-
Surveillance is a critical component of epidemiological and public health practice, playing a significant role in the prevention, control, and management of major public health risks (1). Historically, surveillance methods were primarily based on hospital data (e.g., sentinel hospital monitoring for influenza) or specific populations [such as the human immunodeficiency virus/acquired immunodeficiency syndrome (HIV/AIDS) population] for sentinel surveillance. However, for newly emerging infectious diseases or major infectious diseases with pandemic potential, traditional methods based on hospitals or specific populations may be insufficient for meeting the requirements of multi-source information, active monitoring, and early warning. For instance, the reported number of coronavirus disease 2019 (COVID-19) cases represents passive reporting data, as there is a certain proportion of asymptomatic infected individuals and those who have not been tested. As most countries have relaxed or eliminated COVID-19 testing strategies, the number of reported cases may not accurately or comprehensively reflect the global prevalence levels and dynamic trends of COVID-19 in the general population.
Following the early outbreak phase of COVID-19, China entered a normalization stage of prevention and control on April 29, 2020. During this stage, by adopting a strategy to prevent both imported cases and domestic resurgences, China effectively controlled the epidemic’s spread and significantly reduced the number of deaths. On December 7, 2022, China implemented the “Ten New Measures” to optimize COVID-19 prevention and control efforts further. Against this backdrop, China quickly and urgently established the nationwide Sentinel Community-Based Surveillance (SCS) by the end of 2022 (2), an innovative method for actively detecting infectious diseases, which aims to dynamically monitor the incidence rate of COVID-19 within the general population and provide an evidence-based foundation for estimating healthcare resource needs and allocating resources scientifically. SCS has played an essential, necessary, and irreplaceable role in actively tracking the COVID-19 epidemic situation and effectively managing public health risks in the general population in China. This study analyzes and describes the definition, characteristics of community-based surveillance, and practical experiences in China, providing a model reference for proactive surveillance in other countries or for other infectious diseases.
-
SCS represents a proactive approach to surveillance, involving the systematic and ongoing collection, analysis, and interpretation of data related to community populations. It is closely integrated with the prompt and consistent dissemination of results and evaluations to relevant stakeholders, thus enabling the initiation of appropriate actions (1).
-
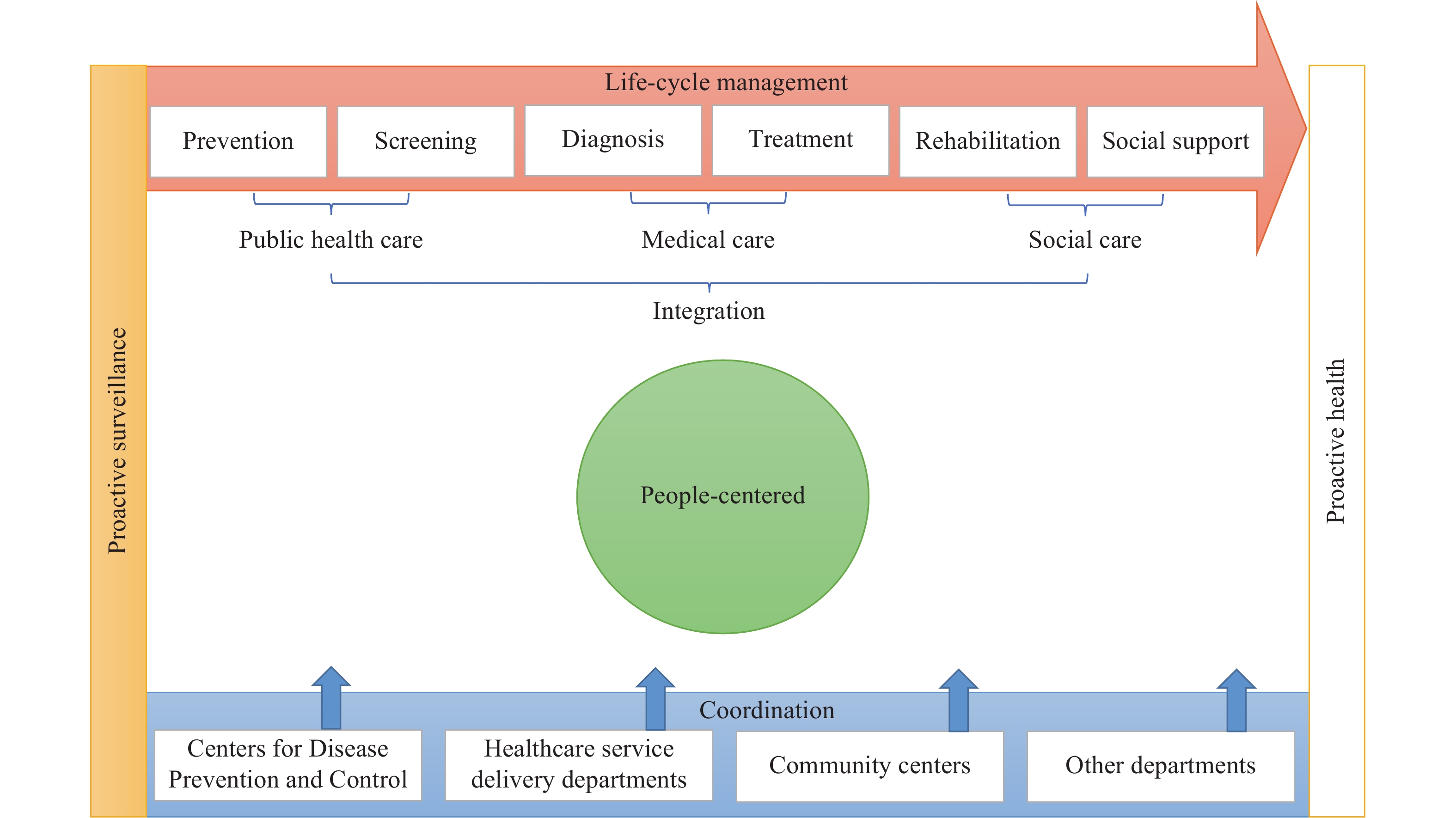
The SCS represents a significant departure from prior surveillance methods through four key advancements. First, the surveillance approach has shifted from passive to proactive, whereby the SCS actively acquires pertinent information regarding potential infectious diseases on a regular basis, drawing upon a national prospective community-based cohort. Second, the focus of surveillance has transitioned from confirmed or suspected patients (patient-centered) to the general population (people-centered). Traditional hospital-based surveillance typically collects data on patients with specific conditions such as influenza or HIV/AIDS, which, despite its relative ease, may not accurately represent the general population due to inherent selection bias. Third, the SCS now encompasses the comprehensive life-cycle management of infectious diseases, including aspects of prevention, screening, diagnosis, treatment, rehabilitation, and social support. Forth, the SCS merges public health, medical care, and social care in a cohesive fashion. The system garners support from a variety of organizations such as the CDCs, healthcare service delivery departments, community centers, and other related departments, ultimately bridging the gaps in fragmented public health and medical surveillance systems.
Consequently, we have distilled these transformations into five core attributes of the SCS model: proactive, people-centered, life-cycle management, integration, and coordination, collectively referred to as the “PELIC” theoretical framework (Figure 1).
-
In December 2022, the Omicron variant strain of severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2) rapidly spread in China (3). To dynamically monitor the epidemic trends and disease burden of COVID-19 in the general population and to promptly understand changes in public medical needs, the National Sentinel Community-Based Surveillance (NSCS) was launched under the support of the National Bureau of Disease Control and Prevention. This aimed to provide scientific evidence for improved prevention, control, and management of COVID-19 and enable the rational allocation of medical and health resources (2).
NSCS is a national community-based sentinel surveillance cohort consisting of a sample size of 0.42 million participants. It employed multistage stratified cluster sampling from all 31 provincial-level administrative divisions (PLADs) and the Xinjiang Production and Construction Corps (XPCC). Each PLAD selected one provincial capital city, one other large city, and one county. At least 2,000 households (≥5,000 individuals) were sampled in each provincial capital city; at least 1,500 households (≥3,000 individuals) were sampled in each selected large city; and at least 1,000 households (≥2,500 individuals) were sampled in each selected county (2). The minimum sampling unit was the household, and all selected households were included in the cohort. Each site conducted nucleic acid or antigen testing twice a week for every household. Additionally, information on symptoms, hospital visits, and other basic data were collected. NSCS collected data and provided feedback through multi-department collaboration. Community or village committees in each surveillance sentinel site were responsible for implementing the investigation and reporting data. The district CDC of each sentinel site was responsible for collecting information and reporting to other levels.
All participants in the monitored communities were tested for infection twice a week from December 16, 2022, to January 12, 2023. Data from the NSCS showed that the peak of SARS-CoV-2 infection in China had passed, and SARS-CoV-2 infection in community populations is currently at a low epidemic level (2). Specifically, the daily average newly positive rate of SARS-CoV-2 infection decreased from 4.13% in Round 1 (December 16–19, 2022) to 0.69% in Round 8 (January 10–12, 2023). The epidemic peak occurred in Round 2 (December 20–22, 2022) (2). In rural areas, the epidemic wave also peaked between December 20–22, 2022, and passed quickly following the optimization of prevention and control measures (4). Since January 13, participants have been tested once a week, given the low epidemic level of SARS-CoV-2 infection. The time interval and content of community-based surveillance have been adjusted and optimized according to the needs of disease prevention and control.
-
The practical experience in China has demonstrated that the SCS model plays a crucial, necessary, and irreplaceable role in actively monitoring the COVID-19 epidemic and effectively managing public health risks among the general population (2,4). The SCS model is particularly well-suited for situations where an infectious disease is in the community-transmission stage (or widely prevalent), or where asymptomatic infections and mild cases constitute a significant proportion of the infected population, and appropriate testing methods are available for screening. This approach enables stakeholders, such as the government, health sector policymakers, CDCs, health workers, communities, and the public, to timely and dynamically assess the incidence rate, cumulative infection rate, and estimate the demand for health resources among the general population. As an innovative method of proactive surveillance for emerging and widespread infectious diseases, the SCS model can also provide a useful reference for proactive surveillance in other countries and for other infectious diseases.
In 2021, China released the Outline of the 14th Five-Year Plan and the Vision 2035 of the National Economic and Social Development of the People’s Republic of China, which explicitly emphasized proactive health intervention technologies (5). As a means of achieving proactive health, proactive surveillance will play a critical role in preparing for and responding to future outbreaks of infectious diseases and other major infectious diseases. Community-based surveillance platforms can also serve a multidimensional role in proactive surveillance (such as symptom surveillance, disease surveillance, and surveillance of health resource demand), early warning, resource preparation and allocation, medical and social support, and community governance. This approach, based on community populations, enhances the preparation and response for future outbreaks of emerging infectious diseases and other significant infectious diseases.
-
No conflicts of interest.
HTML
| Citation: |



 Download:
Download:




