-
Chronic pain affects over 30% of people worldwide (1). It is often considered a precursor to cardiovascular diseases (CVDs) and a consequence of metabolic disorders. However, little is known about whether chronic pain increases the incidence of metabolic-related multimorbidity, including metabolic multimorbidity (MM) and cardiometabolic comorbidity (CMC), or whether adopting healthy lifestyles can mitigate these risks. We addressed these research gaps using the Cox proportional hazards regression and floating absolute risk in R statistical software (version 4.1.2, R Foundation for Statistical Computing, Vienna, Austria). Our results demonstrate that chronic pain is associated with a higher risk of developing new-onset diabetes, dyslipidemia, CVDs, MM, and CMC in middle-aged and older Chinese individuals. Furthermore, adopting healthy lifestyles can lower or even reverse the increased risk of these diseases attributed to chronic pain. Given the substantial burden of chronic pain, our study underscores the importance of adopting healthy lifestyles in preventing metabolic-related multimorbidity among older adults in China.
The present study utilized data from the China Health and Retirement Longitudinal Study (CHARLS) 2011–2018, a nationally representative survey that included participants aged 45 years and older residing in 450 villages and urban communities across China. A total of 17,708 participants were initially recruited at baseline in 2011, with subsequent follow-ups conducted in 2013, 2015, and 2018. To ensure data quality, participants were excluded based on the following criteria: age below 45 years, missing data on sex, residence, education, household income, and marital status at baseline (N=3,089); missing data on chronic pain, hypertension, diabetes, dyslipidemia, and CVDs at baseline (N=336); and missing data on smoking history, alcohol consumption, body mass index (BMI), waist-to-height ratio (WHtR), and sleep at baseline (N=3,175), ultimately resulting in a sample size of 11,108 participants for analysis (Figure 1).
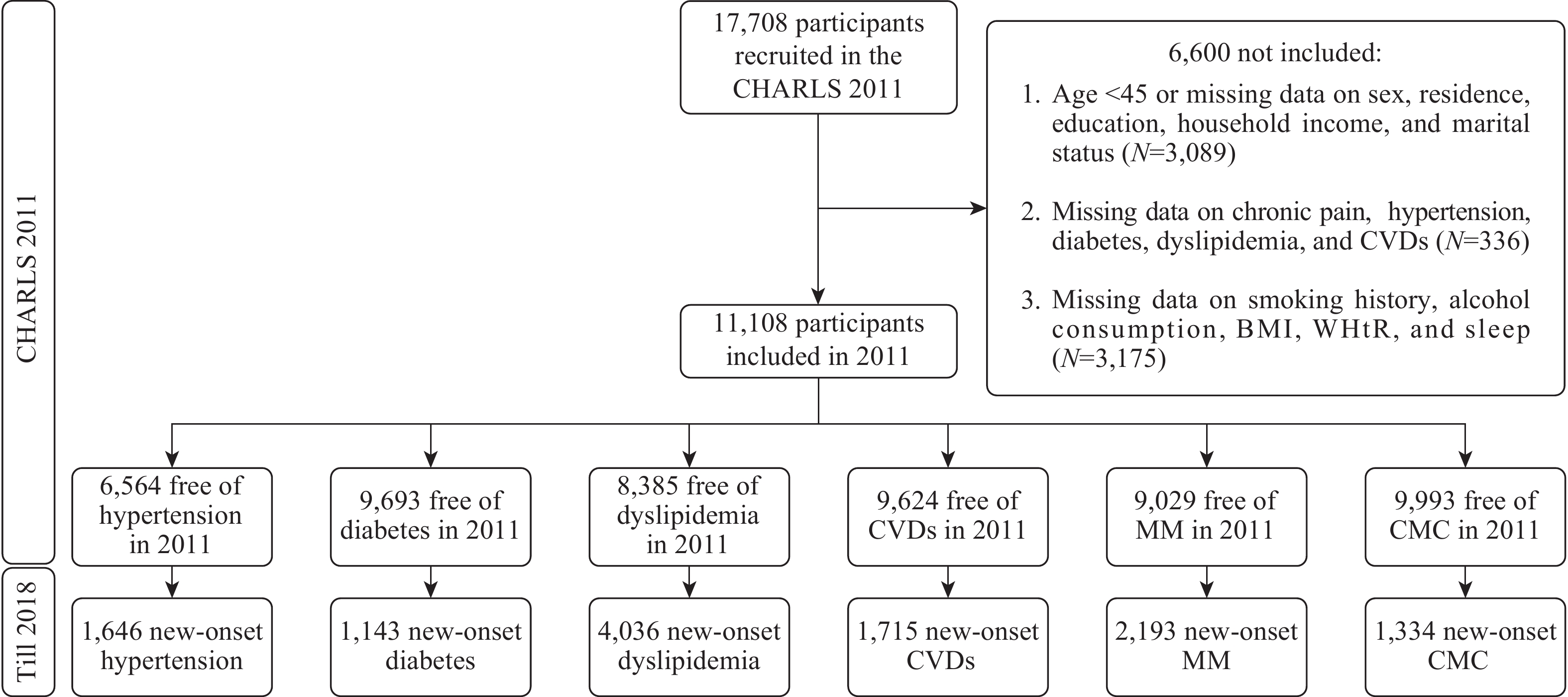 Figure 1.
Figure 1.Flow chart of participants included.
Abbreviation: CHARLS=China Health and Retirement Longitudinal Study, CVDs=cardiovascular diseases, BMI=body mass index, WHtR=waist-to-height ratio, MM=metabolic multimorbidity, CMC=cardiometabolic comorbidity.The study involved participants who self-reported pain in various body parts and were then categorized into three groups: 0 (no chronic pain), 1–3 (mild chronic pain), or 4 or more (severe chronic pain) body parts. Five healthy lifestyle factors were identified, namely, never smoking (with no smoking history), low alcohol intake (less than 14 drinks/week for men and 7 drinks/week for women, with a drink containing 13.6 g of ethanol or equivalent to 375 mL of beer or 118 mL of wine) (2), normal weight (BMI<24 kg/m2), absence of central obesity (WHtR<0.5), and optimal sleep (7–8 hours per night) (3). The participants were classified as least healthy, relatively healthy, and most healthy based on their 0–2, 3, and 4–5 healthy lifestyles. The study also defined cardiometabolic disorders (CMDs) such as hypertension, diabetes, dyslipidemia, and CVDs (heart disease and stroke) by using self-reported physicians’ diagnoses or treatments. For hypertension, a blood pressure of ≥140/90 mmHg was identified, while diabetes was identified if fasting plasma glucose ≥7.0 mmol/L or random plasma glucose ≥11.1 mmol/L or glycated hemoglobin ≥6.5%. Dyslipidemia was identified if total cholesterol ≥240 mg/dL, low-density lipoprotein cholesterol ≥160 mg/dL, high-density lipoprotein cholesterol ≤40 mg/dL, or if triglycerides ≥200 mg/dL. The presence of two or more of hypertension, diabetes, and dyslipidemia was defined as MM, and the presence of CVDs and one or more of hypertension, diabetes, and dyslipidemia was defined as CMC. Age, sex, residence (rural and urban), education level (primary school or less, middle school, and high school or above), household income (overall income divided into first, second, and third tertiles), and marital status (married/cohabiting and single) were considered as covariates.
This study examined the association between chronic pain severity and the onset of hypertension, diabetes, dyslipidemia, CVDs, MM, and CMC. All models were adjusted for age, sex, residence, education, household income, marital status, and healthy lifestyles. The study evaluated the associations of healthy lifestyles, compared to the least healthy, with these disorders in participants with no, mild, and severe chronic pain, while controlling for relevant confounding variables. We also investigated the effects of healthy lifestyles on the association between chronic pain severity and the above disorders, with “Mild chronic pain and least healthy lifestyles” as the reference category. All analyses were two-tailed and considered statistically significant at a P value of <0.05 and a 95% confidence interval (CI) for the hazard ratio (HR) that did not cross 1.00.
Table 1 displays the baseline characteristics of the participants included in our study. The analysis demonstrated that individuals with chronic pain of greater severity exhibit an increased risk for developing diabetes, CVDs, MM, and CMC (all P<0.05). Table 2 illustrates that compared to individuals without chronic pain, those who experienced severe chronic pain were associated with a higher risk of new-onset diabetes, dyslipidemia, CVDs, MM, and CMC. HRs (95% CIs) were 1.22 (1.06–1.40), 1.09 (1.01–1.18), 1.70 (1.53–1.90), 1.23 (1.11–1.37), and 1.64 (1.45–1.85), correspondingly.
Baseline characteristics Chronic pain severity, n (%) P value No (N=7,368) Mild (N=2,047) Severe (N=1,693) Age, years [Median (IQR)] 58.0 (51.0–65.0) 59.0 (53.0–66.0) 59.0 (53.0–65.0) <0.001 Sex <0.001 Men 3,866 (52.5) 908 (44.4) 574 (33.9) Women 3,502 (47.5) 1,139 (55.6) 1,119 (66.1) Residence <0.001 Rural 4,398 (59.7) 1,418 (69.3) 1,268 (74.9) Urban 2,970 (40.3) 629 (30.7) 425 (25.1) Education 3,866 (52.5) <0.001 Primary school or less 4,676 (63.5) 1,537 (75.1) 1,374 (81.2) Middle school 1,694 (23.0) 359 (17.5) 230 (13.6) High school or above 998 (13.5) 151 (7.4) 89 (5.2) Household income 0.041 First tertile 2,435 (33.1) 680 (33.2) 584 (34.5) Second tertile 2,403 (32.6) 714 (34.9) 582 (34.4) Third tertile 2,530 (34.3) 653 (31.9) 527 (31.1) Marital status 0.002 Married/cohabiting 6,537 (88.7) 1,803 (88.1) 1,450 (85.7) Single 831 (11.3) 244 (11.9) 243 (14.3) Never smoking <0.001 Yes 4,268 (57.9) 1,248 (61.0) 1,129 (66.7) No 3,100 (42.1) 799 (39.0) 564 (33.3) No heavy alcohol consumption <0.001 Yes 6,536 (88.7) 1,834 (89.6) 1,565 (92.4) No 832 (11.3) 213 (10.4) 128 (7.6) Normal weight 0.315 Yes 3,030 (41.1) 812 (39.7) 670 (39.6) No 4,338 (58.9) 1,235 (60.3) 1,023 (60.4) No central obesity 0.401 Yes 2,216 (30.1) 624 (30.5) 484 (28.6) No 5,152 (69.9) 1,423 (69.5) 1,209 (71.4) Reasonable sleep <0.001 Yes 3,418 (46.4) 693 (33.9) 507 (30.0) No 3,950 (53.6) 1,354 (66.1) 1,186 (70.0) New-onset hypertension* 0.075 No 3,322 (75.6) 916 (74.8) 680 (72.0) Yes 1,074 (24.4) 308 (25.2) 264 (28.0) New-onset diabetes* <0.001 No 5,766 (89.1) 1,542 (86.8) 1,242 (85.9) Yes 705 (10.9) 234 (13.2) 204 (14.1) New-onset dyslipidemia* 0.197 No 2,959 (52.4) 780 (51.5) 610 (49.6) Yes 2,684 (47.6) 733 (48.5) 619 (50.4) New-onset CVDs* <0.001 No 5,554 (84.3) 1,383 (79.7) 972 (74.5) Yes 1,031 (15.7) 352 (20.3) 332 (25.5) New-onset MM* <0.001 No 4,656 (76.8) 1,238 (75.2) 942 (71.4) Yes 1,407 (23.2) 409 (24.8) 377 (28.6) New-onset CMC* <0.001 No 5,968 (88.2) 1,549 (85.2) 1,142 (81.1) Yes 798 (11.8) 270 (14.8) 266 (18.9) Abbreviation: CVDs=cardiovascular diseases; MM=metabolic multimorbidity; CMC=cardiometabolic comorbidity; IQR=interquartile range.
* means the sample size used was less than 11,108.Table 1. Baseline characteristics of participants by chronic pain severity (N=11,108).
Outcomes HR (95% CI) No Mild Severe Hypertension 1.00 (0.94–1.07) 0.99 (0.88–1.10) 1.09 (0.97–1.23) Diabetes 1.00 (0.92–1.08) 1.15 (1.02–1.31) 1.22 (1.06–1.40) Dyslipidemia 1.00 (0.96–1.04) 1.02 (0.95–1.10) 1.09 (1.01–1.18) CVDs 1.00 (0.94–1.07) 1.31 (1.18–1.46) 1.70 (1.53–1.90) MM 1.00 (0.95–1.06) 1.04 (0.95–1.15) 1.23 (1.11–1.37) CMC 1.00 (0.93–1.08) 1.26 (1.12–1.41) 1.64 (1.45–1.85) Note: All models were adjusted for age, sex, residence, education, household income, marital status, and healthy lifestyles. Bolded indicates statistical significance.
Abbreviation: HR=hazard ratio; CI=confidence interval; CMDs=cardiometabolic disorders; MM=metabolic multimorbidity; CMC=cardiometabolic comorbidity; CVDs=cardiovascular diseases.Table 2. Association of chronic pain severity with new-onset CMDs, MM, and CMC.
Figure 2 illustrates a significant association between healthy lifestyles and decreased risks of CMDs, MM, and CMC for participants without chronic pain or with mild to severe chronic pain. The P values for interaction between chronic pain and healthy lifestyles were >0.05. Figure 3 demonstrates how adopting a healthy lifestyle can reverse the associations between chronic pain and diabetes, dyslipidemia, MM, and CMC. The statistical analysis indicates that individuals with severe chronic pain and with the healthiest lifestyles were 30%–50% less likely to develop diabetes, dyslipidemia, MM, and CMC compared to individuals with no chronic pain and with the unhealthiest lifestyles. Moreover, healthy lifestyles had a neutralizing effect on the associations between severe chronic pain and CVDs. Therefore, adopting healthy lifestyles can weaken the positive correlations between chronic pain and CVDs.
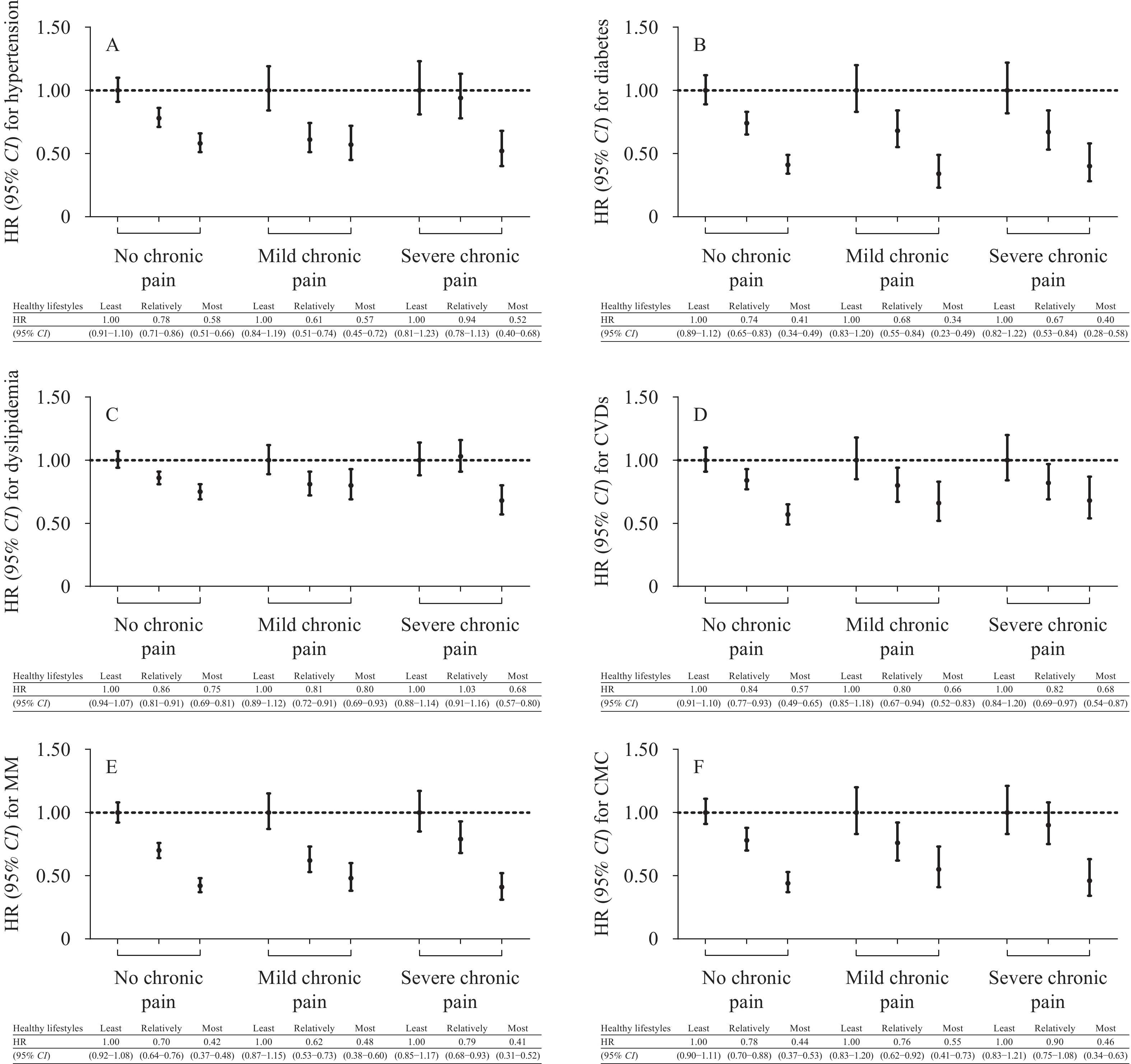 Figure 2.
Figure 2.Association of healthy lifestyles with new-onset CMDs, MM, and CMC in participants with no, mild, and severe chronic pain. (A) Healthy lifestyles with new-onset hypertension; (B) Healthy lifestyles with new-onset diabetes; (C) Healthy lifestyles with new-onset dyslipidemia; (D) Healthy lifestyles with new-onset CVDs; (E) Healthy lifestyles with new-onset MM; (F) Healthy lifestyles with new-onset CMC.
Note: The reference was assigned as the “Least healthy lifestyles” to explore whether the associations between adopting healthy lifestyles and outcomes differ in participants with different pain severity. All models were adjusted for age, sex, residence, education, household income, and marital status.
Abbreviation: HR=hazard ratio; CI=confidence interval; CMDs=cardiometabolic disorders; MM=metabolic multimorbidity; CMC=cardiometabolic comorbidity; CVDs=cardiovascular diseases.
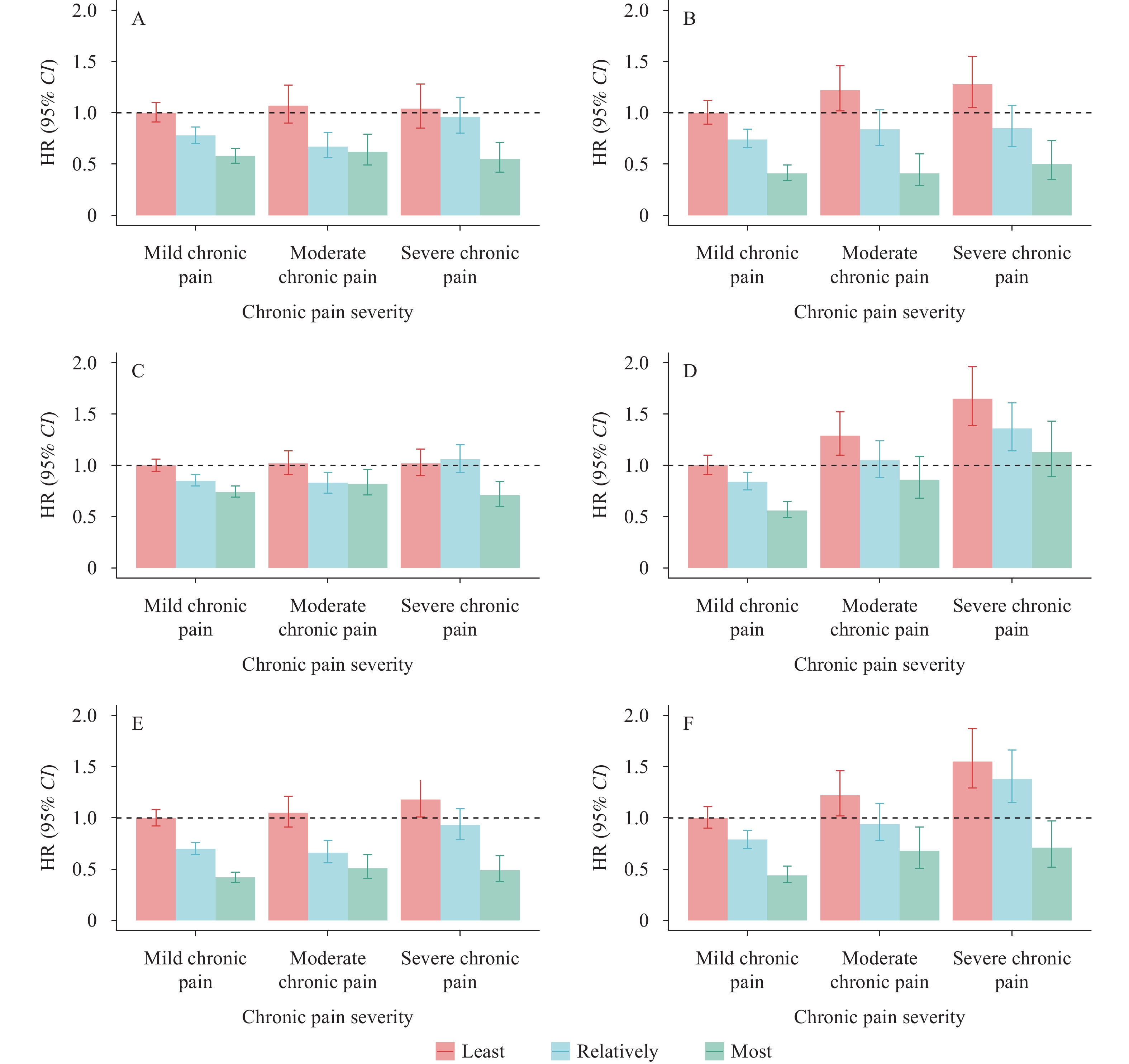 Figure 3.
Figure 3.The dilution effect of healthy lifestyles on the associations of chronic pain severity with new-onset CMDs, MM, and CMC. (A) Dilution effect of healthy lifestyles on hypertension; (B) Dilution effect of healthy lifestyles on diabetes; (C) Dilution effect of healthy lifestyles on dyslipidemia; (D) Dilution effect of healthy lifestyles on CVDs; (E) Dilution effect of healthy lifestyles on MM; (F) Dilution effect of healthy lifestyles on CMC.
Note: The reference was assigned as “Mild chronic pain and least healthy lifestyles” to explore whether adopting healthy lifestyles can dilute or even mask the risks attributed to chronic pain. All models were adjusted for age, sex, residence, education, household income, and marital status.
Abbreviation: HR=hazard ratio; CI=confidence interval; CMDs=cardiometabolic disorders; MM=metabolic multimorbidity; CMC=cardiometabolic comorbidity; CVDs=cardiovascular diseases.
-
This cohort study revealed a significant association between chronic pain and heightened risks of diabetes, dyslipidemia, CVDs, MM, and CMC. Our research further found that adopting healthy lifestyle can successfully mitigate the risks of chronic pain-induced diabetes, dyslipidemia, MM, and CMC, and partially alleviate certain CVD risks.
Prior research has shown that chronic pain is linked to CVDs (4). The occurrence of chronic inflammation, which often coexists with chronic pain, can elucidate the significant associations of chronic pain with CMDs. Even minor degrees of chronic inflammation can heighten the chances of insulin resistance and atherosclerosis, both of which play a role in the etiology of CVDs (5). Oxidative stress, another potential factor behind chronic pain, can give rise to insulin resistance and hyperlipidemia, which increase the risk of CVDs (6). Additionally, individuals with chronic pain are more prone to developing mental health disorders, such as depression, which is highly correlated with cardiometabolic risk (7). Nevertheless, the association between chronic pain and hypertension in our study is weak. The impact of analgesic medications used to alleviate chronic pain on blood pressure varies, which may account for the absence of significant associations. However, data related to this point were limited in the CHARLS.
Previous research has shown that adopting healthy lifestyles can effectively lower the risk of CMDs (8). This study presents a significant finding that healthy lifestyle choices can mitigate or even reverse risks of CMDs, MM, and CMC associated with chronic pain. Healthcare providers often recommend healthy lifestyle changes to chronic pain patients to alleviate their symptoms, decrease the likelihood of developing depression, nervous system disorders, and subsequently, cardiometabolic risks (9). Adopting a healthy lifestyle approach can also reduce inflammation, which has a significant association with chronic pain and CMDs. Conversely, unhealthy lifestyle choices, such as smoking, can quicken the progression of inflammation and lower the pain threshold, exacerbating chronic pain symptoms (10). Furthermore, through lifestyle changes, the interconnected relationship between uric acid-based diseases and metabolic-based diseases can be moderated, which is a matter of concern for future research.
The present study has certain limitations that should be acknowledged. First, due to data limitations, we were unable to include information on exercise and dietary intake. Nonetheless, we utilized BMI and WHtR as proxies, which may partially compensate for the absence of exercise and dietary intake data. Second, we did not consider medical therapies for chronic pain due to data limitations, which may have an impact on the conclusions reached in this study. Moreover, we identified CVDs based on self-reported physician diagnoses and/or ongoing treatments, which may introduce bias. Lastly, our approach to amalgamating various healthy lifestyles may attenuate the influence of individual health practices. To investigate the associations between various healthy lifestyles and chronic pain as well as comorbidities related to metabolism, it will be necessary to conduct future research that is specific to individual health practices.
In this study, we discovered that chronic pain is a risk factor for CMDs, MM, and CMC. It was observed that practicing healthy lifestyles can help to mitigate or even reverse the risks associated with chronic pain regarding these health conditions. Through our findings, we have demonstrated the need for lifestyle interventions in chronic pain patients to alleviate their pain severity as well as lessen their later cardiometabolic risks. Ultimately, this can promote the development of healthy aging in China, making it an important avenue to explore for future research.
-
No conflicts of interest.
-
China Center for Economic Research, National School of Development, Peking University, Beijing, China.
HTML
| Citation: |



 Download:
Download:




