-
Effective prevention and control measures have tamed cervical cancer in most parts of the world. In November 2020, the World Health Organization (WHO) set a 2030 target of 70% cervical cancer screening coverage for women aged 35–45 years. (1) China launched a national free screening program for rural women aged 35–64 years in 2009, in order to combat rising cervical cancer incidence, particularly in younger and rural populations, since the late 1990s (2) and an imbalanced disease burden in the central and western regions (3). It set a goal that screening coverage should reach 50% in women aged 35–64 years by 2025 (4). This study used the latest nationally and provincially representative survey data to estimate screening coverage in China and analyze its key sociodemographic and geographic factors via Rao Scott chi-square tests and logistic regression models. This study still suggests gaps in cervical cancer screening coverage with the WHO 2030 target. It also suggests that national and local policy and financial support should be maintained, health education and outreach efforts should be directed more toward the targeted age groups, and accessibility of health-related services should be further strengthened in the rural areas and central and western regions.
This study estimated China’s latest cervical cancer screening uptake by using newly released national survey data from China Chronic Disease and Nutrition Surveillance in 2018–2019. Women aged 18 years and older were selected from 298 districts/counties across all 31 provincial-level administrative divisions (PLADs) in the mainland of China through multi-stage and cluster randomized sampling. Women were interviewed by trained local health staff about history of previous cervical cancer screening as well as the month and year of the most recent screening, if applicable. A total of 102,779 participants aged 20–64 years old completed the survey, yielding a 95.0% response rate. Among them, 27,471 female participants were excluded from the final analysis because of incomplete sociodemographic data, lack of response to the cervical cancer screening question, or age falling outside the targeted age groups. The screening rates of stratified sociodemographic groups were compared through chi-square tests, and predictors of screening uptake were investigated via multivariate logistic regression analysis. Standard errors (SE) were estimated by Taylor linearization with a finite population correction. Statistical significance was determined using two-sided P<0.05. All statistical analyses were performed over SAS (version 9.4, SAS Institute Inc., Cary, USA).
The final sample consists of 75,308 participants aged 20–64 years old. Participants were 40 years old on average with 44.6% from urban areas, 42.2% from the eastern region of China, 96.9% with health insurance coverage, and 43.8% with health check-ups done in the previous three years (Table 1).
Characteristics No. of participants (N=72,095) Weighted proportion (%)* Age (years) 20–24 1,534 15.9 25–34 8,318 22.0 35–44 12,163 26.7 45–54 24,840 20.0 55–64 25,240 15.2 Area type Urban 33,068 44.6 Rural 39,027 55.4 Location Eastern 26,674 42.2 Central 21,147 32.4 Western 24,274 25.3 Education Primary or less 34,596 31.6 Middle school 21,781 32.3 High school 9,553 16.1 College or above 6,165 20.0 Income (CNY) Q1 (<6,667) 15,278 18.3 Q2 (6,667–13,332) 13,943 18.0 Q3 (13,333–27,999) 13,355 19.2 Q4 (28,000+) 14,142 23.0 Don’t know/refused 15,377 21.5 Employment Employed 47,155 69.1 Housework 14,835 18.3 Retired 6,541 4.3 Unemployed 3,564 8.3 With health insurance No 1,462 3.1 Yes 70,633 96.9 With health check–ups in the past 3 years No 40,195 51.9 Yes 31,900 48.1 Self-assessed health status Poor or fair 41,913 56.5 Good 30,182 43.5 * Percentages are weighted to represent the national total population with poststratification for age and gender. Table 1. Sociodemographic characteristics of female participants aged 20–64 years in the cervical cancer screening survey — China, 2018–2019.
The estimated results show that in 2018–2019, cervical cancer lifetime screening coverage (i.e., the percentage of women who had ever taken screening) reached 43.4% [95% confidence interval (CI): 41.5%–45.3%] in women aged 35–44 years, 39.6% (95% CI: 37.9%–41.4%) in women aged 30–49 years, and 36.8% (95% CI: 35.1%–38.4%) in women aged 35–64 years. (Table 2) Screening coverage peaked at 45.0% in the 40–44 age group and declined to 18.8% in the 60–64 age group. About 90% of the screened women reported doing so within the previous three years.
Sociodemographic variables Screen rates among 20–64 years old
% (95% CI)P-value* 35–64 years old Total Urban Rural Screen rates
% (95% CI)Screen OR (95% CI) Total 29.5 (28.1, 30.9) 32.2 (30.2, 34.2) 26.6 (24.9, 28.3) <0.001 36.8 (35.1, 38.4) Age (years) 20–24 8.6 (6.6, 10.6) 7.8 (4.8, 10.9) 9.5 (6.7, 12.3) 0.473 – – 25–29 19.2 (17.0, 21.3) 21.8 (18.5, 25.1) 15.7 (13.7, 17.7) 0.001 – – 30–34 29.7 (27.3, 32.1) 32.3 (29.0, 35.6) 26.1 (22.9, 29.3) 0.012 – – 35–39 41.7 (39.3, 44.1) 47.3 (44.0, 50.5) 34.9 (31.7, 38.2) <0.001 41.7 (39.3, 44.1) 2.82 (2.48, 3.22) 40–44 45.0 (42.7, 47.2) 48.3 (44.9, 51.6) 41.6 (38.8, 44.3) 0.002 45.0 (42.7, 47.2) 3.51 (3.10, 3.98) 45–49 40.1 (37.8, 42.4) 43.6 (40.4, 46.7) 36.7 (33.7, 39.6) 0.001 40.1 (37.8, 42.4) 3.02 (2.69, 3.39) 50–54 34.5 (32.5, 36.4) 38.6 (35.8, 41.4) 30.4 (27.7, 33.2) <0.001 34.5 (32.5, 36.4) 2.33 (2.13, 2.55) 55–59 27.5 (25.6, 29.3) 30.9 (27.9, 33.9) 24.5 (22.2, 26.7) 0.001 27.5 (25.6, 29.3) 1.60 (1.48, 1.74) 60–64 18.8 (17.2, 20.5) 21.4 (19.0, 23.8) 16.7 (14.6, 18.8) 0.005 18.8 (17.2, 20.5) 1.00 [Reference] Ptrend <0.001 <0.001 <0.001 <0.001 30–49 39.6 (37.9, 41.4) 43.2 (40.7, 45.6) 35.6 (33.6, 37.7) <0.001 – – 35–44 43.4 (41.4, 45.3) 47.8 (44.9, 50.6) 38.5 (36.3, 40.7) <0.001 – – Area type Urban 32.2 (30.2, 34.2) – – 41.1 (38.7, 43.4) 0.92 (0.81, 1.00) Rural 26.6 (24.9, 28.3) – – 32.4 (30.5, 34.4) 1.00 [Reference] Pdifference <0.001 <0.001 Geographic region Eastern 33.4 (31.1, 35.7) 36.0 (33.1, 39.0) 29.3 (26.6, 32.0) <0.001 41.6 (38.9, 44.3) 1.31 (1.12, 1.53) Central 28.1 (25.5, 30.7) 29.9 (25.9, 33.9) 26.6 (23.1, 30.0) 0.242 34.9 (31.9, 38.0) 1.11 (0.93, 1.32) Western 24.8 (23.1, 26.6) 26.6 (24.0, 29.2) 23.4 (21.3, 25.6) 0.070 31.3 (28.9, 33.6) 1.00 [Reference] Pdifference <0.001 <0.001 0.023 <0.001 Education Primary or less 25.3 (23.6, 26.9) 26.4 (23.4, 29.3) 24.8 (23.0, 26.6) 0.348 26.9 (25.2, 28.6) 1.00 [Reference] Middle school 32.1 (30.1, 34.0) 35.3 (32.4, 38.3) 29.2 (27.1, 31.4) <0.001 40.2 (38.2, 42.3) 1.53 (1.40, 1.67) High school 33.5 (30.9, 36.1) 36.0 (32.9, 39.1) 28.1 (23.5, 32.8) 0.011 46.5 (42.9, 50.1) 1.81 (1.58, 2.08) College or above 28.9 (26.3, 31.5) 30.2 (27.2, 33.2) 22.4 (18.3, 26.6) 0.006 55.7 (51.9, 59.4) 1.85 (1.56, 2.20) Ptrend 0.005 0.489 0.493 <0.001 Household income per capita (CNY) Q1 (<6,667) 24.2 (22.3, 26.1) 24.8 (20.0, 29.5) 24.0 (22.0, 26.0) 0.783 29.7 (27.5, 31.8) 1.00 [Reference] Q2 (6,667–13,332) 27.6 (25.7, 29.5) 29.6 (27.3, 31.9) 26.0 (23.4, 28.6) 0.038 34.2 (32.2, 36.1) 1.09 (0.97, 1.23) Q3 (13,333–27,999) 32.4 (30.4, 34.4) 34.0 (31.2, 36.7) 30.2 (27.6, 32.8) 0.054 40.2 (37.9, 42.4) 1.15 (1.01, 1.31) Q4 (>28,000) 36.3 (33.9, 38.7) 37.2 (34.4, 40.1) 33.1 (29.5, 36.6) 0.085 47.3 (44.6, 50.1) 1.24 (1.07, 1.43) Don’t know/refused 26.1 (23.9, 28.3) 28.0 (24.7, 31.4) 24.2 (21.7, 26.8) 0.075 31.8 (28.8, 34.8) 0.92 (0.80, 1.06) Ptrend† <0.001 <0.001 <0.001 <0.001 Employment status Employed 30.5 (29.1, 31.9) 33.4 (31.2, 35.5) 27.6 (25.9, 29.2) <0.001 37.9 (36.2, 39.5) 1.11 (0.96, 1.28) Housework 28.5 (25.9, 31.1) 32.4 (28.5, 36.2) 25.7 (23.1, 28.4) 0.001 33.0 (30.4, 35.6) 1.10 (0.94, 1.30) Retired 35.3 (31.7, 38.9) 35.0 (31.3, 38.6) 45.5 (35.8, 55.2) 0.034 35.8 (32.2, 39.4) 1.00 [Reference] Unemployed 20.3 (17.6, 23.0) 21.7 (18.1, 25.3) 18.1 (14.0, 22.1) 0.215 37.0 (32.4, 41.5) 1.07 (0.84, 1.38) Pdifference <0.001 <0.001 <0.001 0.002 Health insurance No 15.4 (11.9, 18.9) 15.9 (11.5, 20.3) 14.4 (9.1, 19.7) 0.678 21.3 (17.3, 25.4) 1.00 [Reference] Yes 30.0 (28.6, 31.4) 32.9 (30.9, 34.8) 26.9 (25.1, 28.6) <0.001 37.1 (35.4, 38.7) 1.96 (1.57, 2.45) Pdifference <0.001 <0.001 0.001 <0.001 Health check-up in the last 3 years No 20.2 (18.8, 21.5) 20.5 (18.3, 22.7) 19.9 (18.4, 21.4) 0.654 24.5 (22.8, 26.1) 1.00 [Reference] Yes 40.8 (39.1, 42.5) 42.0 (39.8, 44.2) 38.8 (36.2, 41.4) 0.066 51.4 (49.3, 53.2) 3.09 (2.84, 3.36) Pdifference <0.001 <0.001 <0.001 <0.001 Self-assessed health Poor or fair 31.4 (29.9, 32.9) 34.5 (32.2, 36.9) 28.3 (26.7, 29.9) <0.001 37.2 (35.5, 38.8) 1.00 [Reference] Good 27.5 (25.9, 29.1) 29.9 (27.9, 32.0) 24.5 (22.3, 26.7) 0.001 36.2 (34.1, 38.3) 0.85 (0.78, 0.93) Pdifference <0.001 <0.001 <0.001 0.349 Note: Screening rates are all weighted proportions to represent the national total population with poststratification for age and gender.
Abbreviation: OR=odds ratio; CI=confidence interval.
* P-value denotes P-value for difference between urban screening coverage and rural screening coverage in women aged 20–64 years.
† Participants answering “Don’t know/refused” are not included in the calculation.Table 2. Sociodemographic stratifications and multivariate logistic regression results of cervical cancer screening coverage in China, 2018–2019.
Low screening uptake for the 20–64 age groups was found in women with the lowest education (25.3%; 95% CI: 23.6%–26.9%), income (24.2%; 95% CI: 22.3%–26.1%), without health insurance coverage (15.4%; 95% CI: 11.9%–18.9%), without health check-ups in the previous three years (20.2%; 95% CI: 18.8%–21.5%), and in the 20–24 age group (urban, 7.8%; 95% CI: 4.8%–10.9%, vs. rural, 9.5%; 95% CI: 6.7%–12.3%). Screening coverage for women aged 35–64 years in urban areas was 45.6% (95% CI: 42.0%–49.2%) in the eastern region, 37.9% (95% CI: 33.3%–42.5%) in the central region, and 35.3% (95% CI: 32.1%–38.5%) in the western region; for rural women aged 35–64 years, it was 36.0% (95% CI: 32.9%–39.1%) in the eastern region, 32.4% (95% CI: 28.5%–36.3%) in the central region, and 28.3% (95% CI: 25.8%–30.9%) in the western region.
Multivariate logistic regression results for women aged 35–64 years surprisingly revealed that the urban factor was statistically insignificant, if not negative, in predicting screening uptake compared to the rural areas [odds ratio (OR): 0.92; 95% CI: 0.81–1.00]. However, the likelihood of screening in the eastern region still prevailed over the western region (OR: 1.31; 95% CI: 1.12–1.53), whereas the central region showed an insignificant advantage over the western region (OR: 1.11; 95% CI: 0.93–1.32). The likelihood of screening was 96% higher in women with health insurance than in women without health insurance (OR: 1.96; 95% CI: 1.57–2.45), and 2.09 times higher in women with health check-ups during the past three years than in women without health check-ups (OR: 3.09; 95% CI: 2.84–3.36).
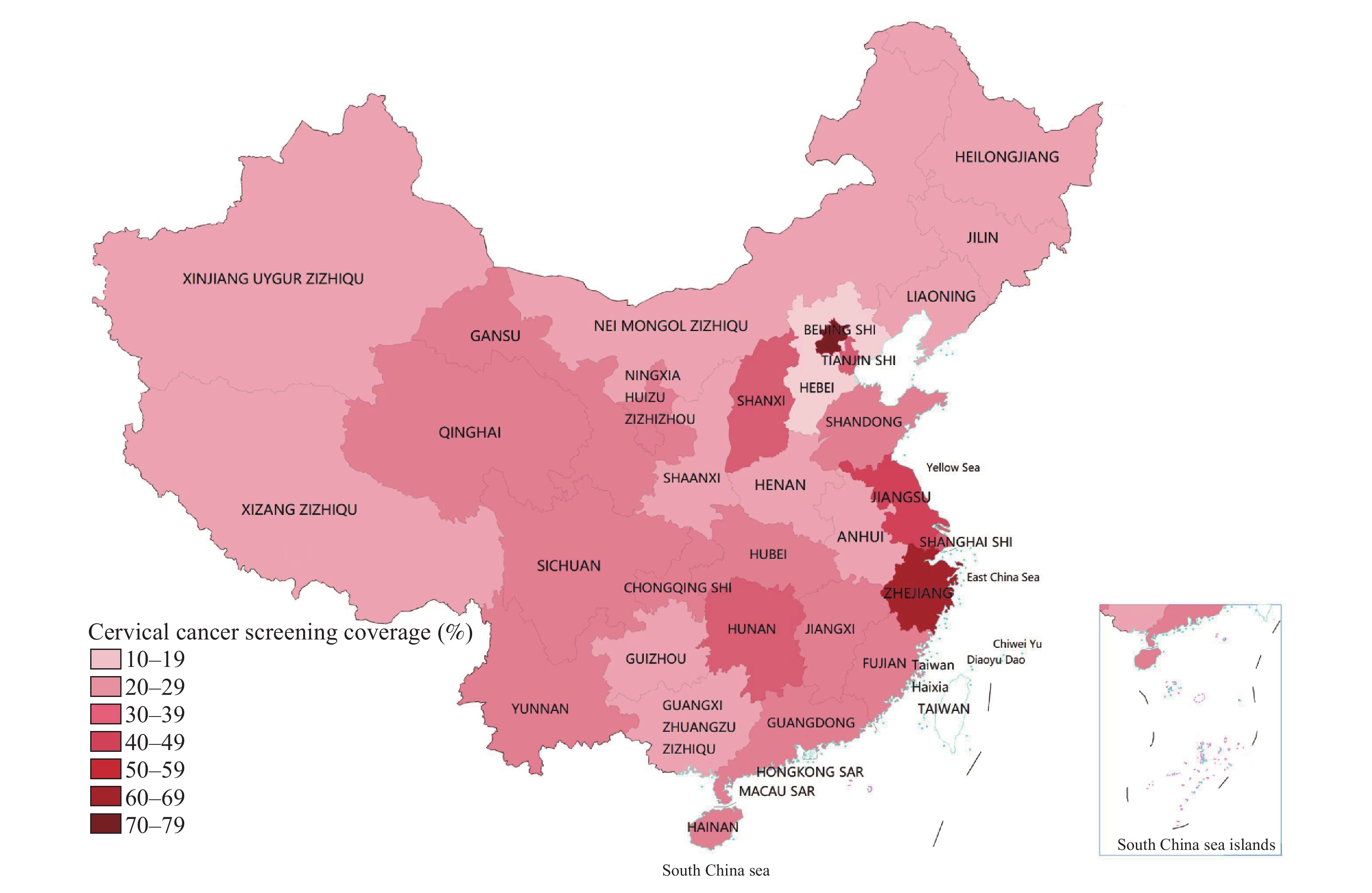
PLADs’ data showed that Beijing Municipality went beyond 70% in screening coverage, followed by Zhejiang Province at above 60%, Jiangsu Province at above 50%, Tianjin Municipality, Hunan Province, and Shanghai Municipality at nearly 50%, while Hebei Province, Xizang (Tibet) Autonomous Region and Guizhou Province fell under 25% in screening coverage (Figure 1).
-
This study estimated that in 2018–2019, 43.4% of women aged 35–44 years, 39.6% of women aged 30–49 years, and 36.8% of women aged 35–64 years had ever participated in cervical cancer screening in China. These results reveal both progress and gaps in cervical cancer screening in China. On the one hand, screening coverage for women aged 35–64 years, the targeted range of China’s national screening program, rose continuously from about 25% in 2010 (5), 27% in 2013 (6), 31% in 2015 (7), to the current 37% in 2018–2019. The upward trend provides strong evidence for the positive impact of the national screening program. Screening coverage for women aged 30–49 years, the age groups recommended by the WHO to monitor screening performance and results (1), also slightly exceeds the estimated worldwide screening coverage of 36% in 2019 (8). On the other hand, the 43% screening coverage for women aged 35–44 years is still far off the WHO 2030 target of 70% screening coverage.
One exciting finding of this study is that traditional disadvantages borne by the rural areas may have begun to dissipate as suggested by multivariate logistic analysis. It again points to the positive impact of the national free screening program in rural areas over the past decade. As the national screening program became the National Basic Public Health Service Program in 2019, national and local policy as well as financial support for cervical cancer screening should be continued to maintain ongoing progress in rural screening uptake. Furthermore, among individual socioeconomic and health-related disparities in screening uptake, which corroborate with previous studies in China and abroad (9), regular health-checkups had strong positive effects over screening uptake, which highlights the importance of strengthened access to health services and health education beyond cancer screening. Moreover, this study suggests excessive screening uptake in the 20–24 age group especially in rural areas, which falls outside the recommended age groups of national screening recommendations (10). To meet the WHO 2030 target, health education and outreach efforts should be directed more toward the targeted age groups.
This study is limited by inaccuracies of self-reported data, potential unequal representation of screening program areas across the sampling regions, and the lack of survey questions on sociopsychological factors of screening uptake. Future studies using administrative data will offer a more definitive look into screening coverage. Qualitative studies on the drivers and barriers of screening uptake will also be helpful in improving screening program design. Moreover, this study only addresses screening coverage without touching upon screening quality control, which is crucial to the effectiveness of any screening program.
In conclusion, this study provides the latest estimate of cervical cancer screening coverage in China based on nationally and provincially representative survey data in 2018–2019. Approximately 43.4% of women aged 35–44 years and 36.8% of women aged 35–64 years reported having had cervical cancer screening in China in 2018–2019. To close the gaps with the WHO target for 2030, national and local policy and financial support should be maintained for cervical cancer screening services, health education and outreach efforts should be focused on targeted age groups, and accessibility of health services should be strengthened in the rural areas and in central and western regions.
HTML
| Citation: |



 Download:
Download:




