-
Pneumoconiosis, an interstitial lung disease induced by dust exposure, represents a significant and prevalent occupational health hazard in China (1). Often, individuals with pneumoconiosis have experienced prolonged exposure to mineral dust, thus significantly impairing their respiratory system’s clearance and defense mechanisms. The chronic and progressive nature of pneumoconiosis remarkably compromises the patient’s immunity. Furthermore, pneumoconiosis patients frequently exhibit a range of comorbidities or complications, including pulmonary tuberculosis (PTB), non-tuberculosis (non-TB) lung infection, pneumothorax, chronic obstructive pulmonary disease (COPD), and chronic pulmonary heart disease. Patients are typically approaching 60 years of age, and the majority are middle-aged to elderly individuals. These patients might also endure additional chronic diseases, such as hypertension and diabetes, alongside pneumoconiosis. The concurrent manifestation of two or more of these aforementioned diseases or conditions within the same individual constitutes multimorbidity (2). Given the aging population and advancements in medical technology, the occurrence of multimorbidity is increasing. Consequently, managing individuals with multiple chronic diseases has emerged as a global challenge for societal and healthcare systems (3).
While some studies have examined the comorbidities associated with pneumoconiosis in specific locales or industries, a comprehensive, large-scale assessment of multimorbidity in pneumoconiosis patients throughout China is yet to be conducted. To address this gap, we performed a cross-sectional survey between December 2017 and June 2021 to understand the patient health statuses and the utilization of medical services by pneumoconiosis patients across 27 provincial-level administrative divisions (PLADs) in Chinese mainland — survey not including Tianjin Municipality, Shanghai Municipality, Hainan Province, and Xizang (Tibet) Autonomous Region.
Our survey employed a face-to-face questionnaire, administered by trained physicians and nurses specializing in occupational diseases. We collected a total of 11,181 valid responses and included 10,137 qualified pneumoconiosis patients in our analysis, amounting to 90.7% of all respondents. The respective annual breakdown of our analytical sample consisted of 953 (9.4%) in 2017, 2,077 (20.5%) in 2018, 3,529 (34.8%) in 2019, 3,084 (30.4%) in 2020, and 494 (4.9%) in 2021.
Using the survey data, we analyzed the distribution of the prevalence of 13 common comorbidities or conditions in pneumoconiosis patients. We stratified these distributions by gender, urban or rural residence, stage of pneumoconiosis, and smoking index. Furthermore, we calculated the prevalence rates, along with their 95% confidence intervals (CIs) for multimorbidity in various age groups, categorizing these by gender, residence, stages of pneumoconiosis, and smoking index. We also explored the patterns of multimorbidity stratified by urban and rural areas. These findings aim to inform the development of effective treatment strategies and health security policies for pneumoconiosis in China.
The questionnaire considered for this study assesses eleven self-reported chronic diseases. Participants were asked, “Have you been diagnosed with any of the following diseases or conditions during treatment or examination at hospitals or outpatient clinics: PTB, lung cancer or mesothelioma, diabetes, hypertension, pulmonary heart disease, cardiovascular diseases (CVDs), cerebrovascular diseases, non-TB lung infection, COPD, pulmonary bullae or pneumothorax, and rheumatism?” The remaining two conditions were determined from the participants’ body mass index (BMI), which included obesity (BMI≥24.0 kg/m2) and underweight (BMI<18.5 kg/m2). For the purposes of statistical analysis, age was categorized as follows: ≤44 years, 45–59 years, and ≥60 years. The smoking index was calculated by multiplying the number of cigarettes smoked daily by the years of smoking. Multimorbidity (MM1+) was defined as a patient having one or more of these 13 diseases or conditions within one pneumoconiosis patient population.
Data conforming to a normal distribution was articulated as mean±standard deviation (SD), while categorical data was represented by numbers (percentages). This study scrutinized the statistical significance of disparities using one-way analysis of variance (ANOVA) or t-tests for continuous variables of normal data distribution, assuming equal variances. For continuous variables exhibiting normal or nearly normal distribution, Pearson correlation analysis was utilized. For categorical data, Chi-square analysis and Fisher’s exact test were deployed. Linear-by-Linear Association (LLA) test was applied to calculate P-values for trends concerning proportions and prevalence. All statistical tests were two-sided, with P<0.05 indicating statistical significance. SPSS software (version 26.0, SPSS Inc., Chicago, IL, USA) was used to conduct all the aforementioned statistical analysis. Further information about the survey design, sample, subject background, questionnaire approaches, and data processes is outlined in a previous publication (4). This paper reports on the prevalence of 13 diseases or conditions in the subjects, with 11 being primarily self-reported by patients based on diagnostic results.
Ethical approval for this research was granted by the Ethics Committee of the National Institute for Occupational Health and Poison Control, associated with the Chinese Center for Disease Control and Prevention (Approval No. 201720). Written informed consent was obtained from all participants.
Of the 10,137 participants in the study, 97.4% were men (n=9,875) with an average age of 57.6 years (SD=11.5). This was notably younger than the female participants, who had an average age of 68.1 years (SD=13.7; F=211.067, P<0.001). Patients in urban locations were older than those in rural areas (F=969.257, P<0.001), and the age of participants decreased correspondingly with the stage of pneumoconiosis (F=159.243, P<0.001). Approximately 39.7% of the participants (n=4,021) were aged 60 years or older. Comparatively, the group aged 60 and above had a higher proportion of females than males (70.2% vs. 38.9%; χ2=104.970, P<0.001). It also had a higher proportion of urban rather than rural participants (53.3% vs. 29.1%; χ2=611.700, P<0.001). Significant statistical differences were observed in the proportions of middle-aged and elderly patients according to their varying clinical stages of pneumoconiosis and those without a stage (47.5% vs. 39.5% vs. 30.6% vs. 22.9%; χ2=303.048, P<0.001).
The prevalence rates for patients with one to six or more comorbidities were 28.8% (2,924/10,137), 15.9% (1,612/10,137), 10.6% (1,074/10,137), 5.9% (599/10,137), 2.9% (291/10,137), and 1.9% (189/10,137), respectively. Of these patients, 66.0% (95% CI: 65.1–66.9) had at least one comorbidity, and 37.1% (95% CI: 36.2–38.1) had two or more comorbid actions. Higher prevalence rates were found in male patients, urban residents, and patients with a smoking index of 200 or higher, with an increased rate coinciding with the severity of pneumoconiosis. Table 1 details the distribution of incidence and prevalence for 13 diseases or conditions, divided by gender, residential area, pneumoconiosis stage, and smoking index.
Diseases and conditions Total
(n=10,137)Sex P Residence P Stages of pneumoconiosis P Smoking index P Male
(n=9,875)Female
(n=262)Rural
(n=5,713)Urban
(n=4,424)Stage Ⅰ (n=4,540) Stage Ⅱ (n=2,518) Stage Ⅲ (n=2,134) No stage
(n=945)<200
(n=5,903)≥200
(n=4,234)PTB and Respiratory system disease PTB 762 (7.5) 748 (7.6) 14 (5.3) 0.176 513 (9.0) 249 (5.6) <0.001 175 (3.9) 193 (7.7) 269 (12.6) 125 (13.2) <0.001 365 (6.2) 397 (9.4) <0.001 Non-PTB lung infection 2,298 (22.7) 2,234 (22.6) 64 (24.4) 0.491 1,144 (20.0) 1,154 (26.1) <0.001 955 (21.0) 554 (22.0) 579 (27.1) 210 (22.2) <0.001 1,345 (22.8) 953 (22.5) 0.743 COPD 2,431 (24.0) 2,349 (23.8) 82 (31.3) 0.005 1,127 (19.7) 1,304 (29.5) <0.001 977 (21.5) 642 (25.5) 630 (29.5) 182 (19.3) <0.001 1,249 (21.2) 1,182 (27.9) <0.001 Lung bulla or emphysema 979 (9.7) 974 (9.9) 5 (1.9) <0.001 690 (12.1) 289 (6.5) <0.001 187 (4.1) 199 (7.9) 467 (21.9) 126 (13.3) <0.001 517 (8.8) 462 (10.9) <0.001 Lung cancer or mesohyloma 41 (0.4) 40 (0.4) 1 (0.4) 0.714 15 (0.3) 26 (0.6) 0.011 25 (0.6) 7 (0.3) 8 (0.4) 1 (0.1) 0.136 25 (0.4) 16 (0.4) 0.721 Endocrine, nutritional and metabolic diseases Obesity 769 (7.6) 738 (7.5) 31 (11.8) 0.009 325 (5.7) 444 (10.0) <0.001 415 (9.1) 219 (8.7) 96 (4.5) 39 (4.1) <0.001 403 (6.8) 366 (8.6) 0.001 Malnutrition 757 (7.5) 735 (7.4) 22 (8.4) 0.562 549 (9.6) 208 (4.7) <0.001 160 (3.5) 143 (5.7) 352 (16.5) 102 (10.8) <0.001 422 (7.1) 335 (7.9) 0.149 Diabetes 652 (6.4) 620 (6.3) 32 (12.2) <0.001 230 (4.0) 422 (9.5) <0.001 390 (8.6) 153 (6.1) 89 (4.2) 20 (2.1) <0.001 359 (6.1) 293 (6.9) 0.090 Circulatory system diseases Hypertension 2,034 (20.1) 1,934 (19.6) 100 (38.2) <0.001 861 (15.1) 1,173 (26.5) <0.001 1,109 (24.4) 531 (21.1) 290 (13.6) 104 (11.0) <0.001 1,125 (19.1) 909 (21.5) 0.003 Pulmonary heart disease 1,177 (11.6) 1,129 (11.4) 48 (18.3) 0.001 493 (8.6) 684 (15.5) <0.001 520 (11.5) 287 (11.4) 291 (13.6) 79 (8.4) <0.001 684 (11.6) 493 (11.6) 0.930 CVDs 1,127 (11.1) 1,044 (10.6) 83 (31.7) <0.001 339 (5.9) 788 (17.8) <0.001 637 (14.0) 322 (12.8) 134 (6.3) 34 (3.6) <0.001 656 (11.1) 471 (11.1) 0.986 Cerebrovascular disease 502 (5.0) 479 (4.9) 23 (8.8) 0.004 168 (2.9) 334 (7.5) <0.001 277 (6.1) 153 (6.1) 48 (2.2) 24 (2.5) <0.001 255 (4.3) 247 (5.8) 0.001 Rheumatism 916 (9.0) 901 (9.1) 15 (5.7) 0.058 664 (11.6) 252 (5.7) <0.001 370 (8.1) 246 (9.8) 194 (9.1) 106 (11.2) 0.009 470 (8.0) 446 (10.5) <0.001 Age 57.9±11.7 57.6±11.5 68.1±13.7 <0.001 54.8±9.9 61.8±12.6 <0.001 60.2±12.0 57.8±12.1 55.3±10.0 52.8±9.7 <0.001 57.4±12.1 58.6±11.0 <0.001 Abbreviation: PTB=pulmonary tuberculosis; CVDs=cardiovascular diseases; COPD=chronic obstructive pulmonary disease. Table 1. Incidence and prevalence (%) of 13 types of diseases or conditions associated with pneumoconiosis categorized by sex, place of residence, clinical stage, and smoking index in China, 2018–2021.
Table 1 reveals that respiratory and circulatory system diseases were the most common comorbidities. Women had higher prevalence rates of circulatory system diseases, COPD, obesity, and diabetes, while men had higher rates of pulmonary bullae or pneumothorax and arthritis. Urban patients had a higher prevalence of circulatory system diseases, pulmonary infection, COPD, obesity, and diabetes, whereas rural patients had higher rates of PTB, underweight, pulmonary bullae or pneumothorax, and arthritis. Stage I patients showed higher rates for obesity, diabetes, hypertension, CVDs, and cerebrovascular diseases, while stage III patients had higher rates for PTB, underweight, pulmonary bullae or pneumothorax, and other respiratory diseases. Individuals with a smoking index of ≥200 had higher rates of PTB, obesity, hypertension, cerebrovascular disease, COPD, pulmonary bullae or pneumothorax, and arthritis.
A positive correlation was found between the number of comorbidities and age (r=0.328, P<0.001). An increase in the prevalence of MM1+ with age was observed, landing at 54.3% (95% CI: 51.2–57.4), 58.4% (95% CI: 57.0–59.7), and 78.6% (95% CI: 77.3–79.8) for age groups ≤44 years, 45–59 years, and ≥60 years, respectively (χ2=419.135, P<0.001). Age-stratified analysis according to gender, locality, pneumoconiosis stage, and smoking index consistently demonstrated an increased prevalence with ascending age. MM1+ prevalence rates were notably elevated among female patients, urban dwellers, those in stage III of pneumoconiosis, and those with a smoking index of ≥200, as outlined in Table 2.
Characteristics N ≥1 Chronic conditions, % (95% CI) ≤44 years (n=1,002) 45−59 years (n=5,114) ≥60 years (n=4,021) Total (n=10,137) Total 10,137 54.3 (51.2−57.4) 58.4 (57.0−59.7) 78.6 (77.3−79.8) 66.0 (65.1−66.9) Gender Male 9,875 54.5 (51.4−57.0) 58.4 (57.0−59.7) 78.0 (76.7−79.3) 65.6 (64.7−66.6) Female 262 38.5 (12.0−64.9) 58.5 (46.5−70.4) 89.7 (85.3−94.1) 79.4 (74.5−84.3) P for difference 0.275 0.990 <0.0001 <0.0001 Residence Rural 5,713 56.9 (53.3−60.5) 57.3 (55.7−59.0) 73.2 (71.1−75.4) 61.9 (60.7−63.2) Urban 4,424 47.9 (42.2−53.7) 60.3 (58.1−62.6) 82.3 (80.8−83.9) 71.2 (69.9−72.6) P for difference 0.010 0.038 <0.0001 <0.0001 Stages of pneumoconiosis Stage Ⅰ 4,540 45.0 (39.5−50.5) 53.4 (51.2−55.5) 79.2 (77.5−80.9) 65.1 (63.7−66.5) Stage Ⅱ 2,518 52.6 (46.6−58.5) 56.6 (53.8−59.3) 79.0 (76.5−81.5) 65.0 (63.1−66.9) Stage Ⅲ 2,134 73.9 (68.2−79.6) 67.9 (65.3−70.5) 75.5 (72.2−78.8) 70.9 (68.9−72.8) No stage 945 48.4 (41.1−55.6) 59.6 (55.5−63.7) 79.6 (74.3−85.0) 62.0 (58.9−65.1) P for difference <0.0001 <0.0001 0.213 <0.0001 Smoking index <200 5,903 50.1 (46.4−53.9) 56.8 (55.0−58.6) 79.1 (77.4−80.8) 64.5 (63.2−65.7) ≥200 4,234 63.8 (58.4−69.2) 60.6 (58.5−62.7) 77.9 (76.0−79.8) 68.1 (66.7−69.5) P for difference <0.0001 0.006 0.354 <0.0001 Note: Pneumoconiosis considered with multimorbidity refers to patients who have been diagnosed by a healthcare professional with one or more of the following 13 types of diseases or conditions: pulmonary tuberculosis, lung cancer or mesohyloma, diabetes, hypertension, pulmonary heart disease, cardiovascular diseases, cerebrovascular diseases, non-TB lung infection, chronic obstructive pulmonary disease, pulmonary bullae or pneumothorax, and rheumatism.
Abbreviation: CI=confidence interval.Table 2. Prevalence of multimorbidity in 10,137 pneumoconiosis patients in China, 2018–2021 (%).
Further analysis revealed a higher proportion of urban and female patients aged 60 years and older. In urban areas, retired workers from state-owned enterprises were significantly more numerous than in rural regions (80.9% vs. 21.4%, χ2=3581.828, P<0.001). Similarly, the proportion of work-injury-insured workers was distinctly higher in urban areas versus rural (86.2% vs. 29.8%, χ2=3197.974, P<0.001). The proportion of retired female employees from state-owned enterprises surpassed that of males (62.2% vs. 47.0%, χ2=49.267, P<0.001), and more female patients were covered by work-related injury insurance than male patients (69.5% vs. 54.0%, χ2=24.688, P<0.001). This can potentially be attributed to the higher incidence of multimorbidity amongst urban patients and females.
In this study, 72.5% of patients working in state-owned enterprises benefitted from work-related injury insurance while only 35.2% and 26.8% did so in collective and private enterprises, respectively (χ2=366.263, P<0.001).
Figure 1 illustrates the patterns of multimorbidity, represented by various pairwise combinations of diseases or conditions, in both rural and urban settings. The most prominent combinations include four specific diseases: non-TB pulmonary infection, pulmonary heart disease, pulmonary bullae, pneumothorax, and hypertension. These were frequently observed in patients with pneumoconiosis from both urban and rural regions, albeit at higher proportions in urban patients. Moreover, the comorbidity of underweight and arthritis paired with non-TB lung infection and pulmonary heart disease were notably higher in rural patients. On the other hand, pairings of diabetes, cerebrovascular disease, obesity with hypertension, CVDs, COPD, and pulmonary infection were more commonly seen in urban patients, establishing several unique aggregate distributions.
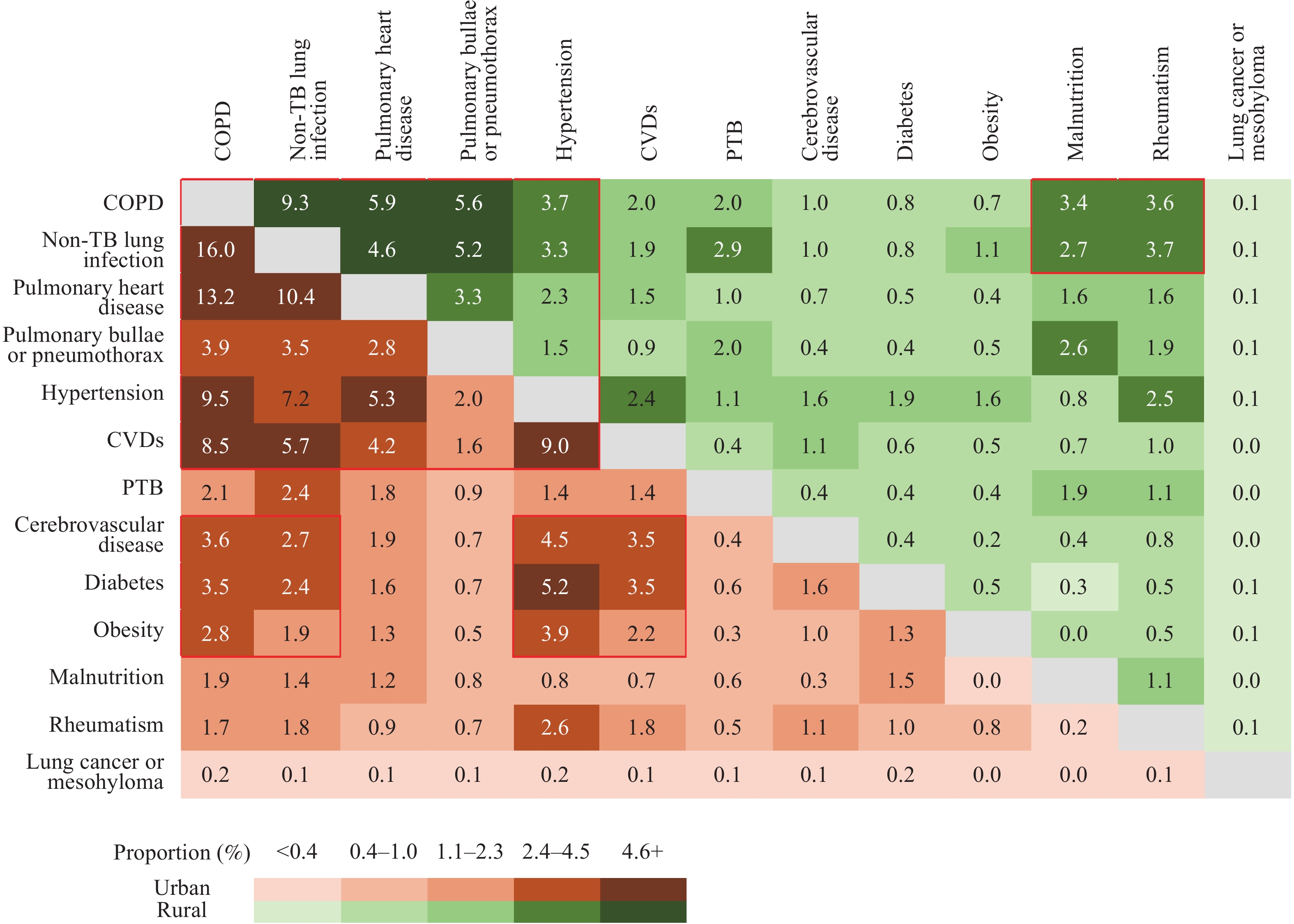 Figure 1.
Figure 1.Heatmap of the percentage of comorbid disease pairs and conditions by residence among pneumoconiosis patients in China.
Note: The proportions depicted by the green diagonal situated above and to the right of the gray diagonal represent patients residing in rural areas. Conversely, the proportions indicated by the brown diagonal below and to the left of the gray diagonal represent patients hailing from urban areas.
Abbreviation: COPD=chronic obstructive pulmonary disease; CVDs=cardiovascular diseases; PTB=pulmonary tuberculosis.
-
Comorbidities and complications significantly influence the treatment, progression, and prognosis of pneumoconiosis, primarily contributing to patients’ deterioration and mortality. An accurate and timely diagnosis and treatment of such comorbidities and complications is crucial to enhancing patient survival rates, their health status, life expectancy, and quality of life. As suggested by the China Expert Consensus on the Treatment of Pneumoconiosis (2018 edition), there is a need to reinforce comprehensive health management and actively carry out symptomatic treatment, management of comorbidities and complications, as well as rehabilitation treatment. Research into pneumoconiosis comorbidities outside the respiratory system has been minimal. The focus of this study is primarily on common comorbidities or complications of pneumoconiosis. This includes not only respiratory illnesses but also circulatory diseases, disorders of the immune and nutritional systems, metabolic diseases, and skeletal conditions. These collectively provide an insight into the distribution of multimorbidity in pneumoconiosis.
A study evaluating data from 126 investigations comprising approximately 15.4 million individuals across 54 countries revealed that multimorbidity prevalence heightens with an increased volume of diseases assessed. When assessing multimorbidity over 10 to 19 conditions, prevalence was disclosed to be 41.3% (5). However, in China, multimorbidity prevalence manifested a considerable degree of variation among elderly individuals, displaying a range from a mere few percent up to 80% (6). In the context of the present study, multimorbidity prevalence within pneumoconiosis patients was identified as being 66.0%, a rate that surpasses the previously mentioned rates.
Research has demonstrated a notable rise in the occurrence of lower respiratory tract infections among coal workers’ pneumoconiosis (CWP) patients co-diagnosed with COPD and tuberculosis. This rise is more prominent in patients in stages II and III compared to those in stage I (7). Consistent with these findings, our study also identified a higher prevalence of pulmonary heart diseases, hypertension and CVDs associated with COPD and lung infections, particularly in urban populations compared to their rural counterparts. Moreover, the occurrence of cerebrovascular diseases, diabetes, and obesity was elevated among urban patients, along with complications such as COPD and non-TB lung infections. Considering the profound correlation between diseases, such as obesity, hypertension, diabetes, and cerebrovascular disorders, and lifestyle factors, it is crucial to intensify health promotion efforts aimed at dust-exposed workers and pneumoconiosis patients.
Patients with pneumoconiosis often experience severe illness or recurrent lung infections, which can lead to malnutrition and consequently impair the body’s defense and immune functions. Repeated infections can exacerbate the disease. Rural pneumoconiosis patients tend to show a higher prevalence of underweight and arthritis. Furthermore, the co-occurrence of non-TB lung infections or pulmonary heart disease is more commonly found among these individuals. Therefore, strengthening nutritional interventions for rural patients is imperative. Comprehensive nutritional support can boost immunity. With the help of financial assistance, patients should be encouraged to maintain a balanced diet and increase their consumption of high-quality protein-rich foods, such as eggs, milk, and lean meats, as well as a variety of other foodstuffs.
Pneumothorax is a prevalent complication of pneumoconiosis that affects the pleura. It primarily occurs during the second and third stages of pneumoconiosis, posing a significant life-threatening risk if it is not diagnosed and treated in a timely manner. Common triggers include a severe cough and expectoration exacerbated by respiratory infection. The study reported a higher prevalence of pulmonary bullae or pneumothorax in cases complicated with non-TB lung infection and pulmonary heart disease. This occurrence was particularly higher in rural participants than in their urban counterparts. Considering that most patients primarily rely on primary medical institutions for their healthcare needs (8), upskilling these institutions, especially in the rural areas, on appropriate diagnostic and treatment methods could be instrumental in controlling the condition. The study further showed that the rural patients with this condition were younger, and the elderly patient population was relatively less. This observation may result from premature deaths due to limited occupational injury insurance and inadequate medical services. It necessitates further investigation. The occupational injury insurance system serves as a fundamental health protection mechanism for patients with pneumoconiosis. However, its uptake among China’s migrant workers remains low. Therefore, effective measures should be adopted to facilitate the coverage of occupational injury insurance among this group. Furthermore, detailed medical security policies specifically tailored to address the different multimorbidity patterns of pneumoconiosis need to be developed and implemented.
The treatment and clinical decision-making process for multimorbidity pose significant health-related challenges to patients, medical professionals, and the broader society. Applying individual clinical practice guidelines in managing patients with multiple conditions might intensify treatment burden and potentially yield negative effects. Considering the inherent complexity, heterogeneity, and the myriad combinations of diseases in multimorbidity, existing guidelines recommend a personalized management approach (9-10).
In clinical settings, pneumoconiosis commonly presents as cough, expectoration, chest tightness, and asthma, with primary treatments consisting of antiasthmatics, expectorants, and antitussives. The frequent overuse of antibiotics and hormones, combined with aggressive diagnostic and therapy approaches, often results in complex multiple bacterial infections in patients with pneumoconiosis, thereby complicating the treatment process. It’s also important to consider that the majority of these patients are middle-aged and elderly individuals who may be experiencing various comorbid chronic diseases, a factor which further compounds the challenge of administering multiple medications. Due to these complexities, there is a pressing need to conduct evidence-based research on therapeutic drugs related to various comorbidities and to establish appropriate technical guidelines.
The current study is not without its limitations. Initially, the primary data for eleven types of diseases or conditions was principally acquired via self-reported questioning, leading to potential inaccuracies due to information bias. This could either underestimate or overestimate the actual figures. Additionally, several common chronic ailments, including but not limited to digestive and kidney diseases, urologic and lumbar issues, and neurological and mental health conditions, were not incorporated into this research. This exclusion was based on the potential inaccuracy of self-reports, which may consequently underestimate the prevalence of multimorbidity. Furthermore, the study’s representation of the complete pneumoconiosis patient population may be imperfect due to uneven participant distribution across China’s districts. Hence, caution should be exercised when interpreting the findings’ applicability to other patient groups. Moreover, the research is a preliminary cross-sectional analysis of pneumoconiosis multimorbidity and requires future in-depth exploration, given its intricate nature. Factors influencing pneumoconiosis multimorbidity, such as the type of pneumoconiosis, locale, education level, financial status, and physical activity levels, warrant additional analysis and investigation.
-
No conflicts of interest.
-
The authors extend their gratitude to the participants of the study and acknowledge the valuable contributions of the survey team members across all 27 regional centers, as well as the project development and management teams.
HTML
| Citation: |



 Download:
Download:




