-
Adolescents and young people represent a growing share of people living with human immunodeficiency virus (HIV) globally (1). In China, new reported HIV cases among Chinese youth aged 15–24 years reached 16,307 in 2017 (2). The 2016 sentinel surveillance indicated that 82% of newly reported HIV cases among students were among males who reported having sex with males (MSM) (3). Of new HIV cases diagnosed in China, the male to male sexual transmission rate increased from 3.4% in 2007 to 28.2% in 2015, and remained at around 28.2% from 2017 to 2018. (4). Also, China has 146 million adolescents, the second largest adolescent population in the world (5), but the population of adolescent MSM (AMSM) in China has not been well-studied. In 2018, an online survey was conducted in Guangzhou City and Tianjin Municipality to measure risk factors and behaviors for HIV and STIs to better plan prevention programs and service.
Eligible participants were male, aged 15–19 years, reported having oral or anal sex with a male in the past 12 months, and were living or working in Guangzhou or Tianjin. Online sampling used standard respondent driven sampling (RDS) method (6), which are a chain referral method used to sample members of hidden and hard-to-reach populations starting by choosing ‘seed’ participants who have large social networks and are well-known within their communities (7). Once the seed participants complete the survey, they are asked to recruit a set number of their eligible peers (usually up to three) using a uniquely coded coupon. Ongoing successive recruitment of peers results in multiple recruitment waves with the intended goal of eliminating common chain referral biases by the time the calculated sample size is reached. A payment system is used to remunerate participants for completing the survey (primary) and for successfully recruiting eligible participants (secondary).
Due to the hidden nature and vulnerability of AMSM and the popularity of online social networks among this age group in China, this study used a web-based peer-to-peer probability-based sampling technique using WeChat, a Chinese multi-purpose messaging, social media, and mobile payment app. The surveys were conducted in Tianjin (2015 population: 14,722,100) and Guangzhou (2015 population: 12,926,800), both of which have a strong presence of community-based organizations (CBOs) and adolescent networks and are also program sites for the China Comprehensive AIDS Response (China CARES) and UNICEF’s adolescent HIV prevention collaboration with the Chinese government. Formative research and training were conducted with managers from CBOs and adolescent representatives from Guangzhou and Tianjin to identify potential sampling issues related to RDS, to resolve study logistics, to determine AMSM web-use behaviors for rolling out the surveys online, and to design the questionnaire.
A WeChat-based online program accessible via quick response (QR) code was developed and rolled out by CBOs in the two cities. Respondents who received a valid recruitment e-coupon could scan their unique QR code and respond to a set of eligibility questions. Eligible persons were then requested to read the purpose of the survey and provide informed consent, and complete the online questionnaire. Those who completed the entire questionnaire received an 8-digit password for an online payment of 30 CNY (~4.24 USD) via Alipay, administered by the survey software manager. After completing the questionnaire, the respondent received up to 5 coupons with unique QR codes which were used to recruit eligible peers into the survey. Respondents received an additional incentive of 30 CNY for each person they recruited who enrolled and completed the survey. These incentives were also provided online via Alipay and administered by the software manager.
No personal identifying information was collected, no response could be traced back to respondents, and, to avoid duplicates, each IP address could only enroll once. The questionnaire collected data on sociodemographic characteristics, social network sizes, use of MSM social networks, sexual and drug risk, knowledge on HIV and testing services, sexual experiences, perceptions, experience with buying and selling sex, condom use, social support, and access to and utilization of HIV related services.
Data were directly entered into a database as participants responded to the online questionnaire. Data were monitored by an information technology manager as well as the survey coordinator and an international consultant. Data were formatted and coded in Microsoft Excel (version 14.0; Microsoft Corporation) and SPSS (version 23.0; IBM Corporation) before being downloaded into RDS-Analyst (www.hpmrg.org), a specialized software for analysing RDS data. Data were assessed for bottlenecks and convergence and population proportions, and 95% confidence intervals (CI) were derived with RDS-analyst using the Gile successive sampling estimator (8-9) adjusted for differential recruitment and social network sizes. Given that the online survey format resulted in some unreliable social network size responses, social network sizes were imputed with the visibility imputation function in RDS Analyst (10). This survey received ethical approval from the ethics review committee of the National Centre for AIDS/STD Control and Prevention of China CDC.
The survey in Guangzhou recruited 288 MSM aged 15–19 years resulting in 3 recruitment chains with a maximum of 13 waves. In Tianjin, 258 were recruited resulting in 5 recruitment chains and a maximum of 9 waves (Figure 1A and Figure 1B, highlighted by age groups). The mean age of MSM aged 15–19 years was 17 years old in Guangzhou and 18 years old in Tianjin. Homosexual identity was reported by 32% of MSM aged 15–19 years in Guangzhou and 69% in Tianjin. Most respondents reported that their parents did not know about their sexual attraction to males, and 75% of MSM aged 15–19 years in Guangzhou and more than 94% in Tianjin reported using any MSM online social network app (Table 1).
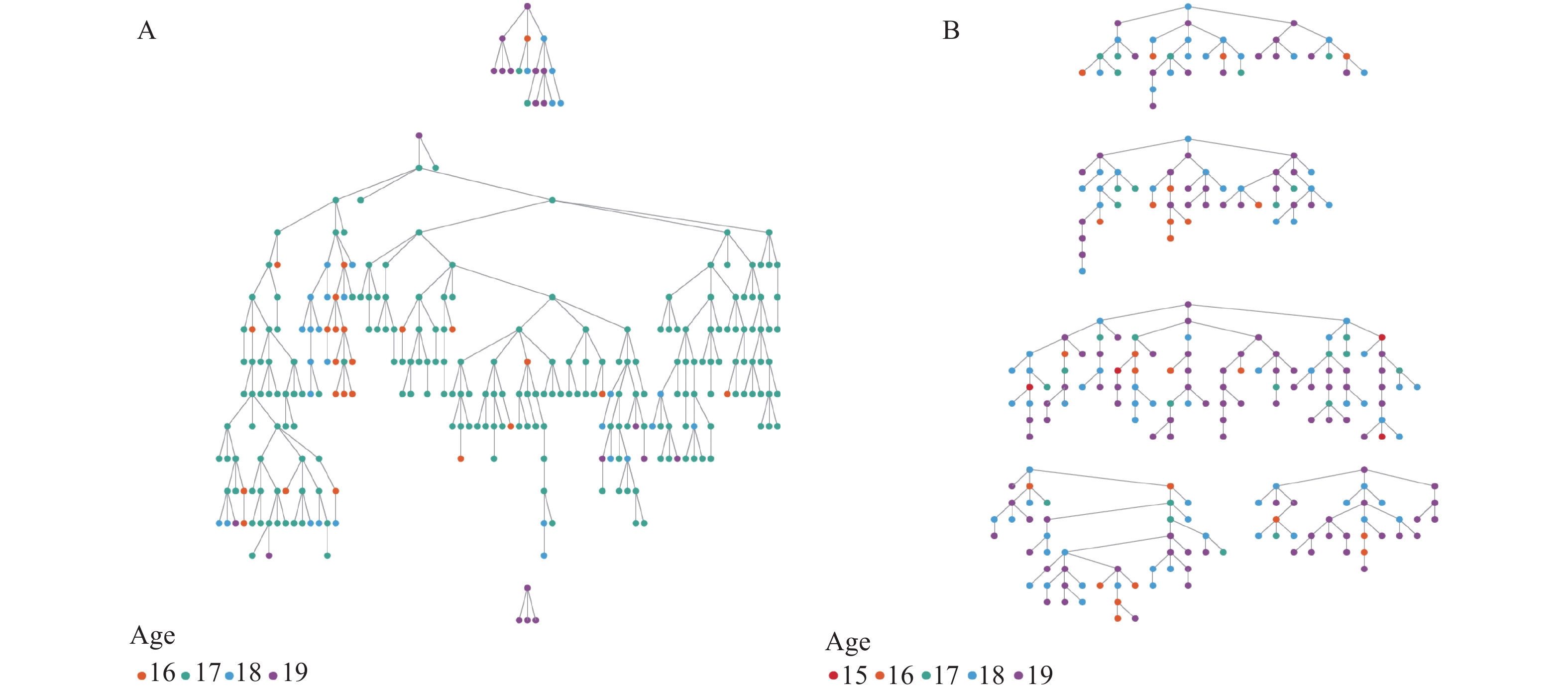 Figure 1.
Figure 1.Recruitment chains of adolescent men who have sex with men (AMSM) sampling in Guangzhou, April−May, 2018 (n=288) (A) and in Tianjin, April−September, 2018 (n=258) (B).
Item Guangzhou (n=288) Tianjin (n=258) N Percentage (CI) N Percentage (CI) Currently in school Yes 270 94.7 (91.9−97.5) 228 83.1 (79.9−94.3) No 18 5.3 (2.5−8.1) 30 12.9 (5.7−20.1) Education level ≤Junior high school 58 19.1 (13.8−24.4) 18 8.0 (2.2−13.9) Senior high/vocational/second 202 71.2 (65.2−77.2) 105 46.0 (35.8−56.2) ≥Vocational college 28 9.6 (5.4−14) 135 46.0 (35.5−56.5) Sexual orientation Gay/homosexual 96 32.1 (25.2−38.9) 173 68.7 (59.2−78.2) Bisexual 59 24.1 (16.8−31.3) 45 18.0 (10.1−25.8) Straight 51 17.2 (11.5−23) 2 2.9 (0−6.6) Unsure 43 17.2 (11.7−22.8) 18 7.2 (2.1−12.4) Other 5 1.8 (0−3.9) 2 0.3 (0−0.7) Do not know 16 7.5 (2.5−12.6) 3 2.9 (0−6.7) Talked about same sex behaviour among circle of friends Yes 143 55.2 (48.2−62.4) 129 57.7 (46.4−68.9) No 121 44.8 (37.6−51.8) 110 42.3 (31.1−53.6) Parents know about sexual attraction to males Yes 101 39.8 (31.4−48.2) 30 11.2 (3.8−18.4) No 163 60.2 (51.8−68.6) 210 88.8 (81.6−96.2) How MSM network was entered Acquaintances outside school 83 28.7 (21.5−25.9) 14 7.3 (3.2−11.5) Classmates 72 25.2 (18.5−32) 34 12.4 (6.9−17.8) From internet 75 28.6 (20.3−36.9) 174 64.2 (55.9−72.5) Other 3 1.9 (0−4.2) 5 2.6 (0−5.7) Can’t remember 45 15.6 (9.6−21.5) 29 13.5 (7.7−19.2) Uses any MSM online social network app Yes 215 74.7 (67.5−81.9) 252 94.3 (88.8−99.9) No 73 25.3 (18.2−32.5) 6 5.7 (0.1−11.2) Table 1. Sociodemographic characteristics and communication factors of adolescent men who have sex with men (AMSM) in Guangzhou City and Tianjin Municipality, 2018.
The age group with the highest percentage for first anal sexual experience was 16 years old in Guangzhou and 18 years old in Tianjin. Most MSM aged 15–19 years in the 2 cities reported having had an anal sexual experience in the past 6 months, with over half having multiple sex partners. One third of respondents in both cities who reported having anal sex were primarily receptive partners. Forty-two percent of AMSM in Guangzhou and 9% of AMSM in Tianjin reported experience of selling sex. Among them 56% and 54% reported having consistent condom use respectively. Among MSM aged 15–19 years who ever used a condom, the age at first condom use during an anal sexual experience most frequently reported was 16 years in Guangzhou and 18 years in Tianjin. An estimated 61% of AMSM in Guangzhou and 43 % in Tianjin reported using any drug before anal sex with a male. Although as much as 65% of MSM aged 15–19 years in Guangzhou and 93% in Tianjin knew that the proper use of condoms during each sexual intercourse reduces the risk of HIV transmission, only 26% of MSM aged 15–19 years in Guangzhou and 12% in Tianjin knew that a healthy-looking person can have HIV, and only 27% of AMSM in Guangzhou and 25% in Tianjin knew that having sex with one faithful, uninfected partner, reduces the risk of HIV transmission. Percentages of MSM aged 15–19 years in Tianjin who were aware of anti-retroviral therapy and self-testing for HIV were 91.6% and 85.6%, respectively, whereas in Guangzhou the awareness rates of anti-retroviral therapy and HIV self testing were 59.5% and 45.8%, respectively. The percentages of MSM aged 15–19 years reporting ever having a HIV test were 46.9% in Guangzhou and 79.4% in Tianjin. Self-reported positive results of HIV was 17.6% in Guangzhou and 2.1% in Tianjin (Table 2).
Item Guangzhou (n=288) Tianjin (n=258) N Percentage (CI) N Percentage (CI) Age at first anal sexual experience ≤12 years 18 6.1 (3.1−9.1) 4 3.0 (0−7.2) 13 years 10 2.6 (0.6−4.8) 8 1.4 (0−3.0) 14 years 25 9.9 (5.7−14.1) 7 3.9 (0.5−7.3) 15 years 44 16.5 (10.9−22.1) 30 7.3 (2.5−19.5) 16 years 63 22.1 (16−28.1) 39 12.6 (5.7−17.8) 17 years 49 21.2 (14.9−27.5) 40 11.4 (5.0−17.8) 18 years 28 10.1 (5.8−14.3) 62 30.2 (20.1−40.4) 19 years 6 2 (0.3−3.6) 29 11.0 (4.5−18.7) Do not remember 25 9.6 (5.5−13.6) 25 18.5 (9.9−27.2) Age at first use of condom during anal sexual experience ≤12 years 10 3.5 (0.4−6.6) 2 2.3 (0−7.8) 13 years 8 3.0 (0−6.3) 4 1.2 (0−3.5) 14 years 16 9.1 (3.0−15.2) 7 3.1 (0.2−6.1) 15 years 39 20.4 (10.2−30.5) 17 4.6 (1.4−7.8) 16 years 68 28.5 (20.0−37.0) 32 16.0 (8.8−23.1) 17 years 53 19.4 (11.6−27.1) 38 12.8 (7.8−17.8) 18 years 33 12.6 (5.5−19.7) 57 31.6 (23.7−39.6) 19 years 12 3.5 (0−7.0) 53 28.3 (20.4−36.2) Anal sexual experience in the past 6 months Yes 211 78.6 (73.1−84) 233 91.0 (84.4−97.5) No 59 21.4 (16.0−26.8) 11 9.0 (2.5−15.6) Number of anal sex partners (among those who had anal sex in past 6 months) 1 102 48.2 (39.5−56.9) 87 42.8 (30.2−55.3) 2–5 58 25.7 (18.3−33.1) 98 42.4 (31.8−53.1) 6–10 23 11 (5.6−16.4) 37 9.4 (3.4−15.4) 11–20 24 12.8 (7.2−18.3) 7 1.5 (0−3.3) 21 and above 4 2.3 (1.4−3.3) 4 4.0 (0−8.8) Age range of sex partners* in past 6 months Under 20 years 185 68.6 (61.5−75.8) 110 45.5 (35.4−55.6) 20–30 years 53 18.3 (12.3−24.2) 113 47.6 (37.0−58.0) 31–40 years 26 10.1 (6.2−14.1) 9 6.9 (0.9−12.9) 41 years or above 6 2.9 (0.6−5.3) 1 0.1 (0−0.2) Usual role in anal sex experience in past 6 months Insertive 93 40.6 (30.2−50.9) 77 37.4 (26.6−48.4) Receptive 70 33.8 (23.1−44.5) 97 38.0 (27.3 48.7) Insertive and receptive 46 25.6 (17.0−34.2) 54 24.6 (15.2−33.9) Ever paid someone money for sex Yes 117 44.6 (37.0−52.4) 13 5.3 (0.2−10.5) No 148 55.4 (47.7−63) 228 94.7 (89.5−99.8) Frequency of using a condom when paying for sex Every time 74 57.9 (47.0−69.0) 2 29.2 (0−76.2) Sometimes 37 36.5 (25.5−47.4) 7 38.8 (0−76.0) Never 6 5.6 (5.6−5.6) 4 32.0 (0−73.4) Ever received money or other benefit in return for sex Yes 112 41.7 (33.2−50.1) 21 9.4 (2.4−16.4) No 153 58.4 (49.9−66.8) 220 90.6 (83.6−97.6) Frequency of using a condom when selling sex Every time 65 55.5 (39.3−71.7) 10 53.6 (25.8−81.6) Sometimes 40 39 (27.6−50.5) 10 45.1 (17.2−72.8) Never 7 5.5 (0−14.2) 1 1.3 (0.4−2.2) Ever been forced or coerced to have anal sexual experience with a male Yes 116 43.7 (35.0−52.2) 19 8.8 (3.8−13.8) No 148 56.4 (47.7−65.0) 222 91.2 (86.2−96.2) Frequency of condom use when forced to have anal sexual experience Every time 66 58.3 (44.5−72.1) 9 53.5 (26.6−80.5) Sometimes 42 36.5 (23.7−49.4) 3 18.3 (3.8−40.4) Never 8 5.2 (1.2−9.0) 7 28.2 (14.2−42.2) Can always negotiate with a partner to use condoms when wanting to Yes 185 74.9 (67.8−82.1) 212 88.7 (83.3−94.1) No 46 21.4 (15.3−27.5) 17 9.0 (3.8−14.2) Never want to use 9 3.7 (0.2−7.2) 6 2.3 (0−4.7) Used a condom during last anal sexual experience Yes 206 85.3 (78.4−92.2) 143 62.7 (51.1−74.3) No 34 14.7 (7.8−21.6) 93 37.3 (25.7−48.9) Used any drug before anal sex with a man to enhance sexual experience Yes 160 61.4 (53.6−69.3) 107 42.5 (32.9−52.3) No 105 38.6 (30.7−46.4) 135 57.5 (47.4−67.2) Awareness that a healthy-looking person can have HIV Yes 75 25.7 (19.0−32.4) 33 12.2 (5.3−19.2) No 130 50.4 (42.7−58.2) 184 73.7 (64.6−82.7) Do not know 65 23.9 (19.0−30.8) 27 14.1 (6.9−21.4) Awareness that having sex with one faithful-uninfected partner reduces the risk of HIV transmission Yes 94 26.6 (26.7−39.2) 45 25.3 (15.8−34.7) No 101 37.8 (30.3−45.3) 178 65.3 (55.0−75.7) Do not know 75 29.3 (21.7−36.9) 21 9.4 (3.3−15.4) Awareness that proper use of condoms during each sexual experience reduces the risk of HIV transmission Yes 180 65.3 (57.8−72.7) 231 93.4 (88.1−98.6) No 51 20.9 (15.5−26.2) 8 3.4 (0−7.0) Do not know 39 13.9 (7.4−20.3) 5 3.2 (0−6.9) Aware of anti-retroviral therapy Yes 167 59.5 (51.3−67.6) 216 91.6 (86.3−96.8) No 103 40.5 (32.4−48.7) 28 8.5 (3.2−13.7) Aware of a test to take by oneself to test for HIV Yes 128 45.8 (37.1−54.5) 201 85.6 (78.5−92.6) No 142 54.2 (45.5−62.9) 43 14.4 (7.4−21.5) Ever tested for HIV Yes 123 46.9 (37.4−56.2) 198 79.4 (70.5−88.3) No 141 53.2 (43.8−62.6) 47 20.7 (11.7−29.5) Result of last test (among those who ever had an HIV test) Negative 78 59.7 (45.7−73.6) 183 84.1 (76.8−91.3) Positive 22 17.6 (9.8−25.3) 4 2.1 (0−5.5) Do not know results 23 22.8 (11.6−33.9) 11 8.3 (0.3−16.4) Self-perceived level of HIV infection risk No risk 51 18.8 (13.4−24.1) 43 18.6 (9.4−27.9) Some risk 116 47.9 (41.3−54.6) 91 36.3 (26.3−46.2) High risk 63 25.2 (18.5−31.9) 75 30.9 (19.9−41.9) Do not know 0 − 17 8.3 (1.9−14.7) * Type of sex is not defined; sex of partner not defined; question asks about multiple partners whose ages may not be in the same range. Table 2. HIV-related knowledge/awareness and behaviours among adolescent men who have sex with men (AMSM) in Guangzhou City and Tianjin Municipality, 2018.
HTML
-
This survey found that AMSM have many intersecting risks including high percentage of inconsistent condom use during anal sex, of early sexual initiation, of recreational drug use, and use of sexual enhancement drugs that are likely leading to unprotected sex or sex with multiple partners. They also have high rates of self-reported HIV infection.
These findings strongly indicated that education on STI/HIV prevention and on risks of drug use must begin at younger ages. Educators in school settings must be trained on and sensitized to the specific needs for knowledge of and services for AMSM and other key adolescent populations to provide early and targeted interventions in response to the high prevalence of risky sex and substance abuse. Both AMSM and service providers should be informed about the actual age of consent of 16 years for independent testing, to encourage more adolecents at high risk of HIV to get tested and receive counselling. In addition, utilization of self-testing should be explored for AMSM.
Because AMSM have large social networks and rely on peers for information, more activities should be explored on how to use the highly active social networks and peer communications to improve AMSM’s knowledge and access to services. Creative technology-based interventions should be enhanced to leverage social media to expand and improve connections with AMSM, to better understand their behaviors, to more effectively disseminate knowledge on HIV prevention, counselling, and testing, and to improve access to services.
This survey had some limitations. Although recruitment through peers using WeChat was effective, the reporting of accurate network sizes could not be verified. Some variables had small values, which resulted in wide confidence intervals that limited the ability to derive accurate estimates. However, this is the first use of online RDS among AMSM in China and provides essential information about their behaviors and needs. Additional surveys using online techniques should be conducted in other cities to gain a more expanded epidemiological picture of AMSM in China.
Acknowledgments: We would like to show our gratitude to Haichao Zhang and Lingping Cai of Beijing Kangzhong Health Education and Service Centre for the design and management of the online system for this web-based survey, and we thank Liqiu Wang, an independent researcher and programme specialist, and Peng Liu of the Chinese Association for STD/AIDS Prevention and Control for their insight and technical advice. We are immensely grateful to UNICEF China and UNICEF East Asia and Pacific Regional Office for their generous funding support and technical advice, and to the Global AIDS Programme (GAP), United States CDC, China Office for their technical expertise around this subject matter.
| Citation: |



 Download:
Download:




