-
Alveolar echinococcosis (AE) is a potentially lethal, zoonotic, parasitic disease caused by the larvae of Echinococcus multilocularis (E. multilocularis) and is designated by the WHO as neglected tropical disease. To comprehensively understand the prevalence and scope of AE in China, China CDC organized the relevant provincial and county-level centers for disease control and prevention to conduct the epidemiological survey on echinococcosis in 409 counties in 9 provincial-level administrative divisions from 2012 to 2016. In total, 1,208,944 people were examined by B-ultrasonography and estimated an overall prevalence in the population of the 6 provincial-level administrative divisions to be 0.27% (95% CI①: 0.25%−0.30%). Using results from this survey, a national plan to address echinococcosis has been formulated, and all detected cases during this study were treated with drugs or surgery. In addition, counties where AE was detected carried out deworming for dogs and wild animals, rat extermination around villages, and large-scale health education initiatives.
The E. multilocularis life cycle takes place primarily between wild canids (e.g. foxes, wolves, dogs, etc.) as definitive hosts and their prey (e.g. rodents) as intermediate hosts. Humans can become accidentally infected while consuming parasite eggs that are excreted in the feces of the definitive hosts, but otherwise does not transmit infections as part of the natural cycle. AE can infect the liver in humans and resemble a cancer-like malignant growth and is primarily endemic in the northern hemisphere including Asia, Europe, and North America. The resulting growth in the liver is characterized by slow development of metacestode stage and a prolonged duration of infection. Early stages are often absent of noticeable symptoms, but if left untreated, AE may lead to death in 90% of cases within 10−15 years of diagnosis (1).
AE cases have been reported continuously by hospitals in Western China. However, AE endemic areas in Western China, especially Qinghai-Tibet Plateau, often have cases that have not been diagnosed and reported to hospitals, potentially due to factors such as poor economic conditions, inconvenient transportation, and poor access to health services. In addition, undiagnosed cases frequently result in fatal outcomes, so reported hospital cases alone have difficulty capturing the full situation of the epidemic in China.
With the support of the National Health Commission of the People’s Republic of China, China CDC organized the relevant provincial and county-level CDCs to conduct an epidemiological survey on echinococcosis from 2012 to 2016. Based on the conditions for transmission of echinococcosis in each county and the presence of reported cases of local echinococcosis infection in the Infectious Disease Reporting System of the China CDC, China CDC determined that 409 counties in 9 provincial-level administrative divisions across the country would be investigated.
A stratified and proportionate sampling method was adopted. In the criteria-meeting counties of Sichuan, Gansu, Qinghai provinces, and Xinjiang, Ningxia, and Tibet autonomous regions, all villages were classified by the mode of production of their local residents into four categories.② The number of villages, sampled randomly in each layer, was determined based on the proportion of the population in each layer of the county’s population,③ and 16 villages were sampled in each county.④
An investigation team composed of epidemiologists and B-ultrasound doctors conducted B-ultrasound screening on survey subjects, recorded basic information for each subject and lesion information for each case, and then diagnosed and classified cases according to China’s “Diagnostic Criteria for Echinococcosis” (WS 257–2006). Before the field survey, all investigators involved in the survey were trained for B-ultrasonography diagnosis and the use of Epi Info software. The same survey plan was used in each county, and all the cases diagnosed in the field survey were reviewed by B-ultrasonography experts at the provincial level.
The positive rate of AE in humans was defined as the number of diagnosed patients out of the total number of people examined. The prevalence of the population was calculated according to the following equation:
$$ p = \sum\limits_{j = 1} {\frac{{njwj}}{{Nj}}} = \sum\limits_{j = 1} {pjwj} $$ where “p” is the prevalence of the population in the surveyed area, “n” is the number of cases detected in this layer, “N” is the total number of surveyed people in this layer, “j” is the rank of stratification, and “w” is the weight of the stratification (the proportion of the population in the layer to the total population of the region). All data were inputted using double entry in the Epi Info 3.5.4 (US CDC) database, with error correction using double-entry comparison. Statistical analysis was processed using SPSS 21.0 (IBM, New York, USA).
From 2012 to 2016, 1,208,944 people were examined by B-ultrasonography in 409 counties among 9 provincial-level administrative divisions including Qinghai, Sichuan, Gansu, Yunnan, and Shaanxi provinces, and Ningxia, Xinjiang, Tibet, and Inner Mongolia autonomous regions; 52.39% were male and 47.61% were female. No cases of AE were detected in Inner Mongolia, Yunnan, and Shaanxi. In 99 counties of the remaining 6 provincial-level administrative divisions, 1,243 cases of alveolar echinococcosis were diagnosed.
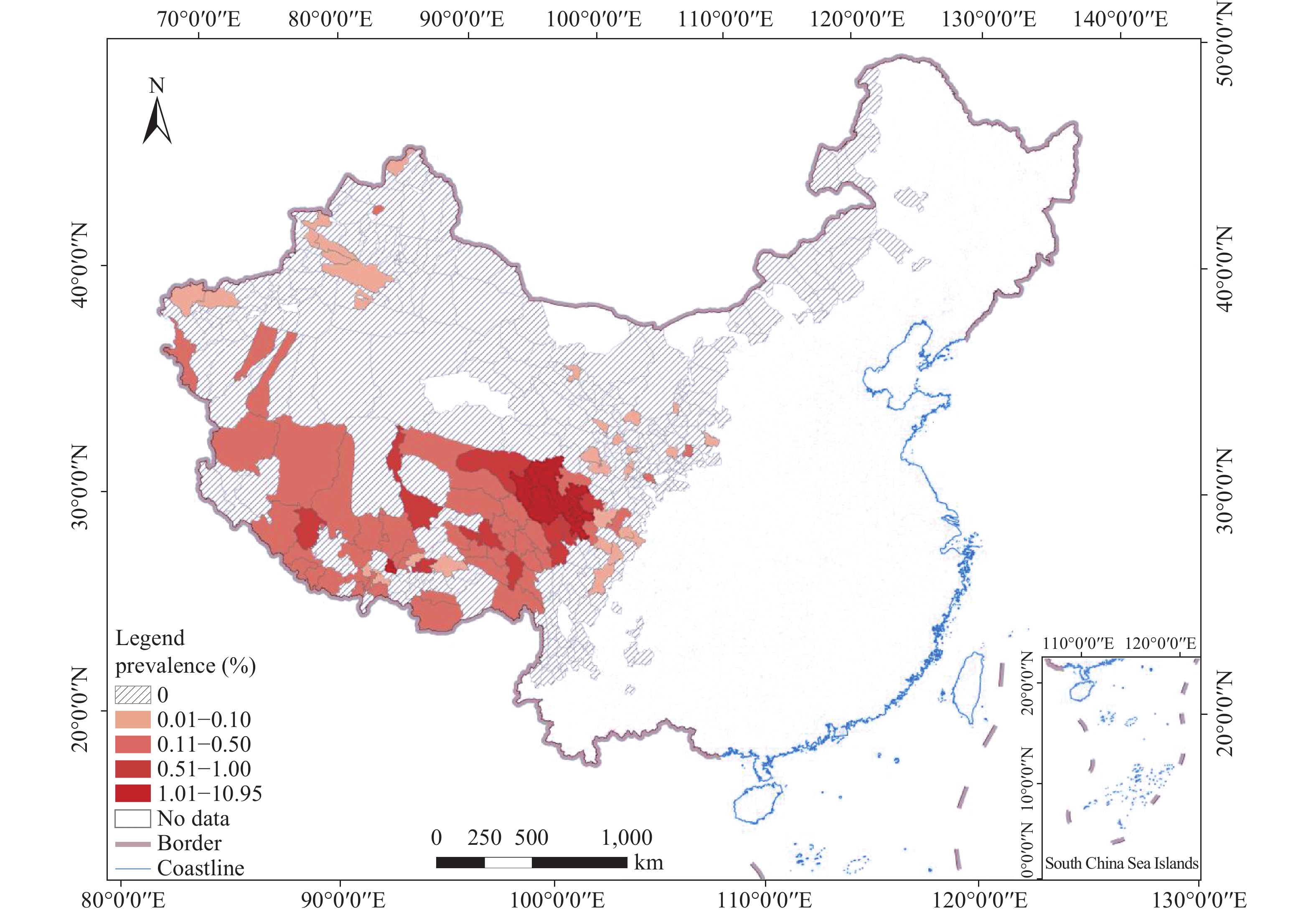
The overall prevalence in the population at risk in 6 endemic provincial-level administrative divisions was 0.27% (95% CI: 0.25%–0.30%), of which the prevalence rate in the population at risk in Qinghai province was the highest 0.73% (95% CI: 0.64%–0.81%). At the county level, the prevalence of 8 counties among 99 AE endemic counties nationwide exceeded 1% and were distributed in Qinghai, Sichuan, and Tibet, and the highest of which was Dari County in Qinghai with a prevalence of 10.95% (95% CI: 9.95%–11.95%) (Figure 1, Table 1).
Province/Autonomous Region County Population at risk Surveyed population Number of cases Prevalence % (95% CI) Qinghai Dari 28,002 3,719 388 10.95(9.95–11.95) Qinghai Chengduo 51,136 2,462 105 5.32(4.43–6.20) Qinghai Maduo 13,780 143 8 5.19(1.56–8.83) Sichuan Siqu 70,100 3,223 150 4.82(4.08–5.56) Qinghai Banma 27,206 2,476 109 3.73(2.98–4.48) Sichuan Seda 44,820 3,202 65 1.87(1.40–2.34) Qinghai Gande 28,815 3,325 42 1.33(0.94–1.72) Tibet Nimu 29,228 853 7 1.04(0.36–1.72) Tibet Baqing 39,416 823 8 0.97(0.30–1.64) Tibet Cuoqin 12,978 824 8 0.97(0.30-1.64) Qinghai Qumalai 27,778 995 11 0.95(0.35–1.55) Sichuan Dege 78,773 3,208 21 0.94(0.60–1.27) Tibet Suoxian 42,398 812 7 0.86(0.23–1.50) Sichuan Ganzi 67,780 3,202 27 0.86(0.54–1.18) Qinghai Jiuzi 24,965 3,242 28 0.86(0.54–1.17) Table 1. Fifteen counties with the highest prevalence of alveolar echinococcosis in China, 2012−2016.
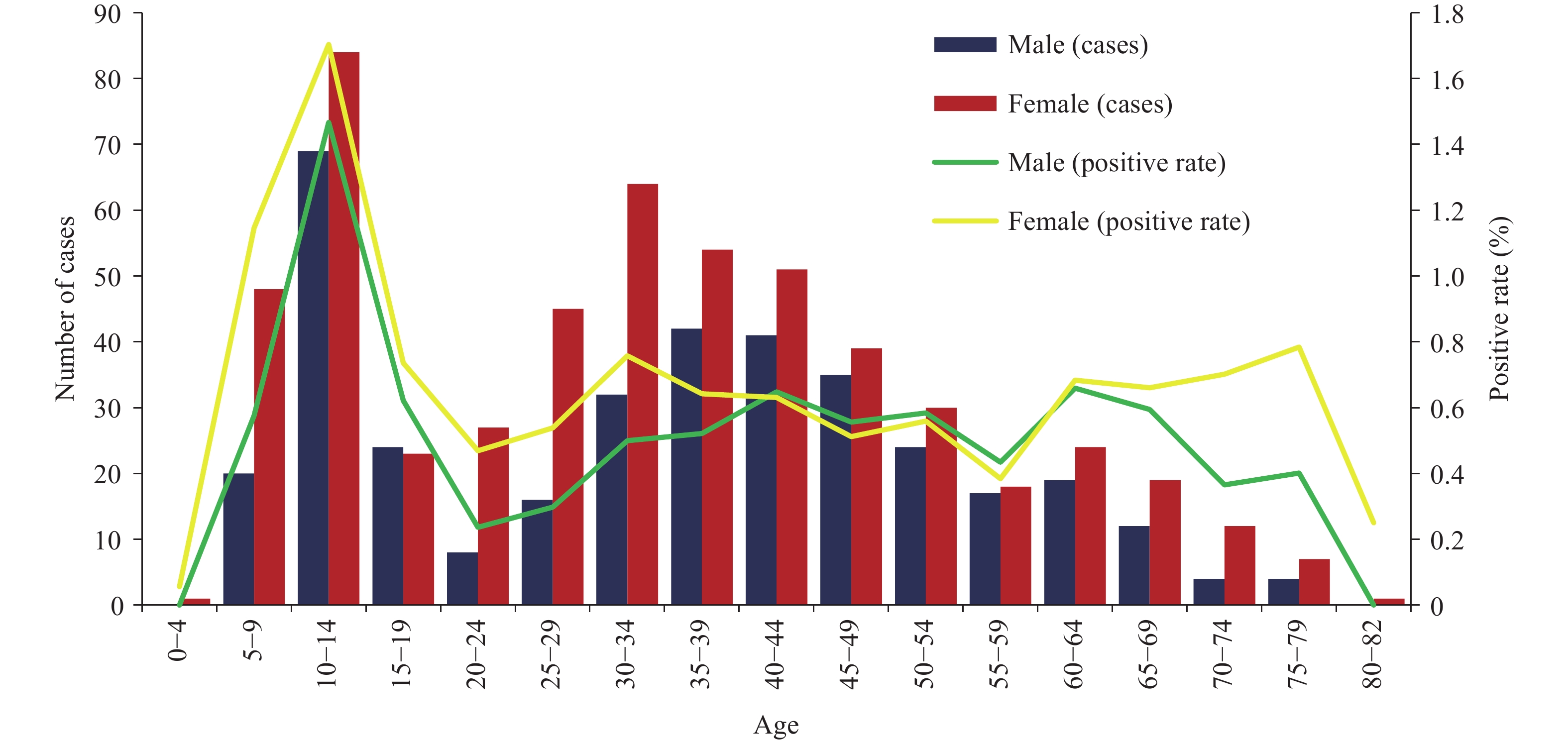
Among 9,007,094 people at risk in 99 AE-endemic counties, 94,687 men and 106,636 women ranging from 1 to 99 years old were examined by B-ultrasonography, of which 524 and 719 cases of AE were diagnosed, respectively. The positive rate of AE among males was 0.55% (524/94,687, 95% CI: 0.51%–0.60%), and lower than that among females, 0.67% (719/106,636, 95% CI: 0.63%–0.72%), and the difference in positive rate between men and women was statistically significant (χ2 person = 11.71, p<0.01). The youngest case of AE was 3 years old, and the oldest was 82 years old. Among both male and female groups, the positive rate was highest in the 10–14 age group with a positive rate of 1.47% (95% CI: 1.15%–1.78%) among males and 1.70% (95% CI: 1.35%–2.06%) among females. From age groups ranged 20 to 79, the positive rate of the population remained at about 0.5% without significant changes, but the rate drops sharply for age groups over 80 years old (Figure 2).
Among the 8 occupational groups, the highest positive rate of AE was found among monks (2.09%; 95% CI: 1.34%–2.58%), followed by herdsmen (1.36%; 95% CI: 1.26%–1.45%) and students (1.36%; 95% CI: 1.19%–1.53%) (Table 2). The positive rates across different occupational groups showed statistical significance (χ2 person = 1195.62, p<0.001). Among different educational level groups, the positive rate of AE among illiterate people was the highest (0.90%; 95% CI: 0.83%–0.97%). As education increases, the positive rate has a downward trend (χ2 Linear-by-Linear Association = 194.85, p<0.001).
Surveyed population No. of cases Proportion % Positive rate % (95% CI) Gender Male 94,687 524 42.16 0.55(0.51–0.60) Female 106,636 719 57.84 0.67(0.63–0.72) Occupations Herdsmen 56,176 762 62.15 1.36(1.26–1.45) Farmers/herdsmen 14,679 53 4.32 0.36(0.26–0.46) Monks 1,385 29 2.37 2.09(1.34–2.58) Students 17,600 240 19.58 1.36(1.19–1.53) House workers 1,819 10 0.82 0.55(0.21–0.89) Public officers 6,195 26 2.12 0.42(0.26–0.58) Farmers 93,995 95 7.75 0.10(0.08–0.12) Others 9,477 11 0.90 0.12(0.05–0.18) Educational level Illiterate 69,485 626 51.06 0.90(0.83–0.97) Elementary school 81,276 532 43.39 0.65(0.60–0.71) Junior high school 32,007 37 3.02 0.12(0.08–0.15) High school 7,098 9 0.73 0.13(0.04–0.21) College and above 5,215 20 1.63 0.38(0.22–0.55) Local residents’ modes of production Pastoral area 62,871 961 78.38 1.53(1.43–1.62) Pastoral and farm area 53,966 120 9.79 0.22(0.18–0.26) Farm area 64,138 61 4.98 0.10(0.07–0.12) Urban area 20,343 84 6.85 0.41(0.32–0.50) Types of residence Settled 159,599 575 46.90 0.36(0.33–0.39) Settled in summer and nomadic in winter 41,581 649 52.94 1.56(1.44–1.68) Others 13,416 174 14.19 1.30(1.11–1.49) Table 2. Positive rates of alveolar echinococcosis among genders, occupations, education levels, and modes of production, and types of residence in China, 2012−2016.
Based on the mode of production of their local residents in western China, the survey regions were divided into pastoral areas, pastoral and farm areas, farm areas, and urban areas, and the positive rate of AE of residents living in different areas showed statistical significance (χ2 person = 1316.46, p<0.001), with the positive rate among people living in pastoral areas being the highest (1.53%; 95% CI: 1.43%–1.62%). Because some herdsmen in the Qinghai-Tibet Plateau need to travel far to pasture and live in tents from May to October every year before returning to their settlement for winter, we compared the prevalence in those people to that of settlers who resided at their settlement for the year. The positive rate among those who were nomadic during the summer and settled in the winter (1.56%; 95% CI: 1.44%–1.68%) was significantly higher than that of settlers (χ2 person = 809.75, p<0.001).
HTML
-
The results of this survey showed that AE was endemic in 99 counties in 6 provincial-level administrative divisions in China including Qinghai, Sichuan, Gansu, Tibet, Xinjiang, and Ningxia. These counties are concentrated in the Qinghai-Tibet Plateau, especially in the border area between Qinghai and Sichuan provinces, as well as the Tibet Autonomous Region where 13 of the 15 counties with the highest prevalence of AE are located. The Qinghai-Tibet Plateau has a large landscape with a wide variety and large population of wild canids, rodents, and other wild animals, and most of the residents are herdsman so the natural transmission cycle of AE is widespread. There are also many domestic and stray dogs in the Qinghai-Tibet Plateau, which can be considered an important source of infection as terminal hosts (2). These natural features may be important determinants for AE in the Qinghai-Tibet Plateau. However, the prevalence at the junctions of the three provincial-level administrative divisions is much higher than that of the other Qinghai-Tibet Plateau regions. For example, residents in areas of Tibet autonomous region that have similar lifestyle habits, modes of production, socioeconomic conditions, and cultural traditions to residents of the junctions have lower prevalence. There may be other factors at work, and further investigation is needed.
In Qinghai, Sichuan, Gansu, Ningxia and other provinces or regions, some sporadic small-scale population surveys of AE conducted in the past showed positive rates varying from 0.2%–10% (3), but these survey results used different methods and choice of survey subjects and have difficulty accurately reflecting the overall AE epidemic situation in China. Following a consistent investigation plan, this survey conducted stratified cluster sampling to examine more than 1.2 million people and showed a 0.27% AE prevalence in 99 counties in 6 provincial-level administrative divisions nationwide. Directly comparing the results of this large population-based sampling survey in China to that of other countries in Europe, Asia, North America, and other regions is difficult because most existing data outside of China are based on hospital reports (4), and only one study, based on the population of Sary Mogol in South Kyrgyzstan (5) which shows the prevalence of AE to be 4.2%(68/1,617), has been found outside China.
Torgerson PR et al. used the previous sporadic survey results in China and the number of cases reported by hospitals in other endemic countries to estimate that the burden of AE in China accounted for more than 91% of the world (6). Applying the calculation method outlined by Torgerson PR et al. to this new survey data, the results still show that China has the most severe AE burden around the world. Apart from the natural factors of the Qinghai-Tibet Plateau, the severity of the AE epidemic in China may be related to poor economic conditions, lack of education in the endemic areas, lack of knowledge on AE, and poor sanitation habits such as insufficient hand washing caused by lack of convenient access to water (7).
For the age distribution of AE, this survey found two distinct, novel characteristics, of which no similar findings have been found in the literature because previous studies in other countries depend on hospital reporting and can only estimate age composition. The first is that the prevalence among children aged 10–14 years is the highest, and the second is that prevalence of the population in the 20–79 age groups is relatively stable. This feature is significantly different from the age distribution of cystic echinococcosis (CE) cases. Population-based surveys in Sichuan, Gansu, Tibet, and other places show that the prevalence of CE increases with age and did not show that the positive rate is higher in the younger age groups (8).
The high prevalence of AE in China in the group aged 10−14 may be related to frequent contact with dogs and poor hand washing habits among young people in the Qinghai-Tibet Plateau. Although the source of AE is generally considered to be predominantly wild canids, some surveys on the Qinghai-Tibet Plateau have shown that dogs have a higher rate of infection with E. multilocularis, indicating frequent contact with dogs is still an important risk factor for children in the region. In comparison to AE, CE has a long course, which can last several decades, and a low mortality rate, so as age increases, cases gradually accumulate and lead to an increase in the prevalence with age. However, AE often has a high mortality rate, which can exceed 90% over 10 years, so the accumulation of cases is less likely. Therefore, the prevalence of people in the age group of 20−79 years is relatively stable.
This survey shows that the prevalence of women is significantly higher than that of men. Surveys in other countries and regions have also shown this result. When reviewing relevant literature, some scholars found that the odds ratio for women was 1.66 (95% CI: 1.31–2.10) (9). This may be a result of women having higher risk of exposure due to taking on more household work, having higher contact with cow dung fuel that may be polluted with worm eggs, and feeding domestic dogs, though a higher biological susceptibility of women to AE should be further investigated.
Most Tibetan residents in the Qinghai-Tibet Plateau region practice Tibetan Buddhism and an important teaching of Buddhism is to not end life, so many stray dogs often gather around the temples to be fed by monks. Therefore, the prevalence of AE among monks is very high in this survey. Herdsmen and illiterate people having higher AE prevalence follows results of surveys in other countries (10) and may be due to the natural cycle of AE being widespread in the grasslands where herdsmen reside, and hygiene practices such as hand washing are poor due to the limitations of the living environment. Similarly, lack of knowledge about the disease is also a risk factor among illiterate people with high prevalence of AE.
This survey was carried out using portable B-ultrasonography in the field. Only abdominal lesions of AE could be found, whereas lesions in the lungs, brain, and other areas outside the abdomen could not be detected. Because the study sampled residents, we cannot exclude the possibility of AE epidemics in other counties of the Qinghai-Tibet Plateau. In Inner Mongolia, Heilongjiang, and Jilin where AE cases have been reported previously, further investigation should be carried out to determine whether they are also endemic areas.
-
This survey is supported by the National Health Commission of the People’s Republic of China and the several provincial and county-level centers for disease control and prevention in Qinghai, Sichuan, Gansu, Shaanxi, and Yunnan provinces, as well as Xinjiang, Tibet, Inner Mongolia, Ningxia autonomous regions. We sincerely thank all the participants involved in this survey and experts who helped develop the investigation plan and analyze data.
FootNote
| ① | CI=Confidence Interval. |
| ② | Pastoral areas (animal husbandry only), semi-pastoral/semi-farm areas (animal husbandry and farming both), farm areas (farming only), and urban areas (live in urban). |
| ③ | For the surveyed villages, if the population of the administrative village was too large, a smaller group of villages within the administrative village was selected as the surveyed area. If the population of the administrative village was too small and could not meet the minimum requirement of 200 people, people from adjacent villages were added as survey subjects. |
| ④ | Due to the small population of some counties in Tibet autonomous region, in counties with a population of more than 100,000, 50,000-100,000, 10,000-50,000, and below 10,000, we selected 16 villages, 8 villages, 4 villages, and 2 villages, respectively. In Yunnan and Shaanxi provinces, 12 villages and 15 villages were sampled in each county by simple random sampling, respectively. |
| Citation: |



 Download:
Download: