-
Meningitis, a critical infection that impacts the meninges — protective membranes surrounding the brain and spinal cord — presents a significant public health challenge due to its life-threatening nature (1). Insights from the Global Burden of Disease (GBD) study exposed an increase of 320,000 worldwide meningitis cases between 1990 and 2016 (1). Given its extensive population, China ranks among the top 10 nations globally for meningitis-associated mortalities. Despite prior research investigating worldwide trends in meningitis mortality, there remains a paucity of understanding regarding national trends and the discrepancies between urban and rural areas. The current study dissected changing patterns in China’s meningitis mortality rate from 1987 to 2021 and spotlighted age-period-cohort effects influencing mortality changes. These revelations will equip the government with valuable insights into long-term trends and guide the development of targeted prevention strategies.
The mortality rates related to meningitis were extracted from the death registration system managed by the National Health Commission in China (2). This registry amalgamates several sources of data, including 1) death certificates and population demographics from the Department of Health, 2) changes in registered residences from the Department of Public Security, 3) cremation data from the Department of Civil Affairs, and 4) termination of social security information from the Department of Social Security. Age-standardized mortality rates (ASMR) were tabulated employing the direct method and the World Standard Population as a frame of reference (3). A joinpoint regression analysis was performed to detect fluctuations in meningitis mortality over time (4). Furthermore, an age-period-cohort model was used to ascertain the independent influence of age, period, and birth cohort on meningitis mortality rates in China (5). This research disclosed a steady decrease in meningitis mortality rates throughout urban and rural China over the past thirty years. Importantly, children, specifically those aged 0–4, present the highest risk of meningitis. These results effectively demonstrate the evolving trends of meningitis mortality and underscore the critical demographics for prevention strategies in China, offering valuable insights for future preventative measures against meningitis.
Figure 1 depicts the longitudinal trends in crude mortality rates and ASMR for meningitis among urban and rural populations in China, stratified by sex, from 1987–2021. Both crude mortality rates and ASMR saw a significant decrease from 1987 to 2002, and largely remained stable after 2002, despite some fluctuations observed between 2010 and 2013. Throughout the study period, higher ASMRs were typically seen in males and rural residents when compared to females and urban dwellers, respectively.
 Figure 1.
Figure 1.Trends in the crude and age-standardized mortality rates from meningitis in urban and rural areas of China, by sex, 1987–2021. (A) Crude mortality rates in urban areas. (B) Crude mortality rates in rural areas. (C) Age-standardized mortality rates in urban areas. (D) Age-standardized mortality rates in rural areas.
Table 1 details the results of the joinpoint regression analysis. The ASMR displayed a general decreasing trend in both urban and rural areas, although the substage trends were not consistent. The decline in urban ASMR was marginally steeper compared to the rural regions. In urban settings, ASMR experienced a rapid decrease from 1987–2003, followed by a gradual rebound from 2003–2016, and a stark decline again from 2016–2021. Conversely, in rural areas, ASMR showed a slow reduction from 1987–1999, a rapid decline from 1999–2002, and a flat rebound from 2002–2021. Notably, a slight disparity was observed between sexes in meningitis mortality in urban and rural areas.
Residence Mortality rate†
(per 100,000)Entire range§ Segment 1 Segment 2 Segment 3 1987 2021 AAPC (%) 95% CI Period APC (%) 95% CI Period APC (%) 95% CI Period APC (%) 95% CI Urban Total 0.53 0.07 −6.5* (−8.6, −4.3) 1987–2003 −10.0* (−11.8, −8.1) 2003–2016 1.9 (−1.4, 5.2) 2016–2021 −15.4* (−25.2, −4.4) Male 0.53 0.08 −6.3* (−8.8, −3.7) 1987–2003 −9.4* (−11.7, −7.0) 2003–2015 2.4 (−2.1, 7.2) 2015–2021 −14.3* (−23.5, −4.0) Female 0.53 0.05 −6.7* (−9.3, −4.1) 1987–2004 −10.5* (−12.4, −8.6) 2004–2017 2.5 (−1.2, 6.2) 2017–2021 −18.0* (−32.5, −0.5) Rural Total 0.52 0.09 −3.7* (−9.6, 2.6) 1987–1999 −2.9 (−6.9, 1.3) 1999–2002 −28.4 (−65.0, 46.4) 2002–2021 0.4 (−1.7, 2.6) Male 0.57 0.12 −3.3 (−9.5, 3.3) 1987–1999 −3.2 (−7.4, 1.2) 1999–2002 −32.1 (−68.0, 44.0) 2002–2021 2.2 (−0.1, 4.5) Female 0.48 0.07 −3.7* (−13.9, 7.7) 1987–2000 −3.0 (−9.3, 3.7) 2000–2003 −29.6 (−80.3, 151.4) 2003–2021 0.9 (−3.2, 5.1) Abbreviation: APC=annual percent change; AAPC=average annual percent change; CI=confidence interval.
* Significant difference from zero (P<0.05).
† Standardization employed is based on the world standard population from the World Health Organization.
§ The time frame considered ranges from 1987 to 2021.Table 1. Joinpoint analysis of age-standardized mortality rates due to meningitis in urban and rural areas.
Figure 2 illustrates the net and local drifts of mortality rates due to meningitis. The net drift indicates the yearly percentage fluctuation in the predicted age-standardized mortality, as the local drift signifies the similar change over time. This pattern was consistently seen in both urban and rural areas of China. Throughout the study period, there was a substantial reduction in mortality resulting from meningitis (urban: −5.22%, 95% CI: −5.66% to −4.78%; rural: −4.51%, 95% CI: −5.04% to −3.98%). However, slight variances were observed in the annual changes between both genders. The decline in overall meningitis mortality was noticeably sharper in females compared to males in both urban (−5.49% vs. −4.83%) and rural areas (−5.25% vs. −3.88%). Also, the local drift curves for rural and urban locales displayed a predominantly positive U-shape. The decline was steepest for the 20–29 age group and routinely decreased with age in the 0–19 and 20–89 age groups. The curves demonstrated relative consistency between urban and rural areas, with the exception of the advanced age group.
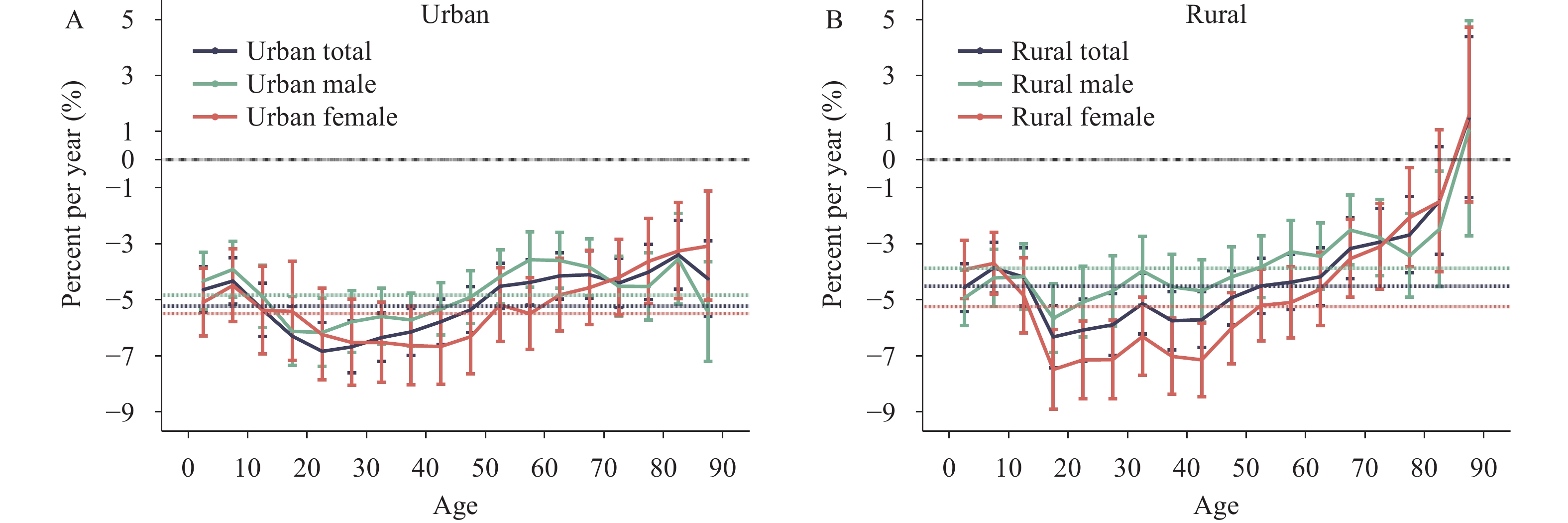 Figure 2.
Figure 2.Net and local changes in mortality rates from meningitis and the associated gender disparities observed across different regions in China, 1987–2021. (A) Net and local drifts in urban areas. (B) Net and local drifts in rural areas.
Figures 3, 4, and 5 delineate estimates of age, period, and cohort effects on the mortality rates due to meningitis. The impact of age on mortality remained consistent across both genders and geographical locations, viz., urban and rural regions. Mortality rates due to meningitis were observed to peak during the 0–4 age range, after which they noticeably plummeted in the 5–9 age range. Post this decrease, the rates were largely stable, maintaining a minimal level across the 10–89 age brackets. Period effects demonstrated a similar consistently diminishing trend from 1987 to 2006 before entering a period of stability post-2007, irrespective of gender and location. Despite this, variations were noted in the period effects of urban and rural mortality rates due to meningitis, with the disparity between genders being less pronounced in urban areas in comparison to rural areas. Furthermore, cohort rate ratios exhibited a similar downward trend across genders and geographical locations. For cohorts born post-1952, the mortality rates due to meningitis have maintained a uniformly low level.
 Figure 3.
Figure 3.Parameter estimates of the effect of age on mortality rates due to meningitis in China from 1987 to 2021. (A) Age effects in urban areas. (B) Age effects in rural areas.
-
The present investigation offers the first exhaustive review of longitudinal trends associated with meningitis mortality rates in China from 1987 to 2021, emphasizing the unique trends and age-period-cohort effects among rural and urban regions. The outcomes underscore a consistent decrease in the meningitis mortality rates within China, thus proving the efficacy of the preventive strategies related to meningitis implemented during the preceding three decades. Notable divergences were found among variables such as age, sex, and regional disparities in several patterns pertaining to meningitis mortality rates. Infants within the age bracket of 0–4 years are at the highest risk of acquiring meningitis. Negligible sex-based discrepancies were noted among age, period, and cohort effects associated with meningitis mortality, with the main rural-urban disparity being evident in the period effects. The identified high-risk groups necessitate immediate consideration and specialized preventative measures against meningitis.
Previous research has identified a variety of factors that contribute to meningitis, including infectious agents such as bacteria, mycobacteria, viruses, fungi, and parasites, as well as autoimmunity, cancer, and medicine reactions (1). Malnutrition, household overcrowding, HIV infection, lack of immunization, indoor air pollution, and sickle cell disease have been identified as risk factors that predispose individuals to meningitis and potential epidemics. In China, the decline in meningitis mortality rate surpasses the global average significantly (1). This decrease can be attributed to enhanced surveillance and diagnostic assessment, improved access to healthcare services, advancements in treatment and caregiving, and a reduction in individual treatment costs, particularly through the widespread administration of meningitis vaccinations for prevention (1,6–7). In 1984, China introduced a comprehensive prevention strategy primarily involving the widespread use of the group A meningococcal polysaccharide vaccine as a means to prevent epidemic cerebrospinal meningitis. This vaccination initiative was further expanded in 1985–1986, resulting in continued declines in incidence rates and the prevention of nationwide epidemics (6). In 2007, the national immunization program incorporated both the group A meningococcal polysaccharide vaccine and the group A and C meningococcal polysaccharide vaccine, with age-appropriate children receiving immunizations. Despite these advancements, China’s absolute number of meningitis deaths remains comparable to nations like Nigeria and Ethiopia situated in the meningitis belt — positioning it amongst the highest globally (1). As such, there is an ongoing need for the persistent implementation of comprehensive meningitis prevention strategies.
Age is a critical demographic factor in the prevalence of meningitis, with existing research emphasizing a heightened incidence of the disease during the neonatal stage and the most elevated mortality rates in children below five years of age (1,8). This is attributed primarily to two factors: one, infants and children’s immature immune system, which reduces their ability to battle infections, such as meningococcal and pneumococcal infections, which constitute significant causes of meningitis mortality (1). Second, the diagnosis of meningitis is particularly challenging in children and specifically, neonates (9). The symptoms of neonatal meningitis often mimic those encountered in neonates with sepsis or other infections, and their limited ability to verbally express their distress may lead to underreporting or a possible delay in the diagnosis. Vaccination has demonstrated effectiveness in preventing meningitis in infants (1,10). Thus, the creation and promotion of more specific vaccines are critical in the fight against this disease.
Previous research has illustrated high levels of meningitis in resource-limited environments due to a combination of factors inclining these regions to infection, epidemics, and poor health outcomes (1). The disparities between urban and rural areas were primarily observable in the overall reduction in meningitis mortality, the division of sub-stages, and variations in the effect of gender over time. The more rapid decline in urban regions can likely be credited to effective screening, diagnosis, and treatment of meningitis (1). The differing sub-stage trends we identified between rural and urban areas may be a result of China’s urbanization process, which has seen a significant migration of rural inhabitants into cities, further intensifying healthcare disparities. Overall, the differences between urban and rural effects on meningitis mortality, regarding age, period, and cohort, were slight in China. This could be indicative of a narrowing gap over the past 30 years in terms of meningitis screening, diagnosis, and vaccine distribution between the two types of regions. However, considerable uncertainty surrounds the causal factors and risks associated with meningitis. Based on the unique urban-rural dynamic in China, it was crucial to implement active disease-specific meningitis surveillance, promote meningitis vaccines, and continually enhance diagnosis and treatment strategies to reduce the nation’s meningitis mortality rate. Furthermore, gender disparities were apparent not only over time in urban and rural regions but also in the decreasing rates of meningitis mortality. Females exhibited a more rapid decline in mortality than males, potentially due to their higher propensity to seek medical attention and greater personal health standards, resulting in fewer infection opportunities and prompt care following infection. This gender gap seems to have grown more pronounced in rural regions in recent years, hence the observed gender disparities over time in urban and rural areas.
This study is subject to some limitations. First, the absence of detailed data on specific forms of meningitis, such as bacterial or viral meningitis, constrains the potential development of more targeted prevention strategies. Second, advances in the quality of meningitis mortality rate data might introduce a temporal bias into our analysis. Unfortunately, assessment reports on such improvements are absent, and noteworthy enhancements in data quality within extensive healthcare systems may require substantial time. As such, we presume that the mortality rate data utilized in this study holds consistent quality. Third, akin to other age-period-cohort analyses, a potential ecological fallacy could arise. Such a phenomenon implies that interpretations derived from population-level findings may not necessarily stand relevant at an individual level.
HTML
| Citation: |



 Download:
Download:






