-
Heart disease (HD) is an important component of the spectrum of cardiovascular diseases (CVDs). China has the highest number of new HD cases in the world (1), posing significant health and economic burdens to society. However, its mortality trends at the national level and urban-rural differences remain unclear. This study, which identifies the age, period, and cohort effects of HD mortality trend changes, would assist the government in understanding future trends and optimizing public health policies. The HD mortality data by age, gender, and region were extracted from China’s National Health Commission’s death registration system, after quality control of ID and duplicate removal (2). The age-standardized mortality rate was calculated based on the world standard population using the direct method. Joinpoint regression was employed to determine HD mortality change patterns across time (3). The age-period-cohort model was used to estimate cohort and period effects (4). In this model, age refers to the individual’s age at a given time, period refers to the time at which the outcome is measured, and cohort refers to the group of individuals born in a particular period. This study revealed that HD mortality in China has rapidly increased over the past two decades, with men increasing faster than women and rural areas increasing faster than urban areas. It is essential for healthcare providers to prioritize their attention towards heart disease among older males living in rural areas.
Figure 1 shows the long-term trends in crude and age-standardized mortality rates for HD in China’s urban and rural populations by gender from 1987–2021. The crude mortality rates from HD showed a significant upward trend in all gender groups and areas during the study period, particularly in rural areas, where the mortality from HD rose sharply since 2005. In metropolitan areas, the crude HD mortality increased by 1.78-fold, with increases of 1.95-fold for men and 1.62-fold for women. In rural regions, the mortality rate increased by 2.11-fold, with 2.22-fold increase for males and 1.99-fold increase for women. However, the increasing trend of mortality after standardization was not as pronounced, showing a stable fluctuation. In general, men had a higher HD mortality than women, and rural areas had a higher mortality than cities.
 Figure 1.
Figure 1.Trend of crude and age-standardized mortality rates from heart disease in China from 1987 to 2021.
The results of the joinpoint regression describing the mortality trends are presented in Table 1. The results indicate that the fastest increasing interval for heart disease mortality in urban areas of China was from 2002–2010, while the fastest increasing period in rural areas was from 2005–2011, which corresponded to the time of the fastest economic growth rate in China. The age-standardized mortality in urban areas showed a small downward trend, while rural mortality rates varied more but remained relatively stable over the last decade.
Subgroup Mortality rate (per 100,000) Total study period§ Period 1 Period 2 Period 3 Period 4 Period 5 1987 2021 AAPC (%) 95% CI Years APC (%) Years APC (%) Years APC (%) Years APC (%) Years APC (%) Crude mortality Heart disease in urban areas Total 92.84 165.37 1.6* (0.3, 3.0) 1987–1993 −1.2 1993–1999 4.3* 1999–2002 −9.0 2002–2009 6.0* 2009–2021 2.1* Male 87.74 171.26 1.9* (0.5, 3.3) 1987–1993 −0.5 1993–1999 4.8* 1999–2002 −8.6 2002–2010 5.9* 2010–2021 1.8* Female 98.26 159.40 1.3* (0.0, 2.5) 1987–1992 −2.9* 1992–1999 3.2* 1999–2002 −8.9 2002–2009 5.6* 2009–2021 2.1* Heart disease in rural areas Total 89.73 188.58 2.3* (0.9, 3.7) 1987–1992 −6.0* 1992–2001 2.5* 2001–2005 −6.0 2005–2009 15.9* 2009–2021 4.3* Male 86.45 192.09 2.4* (0.8, 4.1) 1987–1992 −6.0* 1992–2002 2.8* 2002–2005 −9.2 2005–2009 17.8* 2009–2021 4.1* Female 93.13 184.93 2.2* (0.4, 4.1) 1987–1995 −3.9* 1995–1998 9.9 1998–2005 −2.5 2005–2011 10.0* 2011–2021 4.1* Age-standardized mortality† Heart disease in urban areas Total 130.89 94.19 −0.6* (−1.1, −0.2) 1987–2007 −1.5* 2007–2021 0.7 – – – – – – Male 134.15 110.59 −0.5* (−1.0, −0.1) 1987–2007 −1.4* 2007–2021 0.6 – – – – – – Female 126.75 78.63 −1.2* (−2.2, −0.1) 1987–2008 −2.0* 2008–2016 2.3 2016–2021 −3.4 – – – – Heart disease in rural areas Total 130.34 110.60 −0.4 (−2.2, 1.6) 1987–1993 −7.5* 1993–2002 2.6* 2002–2005 −11.1 2005–2010 9.9* 2010–2021 −0.1 Male 140.20 128.48 −0.3 (−2.5, 1.9) 1987–1993 −7.0* 1993–2002 2.2* 2002–2005 −12.6 2005–2009 15.0* 2009–2021 −0.2 Female 123.29 93.54 −0.4 (−2.3, 1.4) 1987–1994 −6.8* 1994−2001 4.1* 2001−2006 −6.5 2006–2010 10.3 2010–2021 0.1 Note: “–” means no joinpoints identified.
Abbreviation: APC=annual percent change; AAPC=average annual percent change; CI=confidence interval.
* Significant difference from zero (P<0.05).
† Standardized to the World Health Organization world standard population.
§ Years 1987 to 2021.Table 1. Joinpoint analysis of crude and age-standardized mortality rates from heart disease in urban and rural areas.
Figure 2 (A–B) shows HD net- and local-drift. Net-drift represents the average yearly trend for the entire population over the previous three decades, while local-drift refers to the average annual trend for distinct age groups. In this study, the overall net-drift pattern was different in rural and urban China. HD mortality decreased significantly in the urban population across the whole study period {−0.84% [95% confidence interval (CI): −1.40 to −0.28]}, while the general tendency was not noticeable in rural regions [−0.51% (95% CI: −1.23 to −0.21)]. Local-drift reflects the further age variability in mortality trends. The data indicate that mortality among those aged 60 and older exhibits a considerable upward tendency. In terms of gender, the mortality rate of male residents between the ages of 15 and 60 is increasing, with this effect being more pronounced in rural regions, while the mortality rate of female residents in both urban and rural areas is decreasing consistently.
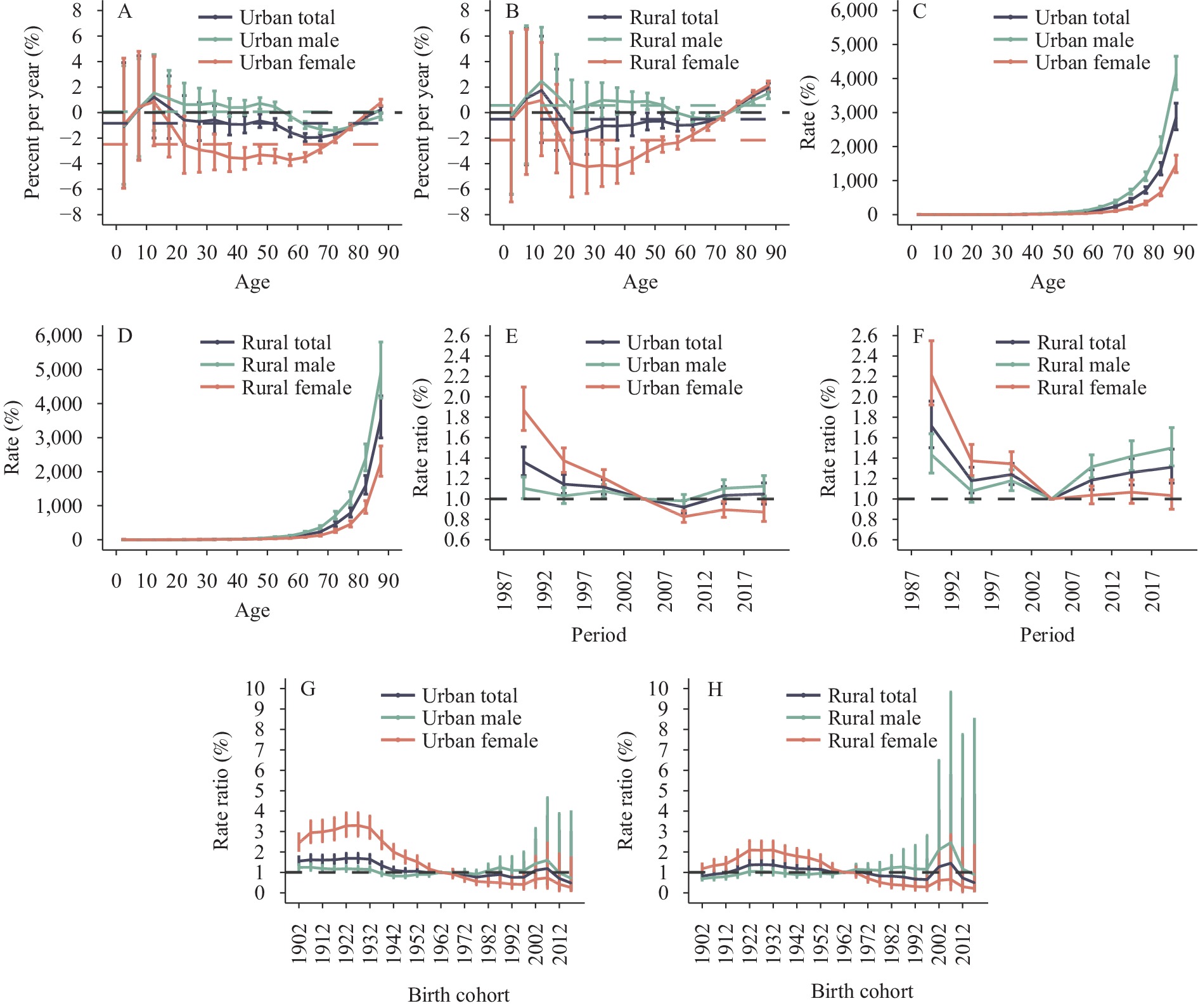 Figure 2.
Figure 2.Parameter estimates of age, period, and cohort effects on heart disease mortality rates in rural and urban China from 1987 to 2021. (A) Net and local drifts in urban areas; (B) Net and local drifts in rural areas; (C) Age effects in urban areas; (D) Age effects in rural areas; (E) Period effects in urban areas; (F) Period effects in rural areas; (G) Cohort effects in urban areas; (H) Cohort effects in rural areas.
Figure 2 (C–H) presents the effects of age, period, and cohort on HD mortality in China. The age effects manifested as an expected exponential curve, with mortality rates increasing exponentially with age. Mortality increased rapidly in older ages, with a higher rate of increase in rural areas than in urban areas and higher in men than in women. Period effects tended to show the same patterns across gender and regions, with a strikingly descending trend from 1987–2005, suggesting significant improvements across the study period. However, since 2007, HD mortality rate in urban and rural areas has shown an increasing trend. Cohort effects tended to show similar patterns between rural and urban areas, with the most striking improvements across birth cohorts in the urban female population and a progressive improvement in mortality in those born from 1930 onward. For the male population, there was little improvement.
-
Previous studies have demonstrated a high burden of HD in China, but few studies have recorded urban versus rural HD mortality rates over a long period. This paper examines China’s HD mortality patterns over the past 35 years, emphasizing the age-period-cohort effects from an urban-rural viewpoint. This study revealed that China’s HD mortality has risen sharply in the previous 20 years, with mortality increasing at a faster rate among men than among women, particularly in rural regions compared to cities. The age-standardized mortality rate (ASMR) of HD is relatively stable, but it also showed a large increasing trend from 2005 to 2010. This finding indicates that the escalation of HD mortality in China is not solely driven by the primary factors of population aging, but rather that social-environmental factors also serve as significant contributing factors. Socio-economic factors, such as poverty, low education levels, and lack of access to healthcare, have been proven to be risk factors for HD, and people who live in poverty may have limited access to healthy foods, healthcare, and safe places to exercise, which can all contribute to the development of HD. Environmental factors, such as air pollution and exposure to toxins, can also contribute to HD. Air pollution can damage the blood vessels and increase the risk of heart disease, while exposure to toxins can also damage the heart and blood vessels. Multiple other factors, such as diabetes mellitus, high blood pressure, unhealthy diet, obesity, cigarette and alcohol use, and physical activity may also contribute to the development of HD (5).
Previous research indicates that the prevalence of HD and accompanying mortality has shifted from developed to developing countries in recent decades, and the high prevalence of obesity, hypertension, diabetes, and hyperlipidemia due to the prevalence of Western lifestyles is the leading cause of HD deaths (6). The period between 2002 and 2011 marked the fastest increase in HD deaths within the Chinese population. Notably, these were also the years when China experienced the fastest economic growth. Dramatic lifestyle changes, environmental pollution, and a large unmet medical need may have contributed to the rapid increase in HD deaths (7-8).
Significant regional differences in HD mortality were observed, with urban deaths being higher than rural deaths until 2013. However, in recent years, rural areas have begun to outpace urban areas, resulting in a widening urban-rural gap. It is likely that smoking, drinking alcohol, and other risk factors, such as high serum cholesterol and blood pressure, have contributed to the higher HD mortality in rural China (9).
At the same time, trends in HD deaths show significant gender and age differences. Men have always been at high risk for HD deaths, and this situation has not improved due to socioeconomic risk factors. Biological, lifestyle, and psychosocial factors may explain this gender disparity (10). Both period and cohort effects show that HD deaths in older groups are increasing, indicating that these populations need special attention. To conclude, the rising mortality from HD and the burden on rural and elderly populations remain a significant public health priority for the Chinese government. It is imperative for healthcare providers to prioritize their attention towards heart disease among older males living in rural areas. Such a targeted approach would contribute to the improvement of overall health and well-being in China.
This study has several limitations. First, the APC effects were estimated using cross-sectional data, not panel data. Second, in addition to urban-rural differences, there are also significant socioeconomic differences between local regions in China, so more fine-grained mortality data for HDs (e.g., provinces) need to be further analyzed. Third, the mortality data were categorized using different ICD versions, ICD-9 before 2002 and ICD-10 subsequently in China, which may affect the accuracy of the trends of CVDs due to an incomplete match. Previous publications have indicated that there is an underreporting of 2%–5% in the mortality data used in this study (2); however, this does not affect the research and analysis of the overall trend.
HTML
| Citation: |




 Download:
Download:




