-
Patients with tuberculosis (TB) may experience delays in seeking care for their illness, as well as in obtaining accurate diagnoses and timely treatments. The coronavirus disease (COVID-19) pandemic has the potential to exacerbate these issues, negatively impacting access to TB diagnosis and treatment. Between 2018 and 2022, the number of reported incident TB cases has declined, while trends regarding delays among TB patients remain unclear. This study analyzed records of TB patients reported between 2018 and 2022 across 32 provincial-level administrative divisions (PLADs) in China to determine the long-term trends in delays experienced by TB patients before and during COVID-19 epidemic in China. There were 3,270,346 TB patients involved in the final analysis. The median interquartile range (IQR) of total delay was 29 (12–59) days. Patient delay, diagnosis delay, and treatment delay were 20 (6–46) days, 1 (0–8) days and 0 (0–0) days, respectively. TB patients who were agriculture workers, minorities, detected through passive case finding methods, complicated with comorbidities, and human immunodeficiency virus (HIV) positive had relatively higher patient delays than other subgroups. Patient delay was shorter in eastern regions than in western and central regions. Health education and active screening need to be promoted and expanded among high-risk groups and regions with prolonged patient delay.
TB is a major public health problem. In China, there were an estimated about 780,000 incident TB patients and 30,000 died from the disease in 2021 (1). Prompt diagnosis and treatment are crucial for effective TB management and control; however, delays in seeking care are common among TB patients. Delays can occur at any stage from symptom onset to treatment initiation and are typically classified into patient delay (from symptom onset to first medical consultation), diagnostic delay (from first medical consultation to confirmed diagnosis), treatment delay (from confirmed diagnosis to treatment initiation), and total delay (from symptom onset to treatment initiation). Prolonged delays in TB diagnosis and treatment can lead to adverse outcomes, spread of the TB bacteria within communities, and the emergence of multidrug-resistant TB (2-3).
Globally, the COVID-19 pandemic had a damaging impact on access to TB diagnosis and treatment and the burden of TB disease (1). Many factors like nonpharmaceutical interventions (NPIs) and declines in income may affect patients’ health care seeking behavior when people become unwell, causing delays in TB diagnosis and treatment. A previous study conducted in 2020 showed that in early period of pandemic, delays for TB patients had not been deeply affected in China. Nevertheless, notification and follow-up examinations were affected significantly (4), and these still continue to impact China’s TB control. The notification number of incident TB patients has declined by 26.4% between 2018 and 2021 (1,5). Whether this effect will have an impact on delays is worrying. This study aimed to analyze long-term trends of delays in TB patients before and during COVID-19 epidemic in China, and describe the socio-demographic, clinical, and tempo-geographic variances of delays among them.
Records of TB patients in 32 PLADs in China, including the Xinjiang Production and Construction Corps, were examined between January 1, 2018, and December 31, 2022. These records were extracted as a Comma-Separated Values (CSV) file from the Chinese Disease Control and Prevention Information System. The analysis included cases with accurate dates of symptom onset, initial medical consultation, and treatment initiation. Data variables were processed in an Microsoft Excel (version 2016; Microsoft Corporation, WA, USA) spreadsheet. Median and IQR were used to summarize delays. Delays were derived from different dates recorded. Illogical delay results (e.g., negative numbers) were excluded from the final analysis. Case finding pathways were derived into two categories: 1) active for those detected through active screening and physical examination; and 2) passive for those detected through direct visiting to designated health facilities, referral, tracing, and recommendation by general health facilities. Descriptive and statistical analysis was done with SAS (version 9.4, SAS Institute, NC, USA). Figures were created using R software (version 4.0.3; R Core Team,Vienna, Austria). The medians of patient delays in different regions were assessed with Kruskall-Wallis independent-samples median test, and pairwise comparisons were further assessed with Dwass, Steel, Critchlow-Fligner (DSCF) tests. A two-sided P-value of 0.05 or less was regarded as significant.
-
A total of 3,270,346 TB patients were included in the final analysis, representing 99.6% of reported TB cases between January 1, 2018, and December 31, 2022. Sociodemographic, clinical, and management characteristics of the patients are presented in Table 1.
Group Number and percentage (%) Patient delay
Median (IQR)Diagnosis delay
Median (IQR)Treatment delay
Median (IQR)Total delay
Median (IQR)Total 3,270,346 (100) 20 (6–46) 1 (0–8) 0 (0–0) 29 (12–59) Gender Male 2,239,756 (68.5) 20 (6–46) 1 (0–8) 0 (0–0) 29 (12–59) Female 1,030,590 (31.5) 20 (6–47) 1 (0–8) 0 (0–0) 29 (12–60) Age group (years) 0–14 33,680 (1.0) 15 (5–35) 0 (0.7) 0 (0–0) 22 (10–44) 15–64 2,369,406 (72.5) 20 (6–45) 1 (0–8) 0 (0–0) 28 (12–58) 65 and above 867,260 (26.5) 21 (7–49) 1 (0–8) 0 (0–0) 30 (14–62) Occupation Agriculture workers 2,027,622 (62.0) 22 (7–50) 1 (0.7) 0 (0–0) 30 (13–62) Houseworkers or unemployees 463,394 (14.2) 19 (5–45) 2 (0–11) 0 (0–0) 28 (12–59) Industrial workers 140,458 (4.3) 16 (4–39) 2 (0–10) 0 (0–0) 24 (10–51) Students 200,555 (6.1) 14 (4–32) 1 (0–8) 0 (0–0) 20 (9–41) Retirees 167,760 (5.1) 18 (6–43) 2 (0–13) 0 (0–0) 28 (12–58) Others 270,557 (8.3) 15 (4–38) 2 (0–12) 0 (0–0) 24 (10–51) Ethnics Han 2,724,054 (83.3) 19 (6–45) 1 (0–9) 0 (0–0) 28 (12–58) Minorities 546,292 (16.7) 25 (8–53) 1 (0–6) 0 (0–1) 31 (13–64) Residence Local 2,571,272 (78.6) 21 (7–47) 1 (0–7) 0 (0–0) 29 (13–60) Migrant–within province 519,054 (15.9) 19 (5–45) 2 (0–12) 0 (0–0) 28 (12–59) Migrant–out of province 180,020 (5.5) 14 (3–37) 3 (0–12) 0 (0–0) 23 (10–51) Case finding Active 125,664 (3.8) 15 (4–34) 2 (0–10) 0 (0–1) 23 (9–52) Passive 3,144,682 (96.2) 20 (7.47) 1 (0.8) 0 (0–0) 29 (12–60) Classification Pulmonary TB solo 2,829,581 (86.5) 20 (6–46) 1 (0–8) 0 (0–0) 29 (12–59) Pulmonary TB complicated with extrapulmonary TB 264,018 (8.1) 22 (8–53) 2 (0–11) 0 (0–0) 31 (14–63) Extrapulmonary TB solo 176,747 (5.4) 19 (7–39) 1 (0–9) 0 (0–0) 27 (14–50) Treatment history New 3,012,678 (92.1) 20 (6–45) 1 (0–8) 0 (0–0) 28 (12–58) Retreated 257,668 (7.9) 23 (7–60) 1 (0–8) 0 (0–0) 31 (13–73) Bacteriological results Positive 1,606,960 (49.1) 21 (7–53) 1 (0–8) 0 (0–0) 30 (12–63) Negative 1,605,704 (49.1) 19 (6–42) 1 (0–8) 0 (0–0) 28 (12–54) Unknown 57,682 (1.8) 16 (4–40) 0 (0–5) 0 (0–0) 24 (9–52) Radiological examination With TB lesion 2,830,766 (86.6) 20 (7–46) 1 (0–8) 0 (0–0) 29 (13–60) Without TB lesion 15,973 (0.5) 19 (5–52) 0 (0–7) 0 (0–0) 28 (10–64) Unknown 423,607 (12.9) 18 (5–44) 1 (0–8) 0 (0–0) 25 (10–55) Drug resistance Rifampin resistant 49,593 (1.5) 22 (6–61) 1 (0–8) 0 (0–0) 31 (11–70) Rifampin sensitive 1,174,187 (35.9) 21 (6–52) 1 (0–8) 0 (0–0) 29 (12–62) Unknown 2,046,566 (62.6) 19 (6–43) 1 (0–8) 0 (0–0) 28 (13–56) Comorbidities Yes 383,161 (11.7) 23 (7–59) 2 (0–10) 0 (0–0) 32 (14–67) No 1,734,878 (53.1) 20 (6–46) 1 (0–8) 0 (0–0) 28 (12–59) Unknown 1,152,307 (35.2) 19 (6–43) 1 (0–8) 0 (0–0) 28 (12–56) HIV Positive 25,512 (0.8) 27 (9–57) 1 (0–10) 0 (0–0) 33 (15–66) Negative 1,905,867 (58.3) 20 (6–46) 1 (0–9) 0 (0–0) 28 (12–60) Unknown 1,338,967 (40.9) 20 (6–45) 1 (0–7) 0 (0–0) 29 (12–59) Note: Patient delay means from symptom onset to first seeking medical care; Diagnosis delay means from first seeking medical care to diagnosis confirmation; Treatment delay means from diagnosis confirmation to treatment initiation; Total delay means from symptom onset to treatment initiation.
Abbreviation: TB=tuberculosis; PLADs=provincial-level administrative divisions; HIV=human immunodeficiency virus; IQR=interquartile range.Table 1. Baseline characteristics and timeliness of TB patients notified in 32 PLADs in China, 2018–2022.
The median and IQR of total delay and its components among TB patients notified between January 1, 2018, and December 31, 2022 was 29 (12–59) days, with patient delay constituting the largest component at 20 (6–46) days. Median (IQR) diagnosis and treatment delays were 1 (0–8) days and 0 (0–0) days, respectively. Male and female TB patients exhibited similar delays. Patients aged 65 and older experienced longer delays than younger age groups. Among various occupations, agricultural workers such as farmers, herdsmen, and fishermen experienced the longest total (30, 13–62) and patient delays (22, 7–50), while students had the shortest (20, 9–41 and 14, 4–32, respectively). Ethnic minorities experienced higher total (31, 13–64) and patient delays (25, 8–53) compared to the Han population (28, 12–58 and 19, 6–45). Migrants from other PLADs had the shortest patient delay (14, 3–37) but the longest diagnosis delay (3, 0–12) compared to local residents and migrants within PLAD. Longer total delays were observed among TB patients detected through passive case-finding (29, 12–60), those who were retreated (31, 13–73), bacteriologically positive (30, 12–63), with radiological TB lesions (29, 13–60), rifampin-resistant (31, 11–70), with comorbidities (32, 14–67), and HIV-positive (33, 15–66) patients, with similar patient delays. Patients with only pulmonary lesions experienced shorter delays compared to those with both pulmonary and extrapulmonary lesions, though patients with only extrapulmonary lesions had the shortest delays.
Trends in diagnosis, treatment, and patient delays have not changed within a 5-year period. Patient delay showed a moderate decrease from 22 (7–48) days in 2018 to 18 (6–43) days in 2021, before increasing slightly to 20 (6–47) days in 2022. These trends were observed in most subgroups, with migrants and individuals identified through active TB screening experiencing a decline over the 5-year period from 2018 to 2022. Conversely, patient delay among those without bacteriological or radiological results exhibited minimal decline and even increased in some years (Table 2).
Group 2018
Median (IQR)2019
Median (IQR)2020
Median (IQR)2021
Median (IQR)2022
Median (IQR)Total 22 (7, 48) 21 (7, 46) 19 (6, 46) 18 (6, 43) 20 (6, 47) Gender Male 21 (7, 28) 21 (7, 46) 19 (6, 46) 18 (6, 43) 20 (6, 47) Female 22 (7, 49) 21 (7, 47) 19 (6, 47) 18 (6, 43) 19 (6, 47) Age groups (years) 0–14 16 (5, 37) 16 (5, 36) 15 (5, 34) 14 (5, 33) 15 (5, 37) 15–64 21 (7, 47) 20 (6, 45) 19 (6.46) 18 (6, 43) 19 (5, 47) 65 and above 24 (8, 52) 23 (7, 49) 21 (7, 49) 20 (7, 45) 21 (7, 48) Occupation Agriculture workers 25 (8, 54) 23 (8, 51) 21 (7, 51) 20 (7, 46) 21 (7, 50) Houseworkers or unemployees 20 (6, 44) 20 (6, 45) 18 (5, 46) 18 (5, 43) 19 (5, 46) Industrial workers 16 (5, 40) 17 (5, 40) 15 (4, 39) 15 (4, 37) 15 (4, 40) Students 14 (4, 33) 14 (4, 32) 14 (4, 32) 13 (4, 31) 14 (4, 34) Retirees 19 (6, 45) 18 (6, 42) 18 (6, 43) 17 (5, 41) 19 (6, 45) Others 16 (5, 38) 15 (4, 37) 14 (4, 38) 14 (3, 36) 16 (4, 41) Ethnics Han 20 (6, 46) 20 (6, 45) 19 (6, 45) 18 (6, 43) 19 (6, 47) Minorities 30 (10, 59) 28 (9, 53) 22 (7, 52) 20 (7, 45) 20 (6, 48) Residence Local 23 (7, 49) 22 (7, 47) 20 (7, 27) 19 (6, 44) 20 (6, 48) Migrant-within province 19 (6, 46) 19 (5, 44) 19 (6, 46) 17 (5, 41) 15 (3, 38) Migrant-out of province 15 (3, 38) 15 (3, 39) 14 (3, 37) 13 (3, 34) 13 (2, 34) Case finding Active 21 (6, 38) 21 (6, 38) 12 (4, 31) 10 (2, 27) 8 (1, 24) Passive 22 (7, 49) 21 (7, 47) 20 (6, 47) 19 (6, 44) 20 (6, 48) Classification Pulmonary TB solo 22 (7, 48) 21 (7, 46) 19 (6, 46) 18 (6, 43) 19 (5, 47) Pulmonary TB complicated with extrapulmonary TB 23 (8, 55) 23 (8, 53) 22 (8, 55) 22 (8, 50) 22 (8, 52) Extrapulmonary TB solo 20 (8, 40) 19 (7, 39) 18 (7, 38) 18 (7, 38) 18 (7, 40) Treatment history New 21 (7, 47) 20 (7, 45) 19 (6, 45) 18 (6, 42) 19 (6, 46) Retreated 27 (8, 61) 25 (7, 61) 23 (7, 61) 21 (7, 53) 20 (6, 58) Bacteriological results Positive 24 (7, 59) 22 (7, 54) 21 (7, 54) 20 (6, 48) 21 (6, 52) Negative 21 (7, 44) 20 (7, 42) 18 (6, 41) 17 (6, 39) 18 (5, 41) Unknown 16 (4, 41) 17 (5, 41) 17 (4, 38) 15 (2, 38) 16 (2, 43) Radiological examination With TB lesion 22 (7, 48) 21 (7, 46) 19 (6, 47) 19 (6, 43) 21 (7, 49) Without TB lesion 23 (7, 59) 18.5 (4, 49) 16 (5, 49) 16 (5, 50) 15 (4, 47) Unknown 14 (1, 36) 13 (1, 35) 15 (2, 39) 14 (3, 35) 19 (5, 46) Drug resistance Rifampin resistant 24 (7, 61) 24 (7, 60) 22 (6, 61) 20 (6, 59) 22 (5, 62) Rifampin sensitive 24 (7, 59) 22 (7, 54) 21 (6, 55) 20 (6, 47) 20 (6, 51) Unknown 21 (7, 46) 20 (7, 43) 18 (6, 42) 17 (6, 40) 18 (5, 43) Comorbidities Yes 27 (9, 61) 25 (8, 61) 22 (7, 60) 21 (7, 52) 23 (7, 57) No 21 (7, 50) 20 (7, 47) 19 (6, 46) 18 (6, 42) 19 (6, 46) Unknown 21 (7, 43) 20 (6, 41) 18 (6, 42) 18 (6, 41) 19 (5, 46) HIV Positive 30 (10, 61) 28 (10, 59) 26 (9, 60) 25 (9, 52) 24 (8, 51) Negative 22 (7, 49) 21 (7, 47) 19 (6, 47) 18 (6, 43) 19 (6, 46) Unknown 21 (7, 47) 20 (7, 44) 20 (6, 46) 19 (6, 43) 20 (5, 47) Note: Patient delay means from symptom onset to first seeking medical care; Diagnosis delay means from first seeking medical care to diagnosis confirmation; Treatment delay means from diagnosis confirmation to treatment initiation; Total delay means from symptom onset to treatment initiation.
Abbrevieation: TB=tuberculosis; PLADs=provincial-level administrative divisions; HIV=human immunodeficiency virus; IQR=interquartile range.Table 2. Patient delays among TB patients across various groups, stratified by year, in 32 PLADs in China, 2018–2022.
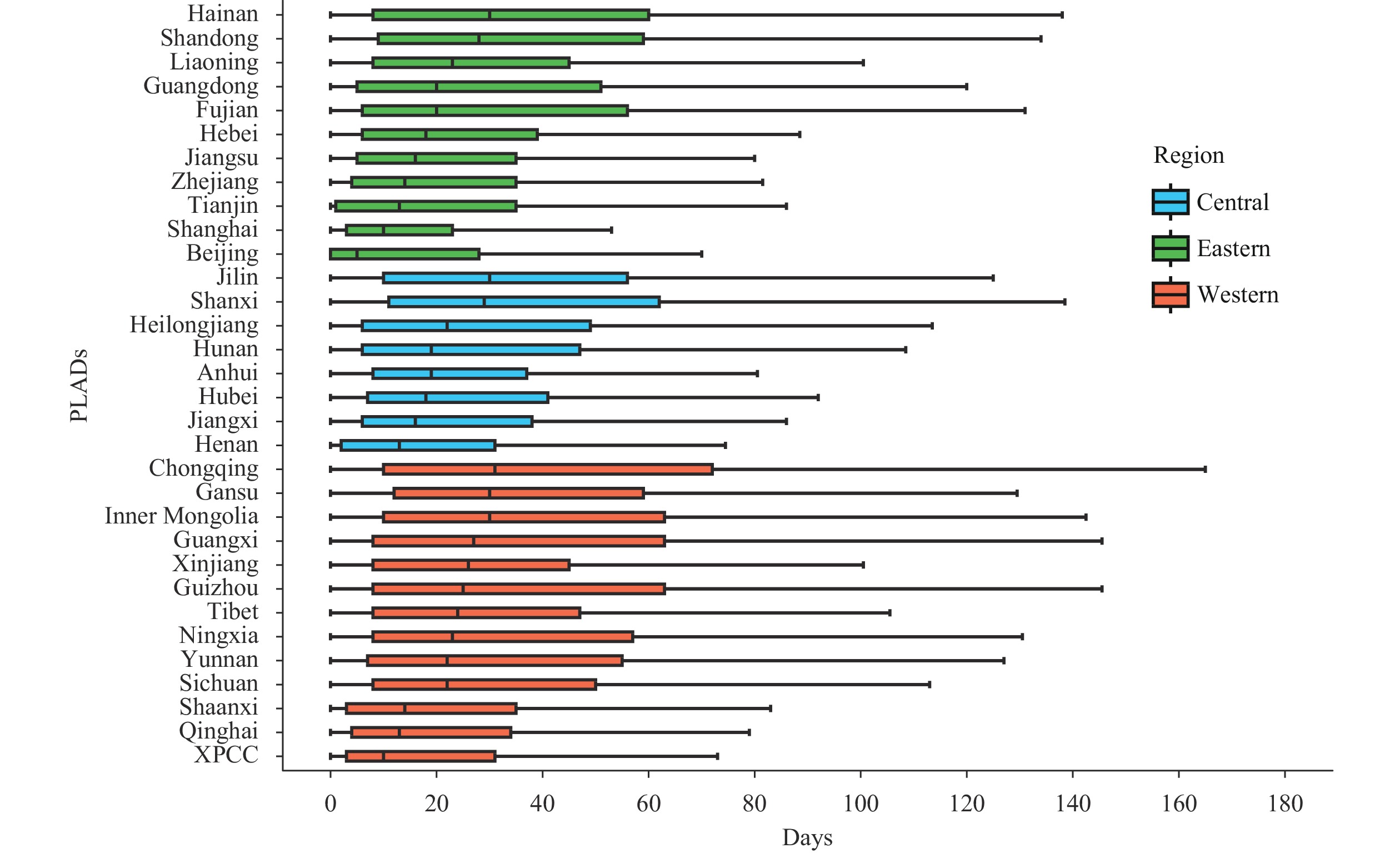
The distribution of patient delay varied across 32 PLADs, ranging from 5 (0–28) days in Beijing to 31 (10–72) days in Chongqing. Overall, patient delay was shorter in eastern regions (27, 11–55) compared to western (30, 13–64) and central regions (29, 13–56), with significant differences (DSCF values =112.0, 59.2; P<0.001). Central regions also had fewer patient delays than western regions (DSCF value =56.5; P<0.001). However, among eastern regions, Hainan had the longest patient delay (30, 8–60), while within western regions, Xinjiang Corps exhibited the shortest patient delay (10, 3–31) (Figure 1).
-
The overall delay experienced by TB patients during the COVID-19 pandemic has slightly decreased compared to pre-pandemic levels. The patient delay was the primary factor contributing to the total delay. TB patients who were agricultural workers, from minority populations, identified through active screening, and those with comorbidities or who were HIV positive experienced relatively longer patient delays compared to other subgroups. Additionally, patient delay was shorter in the eastern regions of the study area compared to the western and central regions.
A previous study conducted in 2021 (6) demonstrated that COVID-19 can influence the behavior of TB patients seeking medical care. Over twenty percent of patients might postpone seeking medical care due to transportation restrictions, disruptions in TB services, and personal reasons. However, the current study did not find any significant increase in delays after 2019. Given that TB is a respiratory disease with symptoms similar to those of COVID-19, the heightened attention paid by patients, communities, and healthcare facilities could be the primary reason for the absence of additional delays. Another contributing factor is China’s strict NPIs strategy during the pandemic period, which caused COVID-19 not to reach true nationwide transmission until the end of 2022. Its impact can vary across time and region according to COVID-19 epidemic and different public health responses. Ningxia has reported a longer patient delay during early 2020 compared to pre-pandemic period (7). On the contrary, pulmonary TB patients in Tianjin experienced a shorter patient delay during almost the same period (8). Nevertheless, the continuous low level of diagnosis and treatment delays can also be evidence for generally non-serious interruption of TB service during COVID-19 epidemic.
Compared to other occupations, agricultural workers often experience poorer health equity. Their remote living conditions and relatively lower income make it more challenging for them to access healthcare facilities when TB symptoms arise. However, the shorter patient delay observed among students may suggest that TB education and control efforts in schools have been effective in recent years. Migrant TB patients have also had less patient delay than local residents in this analysis. Generally, migrant population was considered as one of three major challenges in TB control. Stigma, poor accessibility to health service and many other factors may influence their health-seeking behavior (9). The National TB Program (NTP) started focusing on this vulnerable population since the early 21st century. Many active screening and health promotion activities have been implemented and a specific guideline for cross-regional management of TB patients (10) was launched in 2009. The patient delays were much shorter in eastern regions especially in the biggest cities. It is not surprising that Beijing, Shanghai, and Tianjin had shorter patient delays than most other regions since they have the richest medical resources and people living in these regions may have higher health knowledge. Besides changing individuals’ personal perspectives through health education, active case-finding is the most useful method to reduce patient delay (11). Results from this study further confirmed its effectiveness. However, the proportion of patients detected through active screening still accounted for a minority in all patients. NTP should consider promoting the strategy in larger coverage.
The present study has certain limitations. First, we were unable to quantify the correlation between the COVID-19 pandemic and changes in delays. Furthermore, it is important to note that the number of TB notifications declined by more than a quarter from 2018 to 2021 (1), which could suggest that patients seeking treatment at health facilities exhibited more severe symptoms. In addition, as our study is a retrospective analysis utilizing surveillance data, we could not determine the existence of undetected patients or the impact of these undetected patients on average delays. Lastly, our dataset did not include various social and environmental factors, such as health service accessibility and income, which may have affected the results. Future research should be conducted to identify potential risk factors, especially in different settings, to provide a more comprehensive understanding of the situation.
There is no evidence indicating that delays for TB patients worsened during the COVID-19 pandemic in China. However, the observed increase in patient delays in 2022 warrants attention for ongoing TB control efforts. Health education and active screening should be enhanced and expanded among high-risk populations and in regions experiencing prolonged patient delays.
-
This work was supported by the Epidemic of Tuberculosis Recurrence and Types of Recent Recurrence in Western China (JY22-3-11), Chinese Center for Disease Control and Prevention.
HTML
| Citation: |



 Download:
Download:




