-
China has experienced rapid shifts in its population structure, which have notably influenced the prevalence rate of various diseases, including both infectious diseases and chronic conditions (1). The implementation of China’s policy of free antiretroviral therapy (HAART) for Acquired Immune Deficiency Syndrome (AIDS) patients in 2004 has substantially lengthened the survival timeline of those affected, transforming AIDS from a deadly infectious disease to a manageable chronic condition (2-3). Therefore, significant changes have been observed in the epidemiological characteristics and mortality rate trends of AIDS. Our study investigates the trends in HIV/AIDS case reported rate, mortality rate, and prevalence rate in an attempt to understand the evolving epidemiological patterns and overarching changes in HIV/AIDS across China’s entire population. This investigation provides valuable insights that could inform and enhance HIV/AIDS prevention and control strategies.
The data for this study was from the “China Comprehensive HIV/AIDS Prevention and Control Data Information System” downloaded on June 30, 2023, which included a historical database of HIV-infected individuals/AIDS patients reported before 2022 (infectious disease report cards). It also utilized historical population data from the China Disease Prevention and Control Information System, covering the years 2004 to 2021, which includes nationwide population data categorized by sex and age groups (year), as well as regional code data for different years and counties.
This study applied a multi cross-sectional analytical design, stratified by sex, age groups (year), and geographical regions (Eastern, Central, and Western regions). Annual reported rate, mortality rate, and prevalence rate related to reported HIV/AIDS cases were calculated. The reported rate (RR) was computed by dividing the number of reports in a given year by the population for that year, then multiplying it by 100,000, using the date of onset. Mortality rate for reported cases (MR) was determined using the date of all-cause death, calculated similarly to RR. The prevalence rate of reported cases (PR) was calculated using the combined total of surviving individuals at the start of the year, newly reported cases in that year, and subtracting annual reported deaths, all divided by the population for that year and multiplied by 100,000. The rates were age-standardized (ASR) based on the “2010 China Age-Standardized Population” for the above-mentioned crude rates (CR), consequently yielding SRR, SMR, and SPR. Classification of regions was determined using the “National Regional Code Table” (2023), dividing China into three regions: eastern provincial-level administrative divisions (PLADs) (Beijing, Tianjin, Hebei, Liaoning, Shanghai, Jiangsu, Zhejiang, Fujian, Shandong, Guangdong, Hainan), central PLADs (Shanxi, Inner Mongolia, Jilin, Heilongjiang, Anhui, Jiangxi, Henan, Hubei, Hunan), and western PLADs (Sichuan, Guizhou, Yunnan, Xizang, Shaanxi, Guangxi, Gansu, Ningxia, Qinghai, Xinjiang). The calculation of age (year) at onset (or death) required dividing the difference between the date of onset (or death) and the date of birth by 365.25. All data analysis was performed using SAS software (version 9.4, NC, USA).
This study found that at the national level in China, the reported rate and mortality rate of HIV/AIDS have shown a long-term slow upward trend, but they started to decline in 2018. However, it was observed that the prevalence rate in the population has continued to slowly increase (Figure 1).
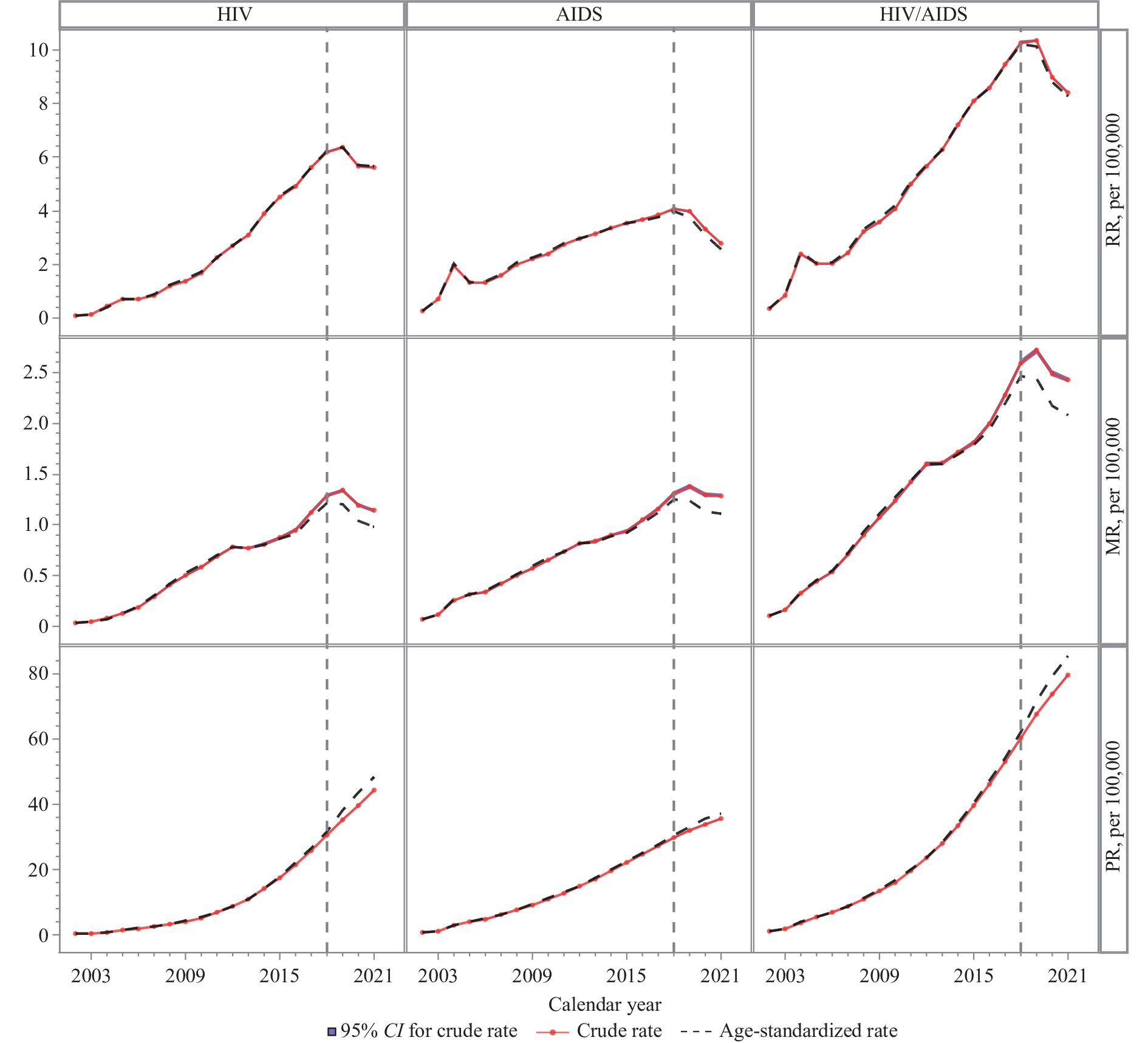 Figure 1.
Figure 1.The trends of reported rate, mortality rate, and prevalence rate of reported HIV/AIDS cases in China, 2002–2021.
Abbreviation: RR=reported rate; MR=mortality rate; PR=prevalence rate; CI=confidence interval.Nationally, the reported rate of HIV/AIDS escalated from 0.37 per 100,000 population in 2002 to 10.27 per 100,000 in 2018 [95% confidence interval (CI): 10.22–10.32], before receding to 8.41 per 100,000 in 2021 (95% CI: 8.36–8.46). A parallel trend was observed in the standardized reported rate of HIV/AIDS. HIV/AIDS associated mortality rate grew from 0.11 per 100,000 in 2002 to 2.59 per 100,000 in 2018 (95% CI: 2.40–2.45), subsequently decreasing to 2.43 per 100,000 in 2021 (95% CI: 2.40–2.45). The standardized mortality rate fell from 2.46 per 100,000 in 2018 to 2.08 per 100,000 in 2021. The prevalence rate of reported HIV/AIDS cases rose from 1.09 per 100,000 in 2002 to 60.21 per 100,000 in 2018, and further to 79.62 per 100,000 in 2021 (95% CI: 79.47–79.77). The standardized prevalence rate of reported HIV/AIDS cases increased from 62.02 per 100,000 in 2018 to 85.36 per 100,000 in 2021.
The reported rates of AIDS cases saw an increase from 0.26 per 100,000 population in 2002 to peak at 4.06 per 100,000 population in 2018, followed by a decline to 2.78 per 100,000 population in 2021. The standardized reported rate of AIDS showed a reduction from 3.99 per 100,000 population in 2018 to 2.58 per 100,000 population in 2021. The mortality rate of reported cases saw a rise from 0.07 per 100,000 population in 2002 to 1.31 per 100,000 population in 2018, which then slightly decreased to 1.28 per 100,000 population in 2021 (95% CI: 1.27–1.31). The adjusted mortality rate showed a decrease from 1.25 per 100,000 population in 2018 to 1.11 per 100,000 population in 2021. The prevalence rate of reported cases increased from 0.64 per 100,000 population in 2002 to 29.66 per 100,000 population in 2018 and further to 35.46 per 100,000 population in 2021 (95% CI: 35.36–35.56). The standardized prevalence rate increased from 30.51 per 100,000 population in 2018 to 37.01 per 100,000 population in 2021.
The standardized reported rate of HIV saw an elevation from 0.10 per 100,000 in 2002 to 6.21 per 100,000 in 2018, before undergoing a subsequent decrease to 5.67 per 100,000 in 2021. The standardized mortality rate of these reported HIV cases experienced a similar growth, increasing from 0.13 per 100,000 in 2002 to 1.22 per 100,000 in 2018, followed by a drop to 0.98 per 100,000 in 2021. The standardized prevalence rate of HIV reported cases mounted from 0.43 per 100,000 in 2002, reaching 31.51 per 100,000 in 2018, and escalating further to 48.34 per 100,000 in 2021.
Sex-specific analysis indicates that peak values for reported rate, mortality rate, and prevalence rate of HIV/AIDS cases in males are 4.0, 3.5, and 2.86 times higher, respectively, compared to females (Figure 2A). Age-specific data demonstrate peak reported rates for HIV/AIDS cases in the following age groups: 0–14 years (0.71/100,000), 15–29 years (9.80/100,000), 30–44 years (12.73/100,000), 45–59 years (13.00/100,000), 60–74 years (15.90/100,000), and ≥75 years (8.41/100,000) respectively (Figure 2B). Region-specific analysis indicates similar reported rate, mortality rate, and prevalence rate of reported HIV/AIDS cases in the eastern and central regions. However, in the western region, peak values are, respectively, 3.56, 4.74, and 3.05 times higher than those reported in the central region (Figure 2C).
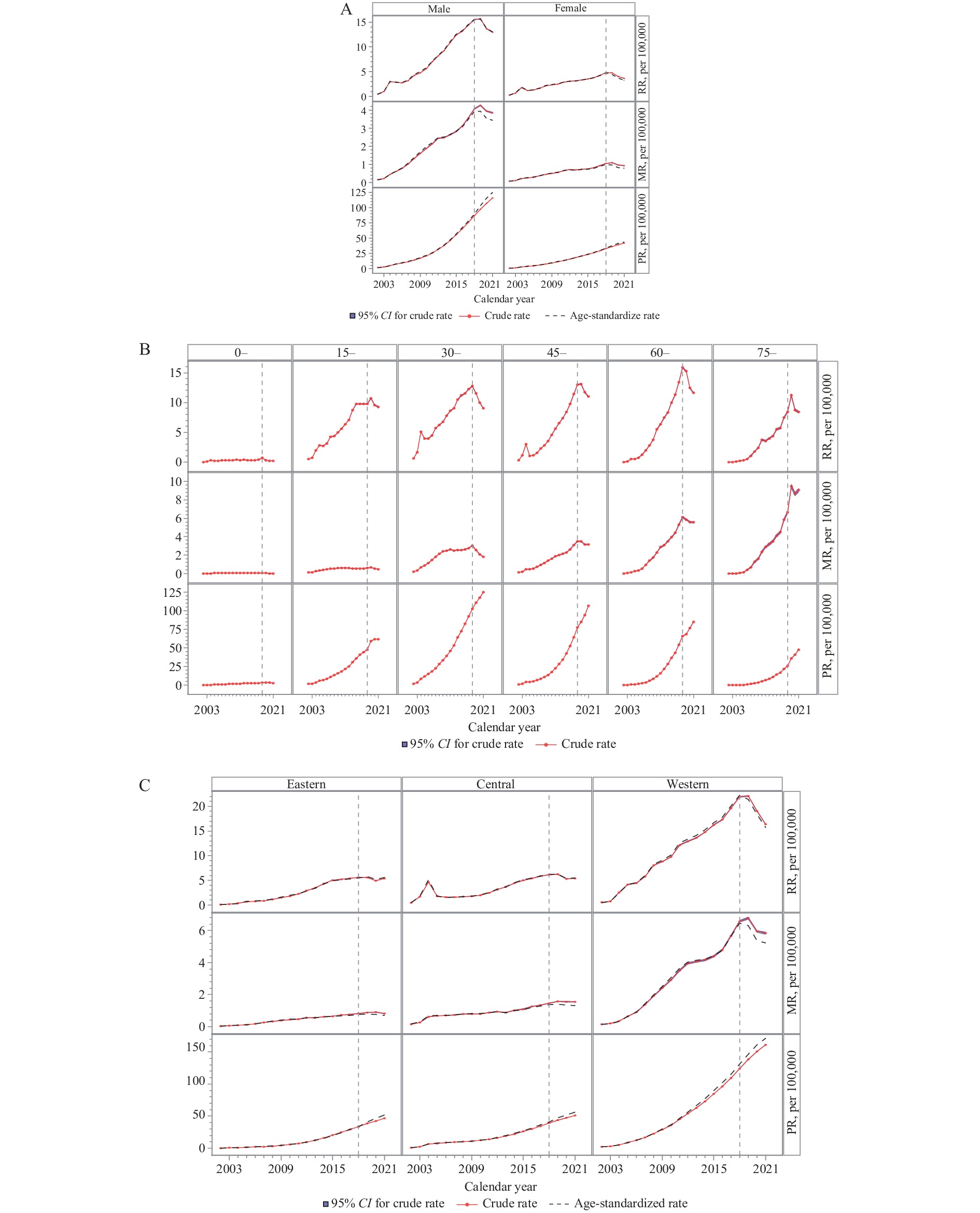 Figure 2.
Figure 2.The trends of reported rate, mortality rate, and prevalence rate of reported HIV/AIDS cases in China, by (A) sex, (B) age groups (year), and (C) region, 2002–2021.
Abbreviation: RR=reported rate; MR=mortality rate; PR=prevalence rate; CI=confidence interval.Our study reveals that at a national scale in China, there was a measured, consistent escalation in the reported rate, mortality rate, and prevalence rate of reported HIV/AIDS cases through 2018. Following this period, these trends partially inverted, indicating a decline in reported rate and mortality rate, which may be due to the effects of China’s comprehensive HIV/AIDS prevention and control strategy and its overlapping impact of pandemic control efforts. Yet, the prevalence rate within the population maintained a slow upward trajectory. Two primary factors are likely contributors to the consistent escalation trends before 2018 as follows:
First, sustained efforts by the Chinese government in preventing, controlling, and actively treating HIV/AIDS have expanded the scope of HIV screening among the population, thereby contributing to an annual increase in the reported rate for HIV/AIDS cases, with HIV reported cases being the predominant contributor (4). Second, significant advancements in the therapeutic landscape for HIV/AIDS played a key role. The extensive application of the “Four Frees and One Care” policy initiated in 2004 proved to be a pivotal juncture in China’s preventative and treatment initiatives for HIV/AIDS. Recently, over 90% treatment coverage has been achieved for HIV/AIDS patients in China, along with a treatment success rate surpassing 90% (4–5). The mortality rate among individuals receiving antiretroviral therapy for HIV/AIDS has now declined to less than 4 per 100 person-years (6), resulting in a marked enhanced life expectancy for patients. This extended life expectancy has led to a sustained accumulation of reported living HIV/AIDS cases, which in turn, drives the steadily ascending rate of prevalence. Collectively, these findings underscore the significant progress China has made in the prevention and control of HIV/AIDS.
Our findings indicate notable differences in the reported rate, mortality rate, and prevalence rate of reported HIV/AIDS cases across sex, age (year), and geographical regions. Males demonstrated a higher rate, mortality rate, and prevalence rate of reported HIV/AIDS cases than females. This difference may be attributed to variations in sex disparities in the mode of HIV/AIDS transmission (such as male-to-male transmission being predominant). Furthermore, the reported rate of HIV/AIDS varies with age, with a higher reported rate among older individuals, potentially because older individuals have more opportunities for HIV screening, and there is a greater accumulation of infected individuals in the elderly population.
Additionally, there is a significantly lower reported rate of HIV/AIDS in the central and eastern regions of China compared to its western regions. This could be attributed to the western regions of China (e.g., Yunnan, Sichuan, and Xinjiang) serving as the focal points of the HIV/AIDS epidemic. In the western areas, the HIV/AIDS outbreak initially stemmed from intravenous drug use as the primary mode of transmission, with heterosexual transmission being predominant, which stood in contrast to the primary transmission routes in the eastern areas. And these disparities may contribute to the comparatively elevated reported rate, mortality rate, and prevalence rate of reported HIV/AIDS cases in the western regions.
Our manuscript is subject to several limitations. First, our analyses are largely dependent on case-reported data, which chiefly represents reported cases of HIV/AIDS, as opposed to actual case numbers. Further investigation into this aspect is required. Second, this research adopts a descriptive study approach, omitting inferential analyses concerning trend alterations, tipping points, or contributing factors related to HIV/AIDS.
To summarize, data from China indicates a steady, the incremental increase in the reported rate, mortality rate, and prevalence rate of reported HIV/AIDS cases through 2018. Subsequent reversal trends suggest a decline, yet the cumulative prevalence rate among the population continued its slow incline. These increasing trends can be largely accredited to the relentless efforts made by the Chinese government in HIV prevention, control and effective treatment strategies. These efforts, coupled with a significant reduction in AIDS-related mortality rate and marked improvements in patient life expectancy, play a pivotal role in the continued rise in the number of people living with HIV/AIDS. The findings of our research could provide valuable insights to support the future monitoring and prevention efforts for HIV/AIDS.
HTML
| Citation: |



 Download:
Download:




