2024 Vol. 6, No. 17
China’s “1-3-7” approach outlines specific targets to guide and monitor the processes of case reporting, investigation, and response. However, few studies have examined the time intervals preceding the initial step, and the timeline from the arrival of imported malaria cases in China to their diagnosis has been largely overlooked.
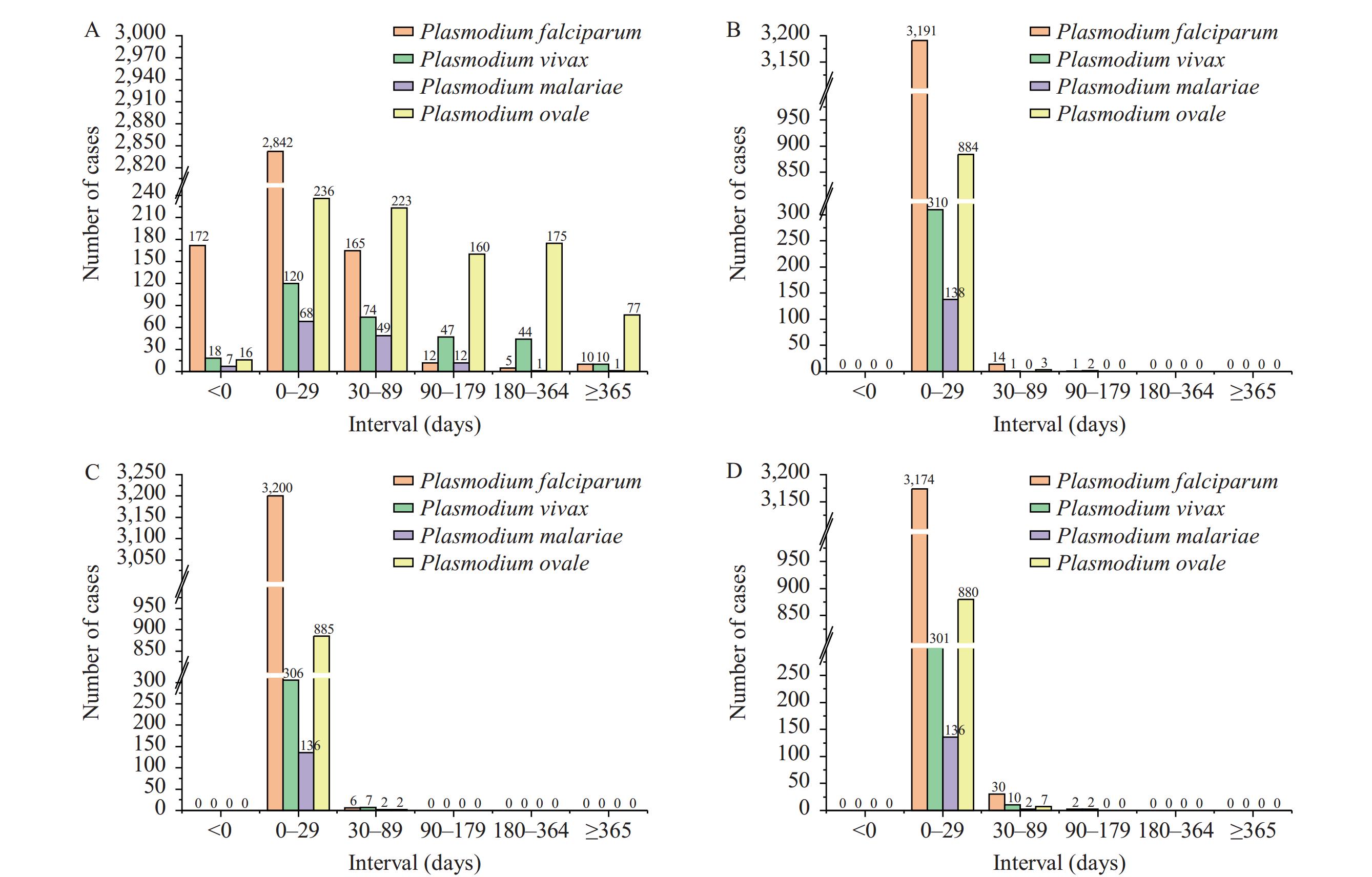
The study demonstrated that the median duration from arrival in China to the onset of symptoms for P. ovale was 78 days, with 71.59% of imported cases manifesting symptoms after more than one month. For P. vivax, the median interval was 42 days, with 55.91% exceeding one month. Additionally, the median time from symptom onset to malaria treatment in China between 2014 and 2021 was 2 days, with an interquartile range (IQR) of 1–4 days.
This study represents the initial effort to delineate the chronology of imported malaria cases, from their arrival in China to their subsequent treatment. The results underscore the importance of providing malaria health education to populations arriving from overseas. Furthermore, enhancing physician training is crucial for improving the diagnosis of malaria.
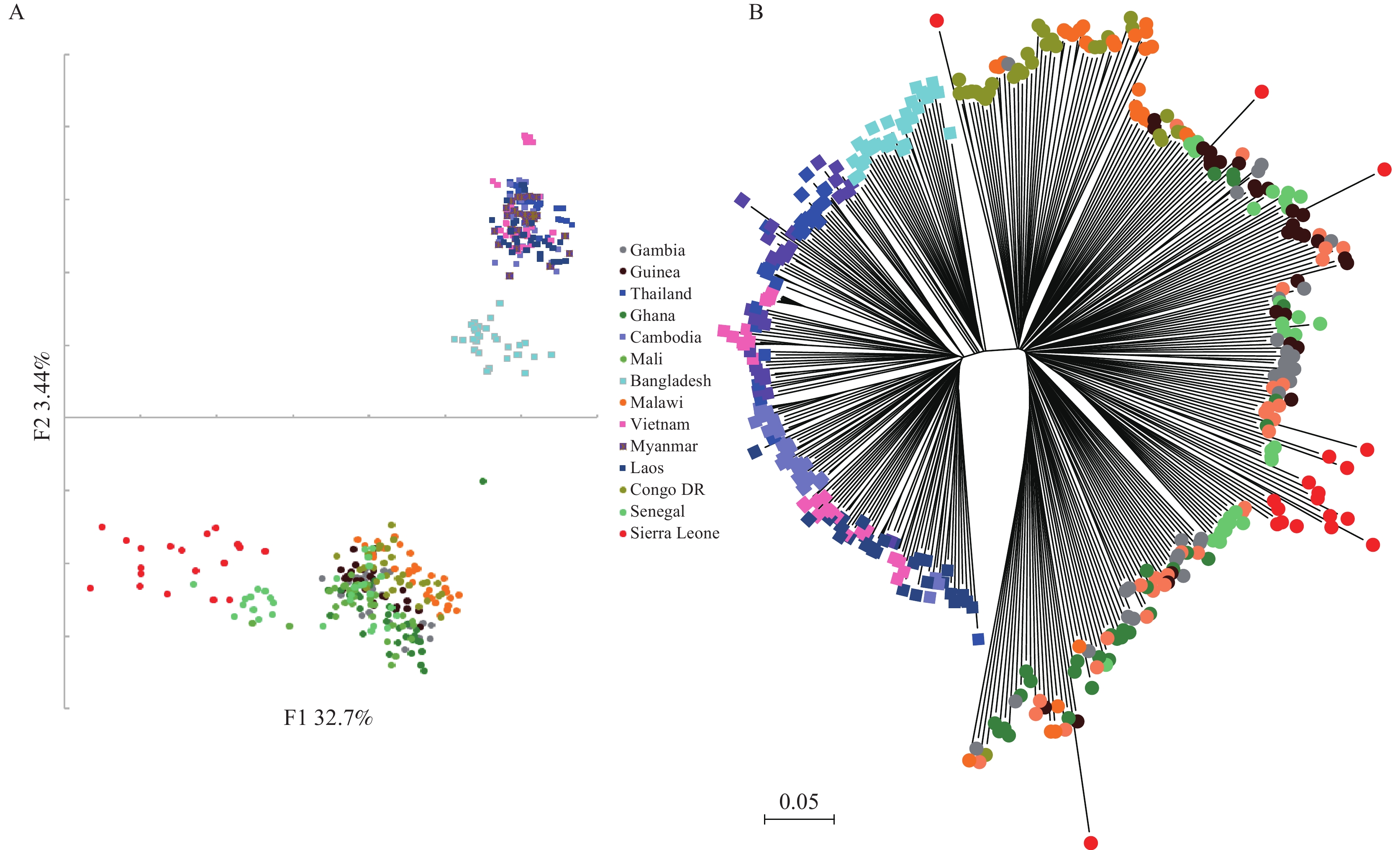
Sierra Leone, with a gross domestic product (GDP) per capita below $300 and significant poverty, ranks among the world’s least developed countries (LDCs). Despite its modest population of 8.6 million, the nation reports approximately 2.6 million malaria cases annually. Previously, there has been no reporting on the malaria genome data from this country.
In this study, we present the first reported whole-genome sequence analysis of 19 high parasite-density Plasmodium falciparum isolates from Sierra Leone, providing insights into the genomic epidemiology of this high-prevalence area. We found a high degree of relatedness among infections and substantial genetic diversity, consistent with the gradual reduction in overall case numbers. Moreover, our whole-genome analysis revealed that, beyond drug-resistance genes, gene families related to blood cell invasion, immune evasion, and others are undergoing directional selection. This suggests that the population in Sierra Leone has developed a relatively strong acquired immunity.
The genomic data not only facilitate the creation of single nucleotide polymorphism barcodes for case tracking but also enable the analysis of evolving transmission dynamics and selection pressures. Additionally, the samples from Sierra Leone exhibited higher selective pressures on resistance genes compared to those from Asia, a trend not commonly observed in other African samples. This suggests that less stringent healthcare systems and inconsistent treatment strategies can subject parasites to increased drug pressure, thereby accelerating the development of resistant strains.
Malaria is a significant public health concern and tropical disease, particularly affecting Myanmar within the Greater Mekong Subregion. The annual parasite index (API) exceeds 1 per 10,000 population in the northern seven townships of Rakhine State, with Minbya Township designated as a high-burden area for malaria by the World Health Organization (WHO) Myanmar and the National Malaria Control Programme (NMCP). Since 2017, the Malaria reduction intensification plan has been in place in this township to combat the high disease transmission rates. This study aims to assess the malaria epidemiology in Minbya Township from 2017 to 2020 under the intensification plan for elimination, as well as to evaluate the effectiveness of the integrated strategy in reducing cases in hotspot areas.
The study utilized a surveillance study design to collect secondary data from the Malaria surveillance system (MSS) and the epidemiologic monitoring dashboard of Minbya Township, Maruk-U District, located in Rakhine State.
Since 2017, the Malaria prevention and control (P&C) Program in Minbya Township has successfully decreased malaria morbidity, eliminated malaria-related deaths, and bolstered malaria testing capabilities through the participation of village health volunteers (VHVs). Approximately 87% of malaria prevention and control services are executed by the township’s malaria elimination and disease control programs, with additional support from stakeholders. The API dropped from 13 in 2017 to 2.5 in 2020, with Plasmodium vivax being the most prevalent malaria species, accounting for 55% of cases.
The study suggests that early diagnosis and promotion of artemisinin-based combination treatment (ACT), along with strategic planning including expanding active case detection in rural health centers and implementing a community-based integrated healthcare approach, are effective and efficient strategies for malaria elimination.
Laiza and nearby areas (LNA) in Myanmar are identified as the primary malaria hotspots in the bordering regions of Yunnan Province, China.
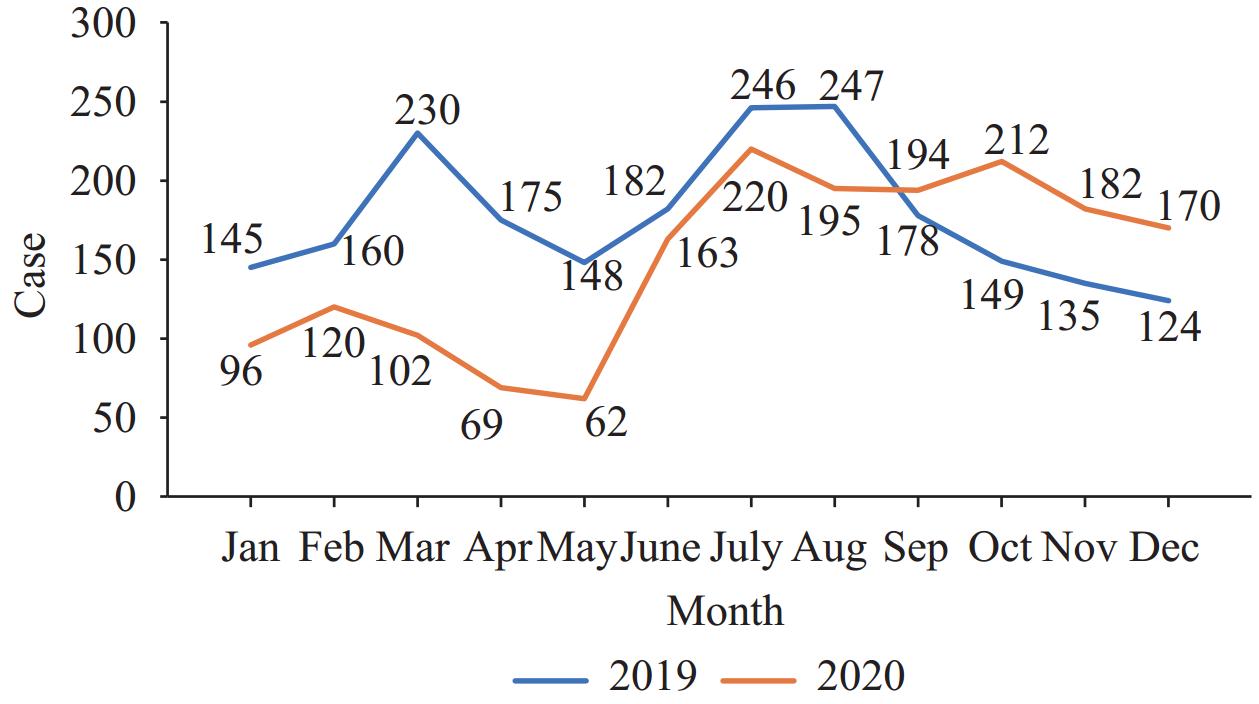
Six sentinel surveillance sites were established at the China-Myanmar border in LNA to monitor malaria. Data from 2019 was used as a baseline to analyze malaria incidence and trends in LNA and Myanmar, as well as the importation of malaria cases into China from 2019 to 2023.
Plasmodium vivax was the predominant species, representing 99.95% (14,060/14,066) of confirmed malaria cases in LNA. A total of 8,356 malaria cases were identified in 2023, with an annual parasite incidence (API) of 19.78 per 100 person-years. Compared to 2019, the incidence rate ratio was 21.47 (95% confidence interval: 18.84, 24.48), indicating that the API in 2023 was 21.47 times higher than that in 2019. In Yunnan, out of 1,016 reported cases, 545 imported cases (53.64%) originated from LNA and spread to 18 (13.95%) out of 129 counties. Ten provinces in China, including Yunnan, reported imported malaria cases from LNA in Myanmar.
The increase in population, particularly among internally displaced persons, along with inadequate healthcare services, has led to a notable resurgence of malaria in LNA. This resurgence poses a risk to preventing the re-emergence of malaria transmission in China. There is an urgent need for novel collaborative policies, as well as financial and technical assistance, to enhance malaria control efforts in LNA, Myanmar.



 Subscribe for E-mail Alerts
Subscribe for E-mail Alerts CCDC Weekly RSS Feed
CCDC Weekly RSS Feed