NVivo12 software, as well as terms lacking substantive relevance, such as possessive pronouns (e.g., yours, mine, his).
Words stages 1984–1988 1989–1998 1999–2005 since 2006 1 HIV/AIDS* HIV/AIDS* HIV/AIDS* HIV/AIDS* 2 Monitor Quarantine Prevention Prevention and treatment 3 Blood Prevention Prevention and treatment Testing 4 Inspection Publicity Education Prevention 5 Import Testing Testing Treatment 6
Sexually transmitted diseaseEducation Publicity Education 7 Management Sexually transmitted disease Control Publicity 8 Prevention Prevention and treatment Treatment Service 9 Dissemination Monitor Management Dissemination 10 Education Dissemination Dissemination Health Abbreviation: HIV=human immunodeficiency virus; AIDS=acquired immunodeficiency syndrome; KAP=knowledge-attitude-practice.
* Because of Chinese vocabulary usage habits, AIDS and HIV were combined into HIV/AIDS, as the same reason, Prevention and treatment was viewed as a word.Table 2. The high-frequency words change of HIV/AIDS prevention and control policies in China.
-
To delineate the evolution of the HIV/AIDS prevention and control policy landscape, our research team conducted a statistical analysis of the departments responsible for issuing policy documents, adjusting for any obfuscations due to renamings, mergers, or dissolutions of the issuing bodies. Utilizing specified inclusion and exclusion criteria, we identified 163 national-level policy documents on HIV/AIDS prevention and control. Among these, 39 (approximately 23.93%) documents were collaboratively issued by multiple government departments in China.
The former Ministry of Health of China (66, 40.49%), the China’s State Council (25, 15.34%), the China’s Ministry of Education (20, 12.27%), the China’s Ministry of Finance (15, 9.20%), and the China’s National Health and Family Planning Commission (10, 6.13%). The departments that jointly issued policies include the former Ministry of Health of China (16 times), the China’s Ministry of Finance (13 times), the China’s Ministry of Education (10 times), the China’s State Taxation Administration (8 times), the China’s National Health and Family Planning Commission (5 times), the China’s Ministry of Justice (4 times), the China’s Ministry of Civil Affairs (4 times) and the China’s Ministry of Public Security (4 times), etc. The China’s State Council, the constituent ministries and commissions of the China’s State Council and the organizations directly under the China’s State Council had issued policies with a wide time span and the largest proportion; the China’s Supreme People’s Procuratorate and the united social groups gradually issued policy texts on HIV/AIDS prevention and control after 2006 (Figure 4).
-
Table 3 displays the results of the analysis of policy types across different time periods. In the initial phase, guaranteed policies constituted the largest proportion at 41.46%, followed by KAP policies at 31.71%. Subsequent phases saw supportive policies gaining ground and eventually surpassing guaranteed policies in both the second and third stages. KAP policies maintained a significant presence from the second stage onward. Interestingly, in the fourth stage, guaranteed policies experienced a resurgence, accounting for 30.82% and exceeding supportive policies, which comprised 22.51%.
Year Type, % Guaranteed policies Support policies KAP policies Guiding policies 1984–1988 41.46 24.39 31.71 2.44 1989–1998 19.15 20.21 57.45 3.19 1999–2005 24.93 32.10 38.46 4.51 Since 2006 30.82 22.51 40.77 6.00 Abbreviation: HIV=human immunodeficiency virus; AIDS=acquired immunodeficiency syndrome. Table 3. Distribution of HIV/AIDS prevention and control policy types in China.
-
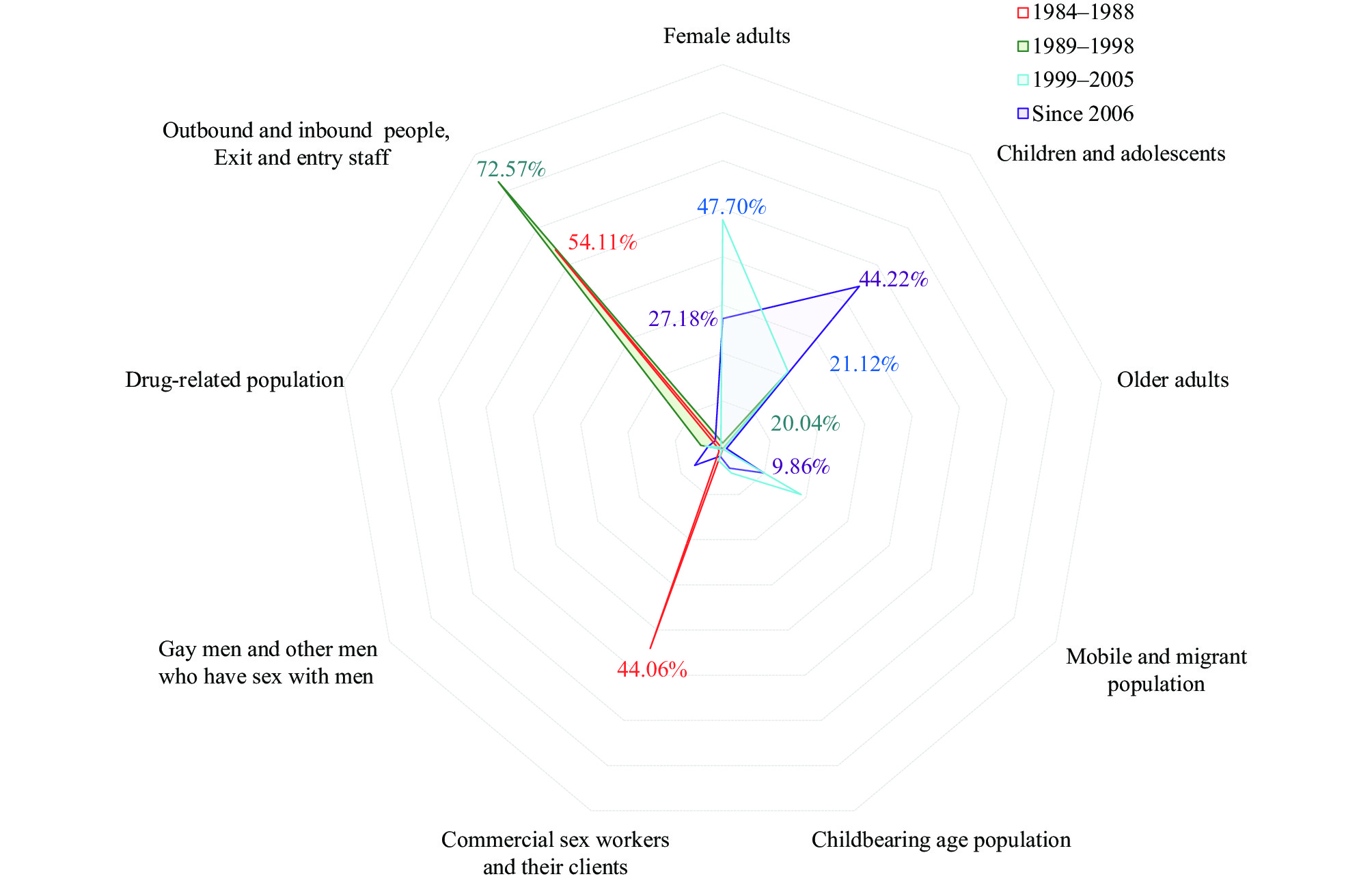
The categorization of population-related terms from the policy documents was systematically conducted, initially identifying 31 open codes, then consolidating into 11 axial codes, and ultimately crystallizing into 9 selective codes. These definitive codes formed the framework for delineating policy target populations within this study (Figure 5). We statistically assessed the frequency at which these policy target populations appeared at each phase, yielding insights into their prominence and implications. In the initial phase, commercial sex workers and their clients (44.06%), along with transnational travelers and border control personnel (54.11%), were identified as the primary focus groups. During the subsequent phase, the emphasis shifted to children and adolescents (20.04%) and remained on transnational travelers and border control personnel (72.57%). However, there appeared to be a need for heightened vigilance concerning the mobile and migrant populations, individuals of childbearing age, and older adults in forthcoming analyses. The third phase honed in on female adults (47.70%) and children and adolescents (21.12%), ensuring comprehensive population coverage. Currently, the spotlight is shared among children and adolescents (44.22%), female adults (27.18%), and the mobile and migrant population (9.86%).
-
Our research introduces a sun-shaped network model that offers a nuanced analysis of China’s HIV/AIDS prevention and control policies. The paramount goal of these policies is to safeguard public health. Effective prevention and control can only be achieved when the public not only possesses accurate knowledge but also embraces a robust sense of responsibility, allowing beliefs to take shape. It is the transition from mere knowledge to deeply held belief that underpins the public’s willingness to adopt positive behavioral changes.
The KAP approach is of particular significance, as it equips individuals with the necessary understanding of HIV/AIDS prevention and control measures. It also fosters constructive beliefs and attitudes toward these measures, culminating in the adoption of healthy behaviors that enhance overall well-being. Given its direct influence on health behaviors and its distinctive nature compared to other policy types, the KAP approach constitutes the core of our proposed model.
Supporting and guaranteeing policies serve to bolster the KAP approach, with the former providing direct reinforcement and the latter having an indirect impact on its implementation and outcomes. Furthermore, the guiding policies exert a direct influence on the other three policy categories, shaping their overall direction and effectiveness.
The NVivo12 software identified high-frequency terms that are fundamentally aligned with policy categories synthesized by grounded theory throughout the evolution of HIV/AIDS prevention and control policies. In the initial stage, terms such as “monitor,” “blood,” and “import” likely represent stringent measures implemented in China to regulate imported blood products, aiming to thwart the proliferation of HIV/AIDS. This phase saw a predominance of policies focused on safeguards (encompassing core themes such as monitoring, detection, and supervision), reflecting their central role in the policy landscape at the time. In the subsequent phase, words like “quarantine,” “prevention,” “publicity,” “testing,” and “education” suggest a shift in response to the widespread nature of the epidemic. With blood transmission, sexual contact, and intravenous drug use emerging as the primary transmission routes, the expansion of testing and quarantine efforts was evident. There was a notable shift towards proactive prevention strategies during this time, intensifying education and public awareness campaigns. This emphasis is mirrored in the KAP policies, which were the predominant policy category in this era. The third stage saw “prevention” and “education” maintaining high frequency, with “prevention and treatment” gaining prominence. Notably, the term “control” surged from the eighth to the second position. This change in frequency might relate to the rapid surge in HIV/AIDS cases during this period and the influence of the 2003 SARS outbreak. It reflected the Chinese government’s heightened recognition of the critical need to preemptively handle public health crises, with a concerted effort to prevent and manage HIV/AIDS encompassing various facets. KAP, support, and safeguard policies were more evenly distributed, indicating a broader and more integrated policy approach. In the final stage analyzed, the emergence of “service” and “health” among the top ten high-frequency terms suggests an evolution towards scientifically grounded HIV/AIDS prevention and control strategies, with an emphasis on advisory services and overall population health. The prominence of the term “health” might signify the incorporation of Health-first and Health in All Policies (HiAP) concepts in HIV/AIDS policy development. Throughout this period, KAP continued to occupy the largest share of policies, underscoring their importance in boosting health literacy and endorsing healthy living standards.
The development and transformation of HIV/AIDS prevention and control policies in China have shown alignment with practical applications, temporal relevance, and adherence to the policy directives issued by General Secretary Xi Jinping, emphasizing the shift from disease-centric treatment to a broader focus on public health. To a noteworthy degree, the persistence, modification, and cessation of HIV/AIDS prevention and control measures in China have been influenced by the trajectory of societal advancement. However, they are predominantly dictated by the tangible demands and exigencies of HIV/AIDS prevention and control efforts.
-
During this period, there was a widespread perception that the contemporary, liberal lifestyle of the West was frequently linked with the proliferation of HIV/AIDS, prompting calls for measures to prevent the introduction of the disease into China. As China’s trade in imports and exports flourished, and as interactions with foreign nationals, cutting-edge technologies, and the intermingling of Chinese and Western cultures increased (particularly during the initial and exploratory phase of the economic reform and opening-up from 1978 to 1991), these factors may have contributed to the aforementioned belief. At that time, societal focus was predominantly on economic policy matters, resulting in HIV/AIDS prevention and control strategies that centered on rejecting or halting the importation of foreign blood products. For example, the Joint Notice on Restricting the Import of Blood Products to Prevent the Spread of HIV/AIDS into China in 1984. This was followed by the 1985 Prohibition on the importation of blood products, such as Factor VIII, which barred the entry of foreign blood products into the country. By 1986, HIV/AIDS was classified as a Class B infectious disease, with new infections required to be reported within 24 hours.
-
During this period, the policy framework for HIV/AIDS prevention and control underwent significant changes. In 1989, HIV/AIDS was classified as a Class B infectious disease in accordance with the Law of the People’s Republic of China on Prevention and Treatment of Infectious Diseases, mandating that HIV/AIDS patients receive isolated treatment. This marked the elevation of HIV/AIDS prevention and control efforts to a legal standing. That same year, the first domestically transmitted case of HIV/AIDS was documented in China. Furthermore, the clustering of HIV/AIDS cases among injection drug users was identified in Ruili, Yunnan Province (10). In response to the escalating HIV/AIDS epidemic, the Chinese government intensified law enforcement and initiated a series of punitive actions targeting drug abuse and prostitution beginning in 1991. By 1995, the spread of HIV/AIDS, fueled by illicit and unregulated blood collection and supply activities in Henan, Hubei, Anhui, and other provinces, had become a serious concern (11). It was becoming clear that HIV/AIDS was spreading not only through international sources but also internally within the mainland. Evidently, the existing HIV/AIDS prevention and control policies, which were centered on surveillance, were not sufficiently effective. Acknowledging the gravity of the HIV/AIDS epidemic and the critical need for efficacious policy interventions, the Chinese central government implemented a spectrum of policy measures. The Blood Donation Law, enacted in 1998, emphasized voluntary over compensated blood donations to ensure the safety of blood for clinical use and the welfare of both donors and recipients. Additionally, the China National Medium and Long-Term Plan for HIV/AIDS Prevention and Control (1998–2010) promoted condom use to prevent the sexual transmission of HIV/AIDS. Concurrent with the ongoing reforms and the opening-up policy, public attitudes became increasingly receptive to Western ideas, fostering a blend of Chinese and Western cultural elements. There was a noticeable enhancement in public understanding of HIV/AIDS, leading to a shift toward active and preventative approaches in the prevention and control policies, which in turn facilitated more progressive and open prevention and control initiatives.
-
The HIV/AIDS epidemic transitioned into a more expansive phase in China following Stage II, with cases reported across diverse populations. As such, singular population-focused prevention and control policies proved insufficient. Demonstrating strong political will and responsibility, the Chinese government implemented a series of comprehensive HIV/AIDS policies. For example, Working duty in HIV/AIDS prevention and control for related ministries, committees, administrations and social groups released in 2000 was the first time to explicitly raise the issue of medical security for people infected with HIV/AIDS. The China’s action plan for reducing and preventing the spread of HIV/AIDS (2001–2005) launched the first Five-Year Action Plan which had considered harm-reduction measures such as methadone maintenance treatment (MMT), needle and syringe exchange and promotion of condom use. In 2003, the progressive “Four Free and One Care” policy was introduced in selected areas, offering free antiretroviral drugs to people living with HIV/AIDS. This initiative was instrumental in curbing the epidemic’s spread and reducing patient mortality. The period’s social security advancements, emerging from the establishment of the socialist market economy (1992–2002), provided a solid foundation for the era’s policymaking. The severe acute respiratory syndrome (SARS) outbreak in 2003 was a pivotal event for Chinese public health governance. This crisis underscored the efficacy of a government-led approach, embracing extensive community participation and multisectoral collaboration as the optimal strategy for resolving public health challenges. Consequently, an approach designed to foster widespread awareness and active engagement in HIV/AIDS prevention and control became progressively formulated and effectively executed. Over time, the nature of prevention and control efforts evolved towards proactive prevention, intervention, and legitimization. Significantly, official pilot programs for HIV/AIDS prevention and control demonstration zones targeting high-risk groups commenced, marking a notable advancement in the nation’s response to the HIV/AIDS epidemic.
-
During the era of socialist market economic development from 2003 to 2011, China experienced a continued strengthening of its economic prowess and an enhancement of its social security system. The government underwent a paradigm shift, opting to procure social services, and acknowledged the necessity of engaging all societal sectors, including non-governmental organizations (NGOs), to achieve mutual benefits in the realm of HIV/AIDS prevention and control. Furthermore, the Chinese government recognized the significant societal impact of HIV/AIDS and placed an elevated emphasis on the health of its citizens. This marked a new phase where government-led initiatives encouraged full public participation and saw the implementation of large-scale, targeted HIV/AIDS prevention and control policies. These policies became more comprehensive, structured, and compassionate. In 2006, the Regulations on AIDS Prevention and Treatment were enacted by the State Council of China, formalizing the “Four Free and One Care” policy. This policy not only protected the legal rights of individuals living with HIV and their families but also fortified important HIV/AIDS prevention and control efforts through legal and regulatory measures. It sanctioned behavioral interventions like condom promotion and substitution therapy for drug users, and it established a firm stance against discrimination. This regulation also provided a formal legislative endorsement for the provision of free antiretroviral treatment for individuals with HIV/AIDS. Wu Zunyou, the lead expert in epidemiology from the Chinese Center for Disease Control and Prevention, remarked that the “Four Free and One Care” policy was a cornerstone for HIV/AIDS prevention and control efforts in China. It not only reinforced these efforts, but it also indicated a significant shift in the government’s approach — from denial and inaction to proactive involvement and advocacy, setting an example at the global level (12). Proceeding with the proactive stance on HIV/AIDS countermeasures, the “China’s Action Plan on HIV/AIDS Prevention and Containment (2006–2010)” unrolled the second Five-Year Action Plan. This initiative built upon existing efforts by developing more targeted strategies and objectives. In 2008, the Ministry of Health released a directive to pilot an integrated HIV prevention and treatment program specifically for men who have sex with men, representing the most comprehensive policy to date addressing China’s HIV epidemic among this demographic address the HIV/AIDS epidemic among men in China. The policy named Five Expands and Six Strengths were proposed in 2010 to address the problems encountered by the Four Free and One Care policy, particularly in health education, HIV testing, and prevention and care services, ensuring a multifaceted approach to the ongoing health crisis.
In the context of comprehensive reform initiatives commenced in 2012, the Chinese government has implemented a robust reform agenda epitomized by an integrative five-sphere plan encompassing economic, political, cultural, social, and environmental domains. The government remains committed to sustaining and enhancing public welfare, bolstering prevention and control authorities, increasing funding, and refining supervision and evaluation mechanisms. Notably, China’s 12th Five-Year Action Plan for reducing and preventing the spread of HIV/AIDS (2011–2015) clarified the concept and measuring method of new infections of HIV/AIDS, expanding the coverage of HIV testing and surveillance, and maximizing the detection of HIV/AIDS cases. It also first proposed the principle of Knowing Situation but Not Refusing — When HIV testing agencies explicitly informed citizens that they would be provided with HIV testing services, the citizen who did not refuse was deemed to agree to undergo testing. Similarly, the 13th Five-Year Action Plan for HIV/AIDS control (2016–2020) aimed to raise awareness of HIV/AIDS prevention and treatment among the populace, extend the reach of testing and surveillance activities, and ensure comprehensive follow-up and execution of treatment and rescue measures. Furthermore, the Action Plan to Eliminate Mother-to-Child Transmission of HIV/AIDS, Syphilis, and Hepatitis B (2022–2025) sets objectives for the strengthened prevention of vertical transmission of these infections, with the primary goal of achieving national eradication of mother-to-child transmission. Central to the realization of these strategies was the aspiration to maintain the HIV/AIDS epidemic in China at low levels. The evolution of HIV/AIDS policies and their consequent implementation reflect an increased level of comprehensiveness, diversity, specificity, and institutionalization within the public health infrastructure of China (6,13–17).
Over the past four decades, China has made considerable progress in HIV/AIDS prevention and control efforts, paralleling the nation’s socioeconomic development. Evidence-based scientific advancements have been pivotal in informing policy development and execution. The approach to HIV/AIDS prevention and control has matured into a forward-thinking, proactive model that emphasizes cooperation among social communities (18). China’s government authorities have taken an active role in coordinating with various stakeholders to draft, disseminate, implement, and evolve policy measures. Social communities, recognized for their deep community engagement, adaptive approaches, and innovative problem-solving, have established a synergistic relationship with governmental and professional entities, fostering an environment of mutual support, complementarity, and shared benefits (19-20). In 1995, China initiated sentinel surveillance specifically targeting key populations at risk for HIV/AIDS. Presently, prevention and control initiatives encompass the entire lifespan, from infants to the elderly. As of 2022, there have been 10.7 million reported cases of HIV/AIDS, with 48.1% occurring in individuals aged 50 and above (21). Despite this, the term “older adults” remains underrepresented in the discourse. Analysis reveals that, over the last ten years, the prevalence of HIV/AIDS in the over-60 demographic has been increasing, with nearly half of these older adults diagnosed at an advanced stage of the infection (16,21). Several factors contribute to this trend. Common societal perceptions suggest that older adults are less likely to engage in sexual activity or substance abuse, thereby masking their risk profile. Furthermore, older adults face numerous barriers to obtaining sexual health information and to the early detection of HIV/AIDS (21-22). Policy initiatives concerning HIV/AIDS prevention and control have traditionally overlooked this age group, leading to a general lack of awareness and safety among older adults in the context of sexual health. Additionally, life circumstances such as widowhood and isolation may drive an increase in commercial sex-seeking behaviors among this population (22–24). With the acceleration of China’s aging process and the demographic shift toward a younger-elderly populace, it is crucial to develop and implement tailored HIV/AIDS health education and promotion strategies for older adults (25-26). This demographic now constitutes over half of the senior population, prompting an urgent need for appropriate intervention models to address this growing challenge.
In conclusion, this study employed a mixed-methods approach to objectively evaluate HIV/AIDS prevention and control policies in China, integrating both qualitative and quantitative assessments. By scrutinizing policy documents and the impacts of policy enactment, as well as other multifaceted metrics, the study devised an innovative sun-shaped network model for HIV/AIDS policy management. Advanced tools such as NVivo12 software and the principles of grounded theory facilitated a thorough three-tiered coding analysis of national-level HIV/AIDS policies. This methodology stands apart from previous studies that centered on chronological investigation, offering benefits in terms of comprehensiveness, currency, and analytical precision. Moreover, the study affirmed the suitability and practicality of applying grounded theory to the textual analysis of these policies within the Chinese context. Despite these strengths, some limitations were noted. Consequently, future research endeavors will integrate interviews, semi-structured interviews, and additional evaluative techniques to thoroughly appraise aspects of policy design, issuance, impact, funding, and program development. The objective is to underpin the formulation of HIV/AIDS policies with robust scientific evidence and articulate strategic recommendations to enhance their effectiveness in China.
HTML
Data Sources and Collection
Policy Analysis Method
HIV/AIDS Prevention and Control Policy Network Model
Time Distribution of Policy Issuance
Distribution and Development of Policy Subjects
Distribution and Development of Policy Types
Distribution and Development of Policy Objects
Stage I: Strictly Monitor and Prevent Introduction of HIV/AIDS (1984–1988)
Stage II: Strengthen Publicity, Education and Active Prevention and Control of HIV/AIDS (1989–1998)
Stage III: Government-led and Comprehensive Prevention and Control of HIV/AIDS (1999–2005)
Stage IV: Enhancing the Implementation of Evidence-Based HIV/AIDS Prevention and Control Strategies (Since 2006)
| Citation: |




 Download:
Download: