-
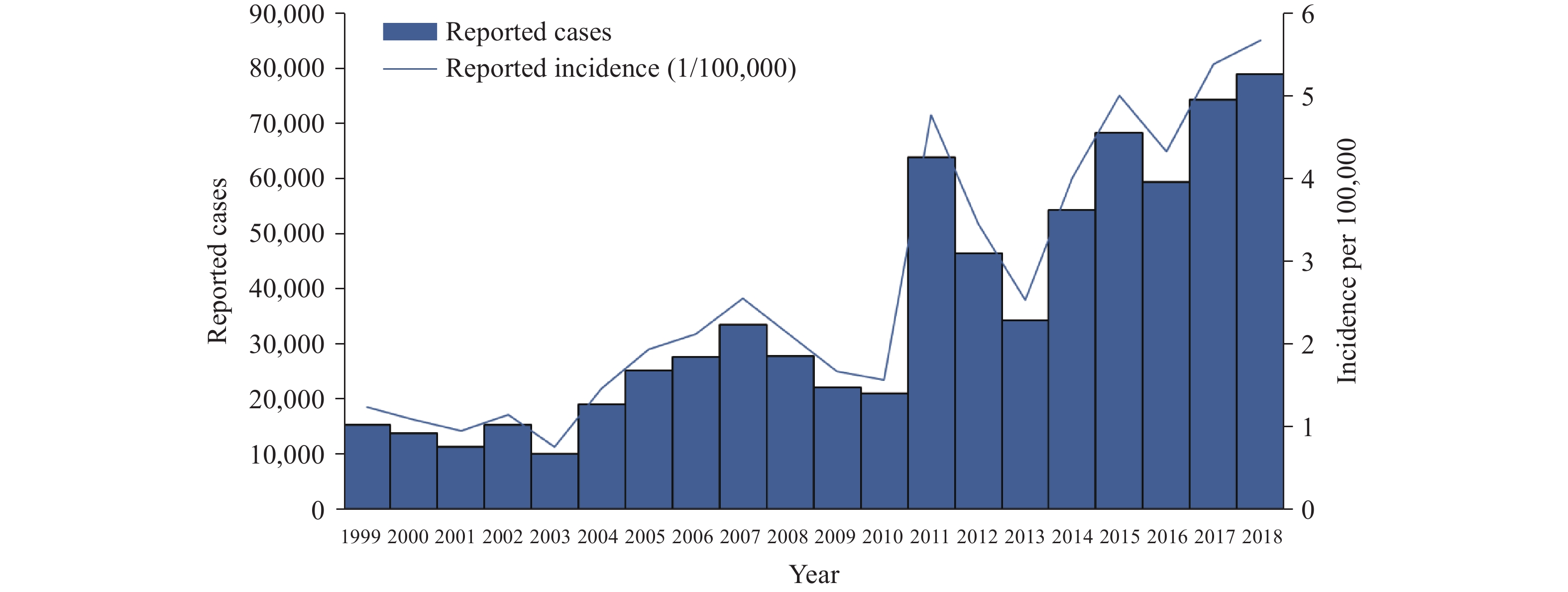
Scarlet fever is a common pediatric respiratory disease caused by Streptococcus pyogenes (Group A Streptococcus; GAS), which can also cause other mild infections such as pharyngitis and impetigo and serious invasive infections including necrotizing fasciitis. The major clinical manifestations of scarlet fever include sore throat, fever, diffuse red rash, and a “strawberry tongue” (1). China CDC affiliated researchers analyzed reported scarlet fever cases from 1999 to 2018 from the National Notifiable Diseases Reporting System (NNDRS) of Mainland China to determine incidence trends. In this period, 720,920 cases were reported with a sudden increase in 2011 and a peak incidence in 2018 of 5.68 cases per 100,000 population, which represents a 2018 total of 78,864 reported cases.
Scarlet fever was considered a fatal disease during 19th and early 20th centuries. The morbidity and mortality of scarlet fever dramatically dropped worldwide when antimicrobial drugs became widely used. Most scarlet fever cases are now diagnosed as mild infections, and fatal infections are now rare. However, a small proportion of cases still may develop serious sequelae.
Since 1950 in China, scarlet fever has been listed as a Type B notifiable disease, which is required to be reported within 24 hours. According to previous analysis (2), the incidence of scarlet fever in China was high between the 1950s and 1980s and then dropped to a low level during the 1990s. In 2011, compared to the baseline level prior to the epidemic, a sudden 2.6-fold increase in the incidence of reported scarlet fever cases was recorded (2). Meanwhile, many other countries also reported significant increases of scarlet fever epidemics worldwide (3-6). The resurgence of scarlet fever has been a concerning public health problem globally.
In early 2019, an emm12 genotype scarlet fever isolate related to UK scarlet fever outbreak strains was detected in Australia through sentinel hospital surveillance (7). The surveillance in China indicates that emm12-type GAS has been predominantly responsible for the scarlet fever resurgence since 2011. All isolates in China are susceptible to β-lactams but are mostly resistant to macrolide antibiotics (2).
Scarlet fever cases reported through the NNDRS of China from 1999 to 2018 were retrieved for analysis (2). Only verified clinic-diagnosed and laboratory-confirmed cases from Mainland China were included in the analysis, excluding Hong Kong, Macao, Taiwan, and foreign residents. Population size data from the China National Bureau of Statistics for denominators were used to calculate incidence rates of scarlet fever. Annual case number and incidence of reported scarlet fever from 1999 to 2018 were analyzed to investigate long term temporal trends. The geographic incidence data and case number were extracted from 1999 to 2018. After a comparison between each year, the incidence data for the year 2010 and 2018 were shown to reflect the variation of geographic incidence before and after the year 2011 when the outbreak started. The age data for scarlet fever incidence were also extracted and shown for the years 2010 and 2018 as representatives before and after the year 2011.
Between 1999 and 2018, there have been three peaks at four-year intervals including 2007, 2011, and 2015. A fourth peak has now been observed in 2018 with 78,864 reported cases and an incidence rate 5.68 per 100,000, which is the highest total over the last 20 years. The incidence increased 5.34% compared to that of 2017 (Table 1, Figure 1). Rare cases of death were reported during 1999 and 2018 (Table 1). The highest number occurred in 1999 with five reported deaths. There was one death in the 2011 epidemic, and in the following years, a total of five deaths were reported. Both 2010 and 2018 data show incidences of northern regions are higher than southern regions. The incidence rate of 2018 significantly increased compared to that of 2010 (t of 2010 (Figure 2). The age group from 5 to 6 years old had the highest incidence for both 2010 and 2018 (Supplementary Figure S1 ).
Year Reported cases Reported incidence (1/100,000 persons) Reported deaths from scarlet fever 1999 15,246 1.23 5 2000 13,720 1.08 3 2001 11,261 0.94 2 2002 15,234 1.14 2 2003 10,063 0.75 1 2004 18,939 1.46 1 2005 25,068 1.93 2 2006 27,620 2.11 0 2007 33,488 2.55 1 2008 27,782 2.10 0 2009 22,068 1.66 0 2010 20,876 1.56 0 2011 63,878 4.76 1 2012 46,459 3.45 2 2013 34,207 2.53 2 2014 54,247 4.00 0 2015 68,249 5.00 1 2016 59,282 4.32 0 2017 74,369 5.39 0 2018 78,864 5.68 0 Table 1. Reported number of cases, incidence rates, and number of deaths caused by scarlet fever per year, 1999−2018 in China.
-
The data reported in this and a previous study (2) indicate the incidence of scarlet fever in China is still increasing, which emphasizes the importance of national scarlet fever alerts. Before 2011 when the epidemic began, the highest number of scarlet fevers occurred in 2007 during the period of 1999 and 2018 (Table 1, Figure 1). Similar epidemic patterns were observed in other East Asian countries including Singapore, and European countries (Germany), where an incidence peak was observed in 2008, prior to the 2011 epidemic surge (4,6). These clues may reflect a similar mechanism attributed to the resurgence of scarlet fever across different parts of the world. The higher incidence of northern regions suggests that more attention should be given to strengthen surveillance in these areas. Active bacterial surveillance on the susceptible populations of age group with highest incidence is necessary.
The reasons underlying the scarlet fever resurgence in China and other countries are still unclear. Several studies have suggested possible reasons for this scarlet fever incidence increase (2,8-9), such as weakened herd immunity, environmental factors, and genetic mutations in the pathogen. Because there is no commercial vaccine for scarlet fever (GAS) prevention (1), natural population immunity may play an important role in the disease epidemic cycle. Further investigations are needed to learn more about the changing immunity patterns in susceptible and resistant populations.
For the current epidemic in Western and Asian countries including China, multiple scarlet fever-causing serotypes and clones have been identified, many of which contain genetic elements carrying streptococcal exotoxins and antimicrobial resistance genes that are widely detected among Asian and European predominant clones. These virulence determinants are thought to play an important role in triggering the epidemic, though further investigations are required (2,10).
The findings in this report are subject to one limitation. The most accurate diagnosis of scarlet fever should be based on pathogen isolation. The majority of reported cases are clinically diagnosed and the proportion of confirmed cases based on pathogen isolation is less than 5%. Thus, the accuracy of surveillance data could be affected by introducing false negative or false positive clinically diagnostic cases.
In summary, China is in a new period of high incidence of scarlet fever. A vaccine is not available for prevention of scarlet fever currently, although advances are being made in GAS vaccine research. Nonetheless, antibiotic treatment is effective. Prevention and control measures for scarlet fever could include identifying cases as early as possible and providing effective antibiotic treatment, controlling cases clusters and dealing with public health events in a timely fashion, and strengthening health education in schools and kindergartens.
The increasing disease burden caused by scarlet fever suggest that health facilities and the public health professionals should pay increasing attention to scarlet fever prevention and control. Medical and health institutions at all level should enhance scarlet fever surveillance. Clinicians should be aware of the increasing trend of scarlet fever incidence in China and undertake early diagnosis and precise treatment with antibiotics. Public health facilities should report suspected cases and detect and control outbreaks in a timely manner. The general public should learn about the knowledge of scarlet fever control and prevention such that if children experience symptoms suspected to be scarlet fever, they should promptly seek a medical diagnosis and treatment.
Scarlet fever GAS pathogen surveillance capabilities should be established where not available, and enhanced if limited to only a few dispersed centers within provinces of China, so as to closely monitor epidemic foci, spread, complications and severe cases, and identify any genetic changes related to bacterial drug resistance, virulence and epidemiology.
-
We thank Dr RJ Simonds from US CDC for his kind help on language editing and providing constructive suggestions.
-
The authors declare no competing interests.
HTML
| Citation: |



 Download:
Download:






