-
China is facing a rapidly increasing trend in hypertension prevalence with excessive sodium intake (1). Among Chinese adults, the main source of dietary sodium is cooking salt as a condiment (2). Data collected in the China Health and Nutrition Survey (CHNS) from 1991 to 2018 was used to observe trends in cooking salt intake among adults aged 18 years and above. Median cooking salt intake was found to decrease from 12.0 grams per day (g/d) in 1991 to 6.3 g/d in 2018. Through public health initiatives addressing the excessive cooking salt intake, overall population consumption of cooking salt has decreased, but challenges still exist for much higher consumption of sodium.
A national representative survey in 2012−2015 indicated that 23.2% of Chinese adults (≈244.5 million individuals) had hypertension (3), and strong evidence has shown that excessive salt intake is one of the most important etiological factors for hypertension and the onset of cardiovascular diseases (CVD) (4-5). The World Health Organization (WHO) has recognized salt reduction as one of the most cost effective and feasible approaches to prevent non-communicable diseases (NCDs) (6), and the Healthy China Action Plan for 2019−2030 has recommended consuming salt less than 5 g/d. Action groups and initiatives have been established to help China’s population reach this target, and consistent monitoring of the situation is crucial for providing data on the effectiveness of salt-reduction interventions and for further policy development.
This study used data from the CHNS, which was an ongoing large-scale, longitudinal, household-based survey conducted from 1989 to 2018. The CHNS used a multistage random-cluster process to draw the sample in nine provinces/autonomous region①. The detailed design and sampling have been reported elsewhere (7). Three megacities (Beijing, Chongqing and Shanghai) were added in 2011, three new provinces (Shaanxi, Yunnan, and Zhejiang) in 2015, and Hebei in 2018. Overall, the CHNS covered 16 provincial-level administrative divisions that varied in demography, geography, economic development and public resources.
The analysis was based on 26,859 individuals in 4 waves of the survey in 1991, 2000, 2009, and 2018 with 8,407, 9,962, 9,644, and 14,619 adults having complete demographic and dietary data, respectively. Each wave of the survey assessed dietary intake using 3 consecutive 24-hour dietary recalls at the individual level in combination with weighing the amount of salt at the household level. Cooking salt in the home inventory and purchased at market were carefully recorded and measured at the start of the first 24-h dietary recall and at the end of the last 24-h dietary recall. The study allocated proportions of cooking salt at the household level to each individual based on the proportion of total energy that he or she consumed. In the study, cooking salt was only the salt added during cooking, not including other condiments like soy sauce or monosodium glutamate.
Nonparametric tests were applied to test differences between groups and waves for cooking salt intake. All statistical analyses were performed using the SAS software package (version 9.2; SAS Institute, Inc. Cary, NC, USA).
Table 1 showed the characteristics of participants from 1991 to 2018. The age distribution showed that the population had aged over time. The gender and area composition remained approximately similar. There were more participants living in the south than in the north. Median cooking salt intake decreased from 12.0 g/d in 1991 to 6.3 g/d in 2018 (Table 2 and Figure 1). Cooking salt intake was generally higher for younger age groups than the oldest age group, for men than for women, and for rural than for urban residents. In 1991, cooking salt intake was higher in Northern China (12.4 g/d) than in Southern China (11.9 g/d),② while in 2018, cooking salt intake was higher in Southern China (6.4 g/d) than in Northern China (6.2 g/d).
Items 1991 2000 2009 2018 No. of subjects 8,407 9,962 9,644 14,619 Age 18−44 5,306 (63.1) 5,214 (52.3) 3,674 (38.1) 4,091 (28.0) 45−59 1,841 (21.9) 2,874 (28.9) 3,364 (34.9) 4,888 (33.4) ≥60 1,260 (15.0) 1874 (18.8) 2,606 (27.0) 5,640 (38.6) Gender Male 3,964 (47.2) 4,812 (48.3) 4,614 (47.8) 6,738 (46.1) Female 4,443 (52.8) 5,150 (51.7) 5,030 (52.2) 7,881 (53.9) Area Urban 2,904 (34.5) 3,152 (31.6) 3,008 (31.2) 4,984 (34.1) Rural 5,503 (65.5) 6,810 (68.4) 6,636 (68.8) 9,635 (65.9) Region North 3,031 (36.0) 4,280 (43.0) 4,127 (42.8) 5,664 (38.7) South 5,376 (64.0) 5,682 (57.0) 5,517 (57.2) 8,955 (61.3) Table 1. Characteristics of participants of the China Health and Nutrition Survey, 1991−2018.
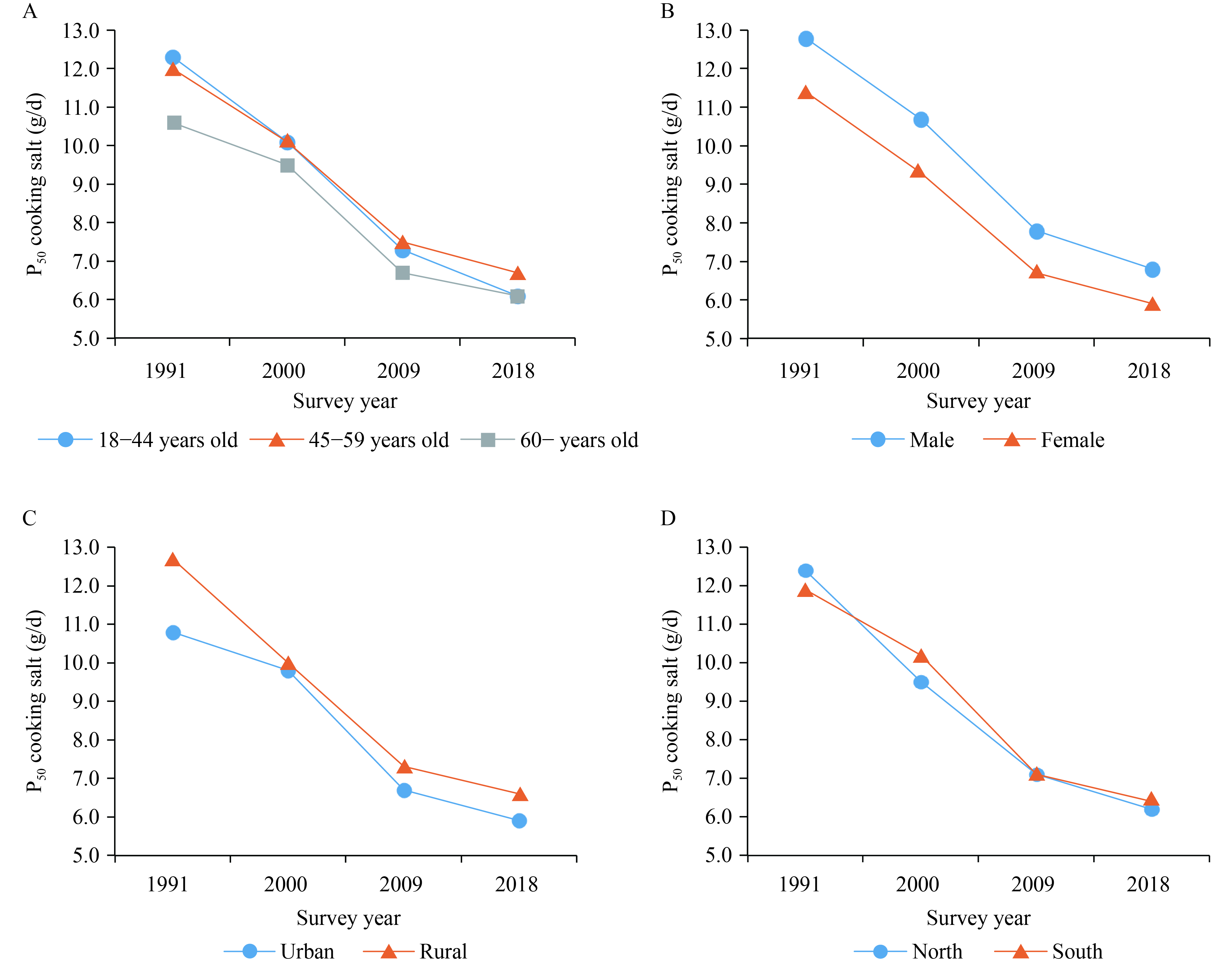 Figure 1.
Figure 1.Trends in cooking salt intake among surveyed adults in subgroups from 1991 to 2018. (A) Trends in cooking salt intake among adults in age groups. (B) Trends in cooking salt intake among adults in gender groups. (C) Trends in cooking salt intake among adults in area groups. (D) Trends in cooking salt intake among adults in region groups.
Items 1991 2000 2009 2018 Median (P25, P75) Median (P25, P75) Median (P25, P75) Median (P25, P75) All† 12.0 (7.4, 17.6) 10.0 (6.8, 14.8) 7.1 (4.8, 10.2) 6.3 (3.8, 9.8) Age 18−44 12.3 (7.6, 18.0)† 10.1 (6.7, 14.8)* 7.3 (4.9, 10.2)† 6.1 (3.6, 9.8)† 45−59† 12.0 (7.7, 17.8) 10.1 (7.1, 15.0) 7.5 (5.0, 10.7) 6.7 (4.1, 10.2) ≥60† 10.6 (6.0, 16.5) 9.5 (6.7, 14.6) 6.7 (4.5, 10.0) 6.1 (3.8, 9.5) Gender Male† 12.8 (8.0, 18.8) 10.7 (7.4, 15.7) 7.8 (5.3, 11.0) 6.8 (4.1, 10.4) Female† 11.4 (7.0, 16.7) 9.3 (6.4, 13.9) 6.7 (4.5, 9.6) 5.9 (3.6, 9.2) Area Urban 10.8 (6.6, 16.4)† 9.8 (6.7, 14.5)* 6.7 (4.4, 9.7)† 5.9 (3.6, 9.0)† Rural† 12.7 (8.0, 18.2) 10.0 (6.9, 15.0) 7.3 (5.0, 10.5) 6.6 (4.0, 10.2) Region North 12.4 (7.3, 18.8)† 9.5 (6.1, 14.9)† 7.1 (4.6, 10.3) 6.2 (3.8, 9.7)* South† 11.9 (7.5, 16.9) 10.2 (7.4, 14.8) 7.1 (4.9, 10.2) 6.4 (3.8, 10.0) Note: Wilcoxon test was used for two groups. Kruskal-Wallis test was used for more groups and waves.
* p<0.05.
† p<0.001.Table 2. Trends in cooking salt intake among adults of the China Health and Nutrition Survey, 1991−2018 (g/d).
HTML
-
In order to reduce blood pressure and the risk of cardiovascular disease, stroke, and coronary heart disease in adults, the WHO recommends that all adults reduce their sodium intake to <2,000 mg/d (8). In China, sodium in the diet comes mainly from salt added during cooking (63.6%) (2). Therefore, public health initiatives are needed to reduce the amount of cooking salt.
The trend of decreased cooking salt intake was seen from 1991 to 2018 among Chinese adults. This could be attributable to the national campaigns focusing on salt reduction. For example, the Chinese Ministry of Health and the Shandong government collaboratively launched the Shandong-Ministry of Health Action on Salt Reduction and Hypertension (SMASH), 2011–2015, the goal of which was to reduce daily salt intake and increase awareness and control of hypertension among adults (9). The China Healthy Lifestyle for All (CHLA) campaign, which was launched in 2007, set salt reduction as a key component of its second stage. The campaign widely disseminated multiple messages regarding the effect of salt on health and the methods of limiting salt intake. Regionally, in some cities like Beijing and Shanghai, the governments distributed free salt spoons to families to encourage restricting the amount of salt added during cooking and food preparation (10).
Another possible explanation for the decreased trend is the changing environment associated with eating behaviors. One of these is less reliance on salty and pickled foods because of modern agricultural technologies, fresh food transportation, and the widespread use of refrigerators (11). Because of Northern China’s historical reliance on these pickled foods, these afore mentioned factors may also explain why cooking salt intake has decreased faster in the north than in the south and why the north–south gap is closing. Increased usage of salt-containing condiments such as soy sauce is another possible reason for the decrease in cooking salt. At the same time, there are rising trends of eating out-of-home and eating packaged foods. All this has come with the very rapid modernization of the restaurant and packaged food manufacturing and retail sectors (12). A study in Beijing indicated that 39.5% of dietary salt was consumed at cafeterias or restaurants in 2011 (13), so assessing and reducing salt used at restaurants and in packaged foods is a growing focus of salt reduction.
It is encouraging to see that cooking salt intake among adults decreased over time. However, cooking salt is only one source of sodium, and sodium intake in China is still among the highest in the world (14). A recent study showed that median sodium intake in adults was 3,960 mg/d in 2015, equivalent to 10 g/d of total salt, which far exceeded recommendations of the WHO (<5 g/d of salt) (2). Recently, the Healthy China Promotion Committee issued the Healthy China Action (2019−2030) at the national level, which established a target salt intake of less than 5 g/d by 2030. Moreover, an action group called Action on Salt China (ASC) has been set up to develop and implement an evidence-based, comprehensive, effective, and sustainable national salt reduction program to help achieve WHO’s recommended salt intake in China (15).
This study is subject to at least three limitations. First is the lack of nationally representative results, even though the survey captured different demographic and geographic areas. Second, the study did not analyze factors such as lifestyle habits that may affect the trends. Third, the study may underestimate cooking salt intake because of the assessing method used. Despite these limitations, to the best of our knowledge, this is the first study to report the most recent cooking salt intake and trends for the past three decades based on a large sample.
In conclusion, cooking salt has decreased among Chinese adults from 1991 to 2018. Despite a decline, effective policies and interventions need to be sustained and intensified to lower cooking salt intake, thus achieving the recommended level of sodium intake. Monitoring sodium consumption at the population level is necessary, which could provide essential information to policymakers and all interestedstakeholders.
-
The authors are grateful to the participants and investigators for their involvement in the survey. The authors also thank the team at National Institute for Nutrition and Health, Chinese Center for Disease Control and Prevention, and the Carolina Population Center, University of North Carolina at Chapel Hill.
FootNote
| ① | From northeast to southwest: Heilongjiang, Liaoning, Jiangsu, Shandong, Henan, Hubei, Hunan, Guizhou and Guangxi. |
| ② | The division between China’s North and South is historically a line running along the Qinling Mountains and the Huaihe River. |
| Citation: |



 Download:
Download:




