2022 Vol. 4, No. 38
The incidence of tuberculosis (TB) was declining in China but has plateaued in recent years.
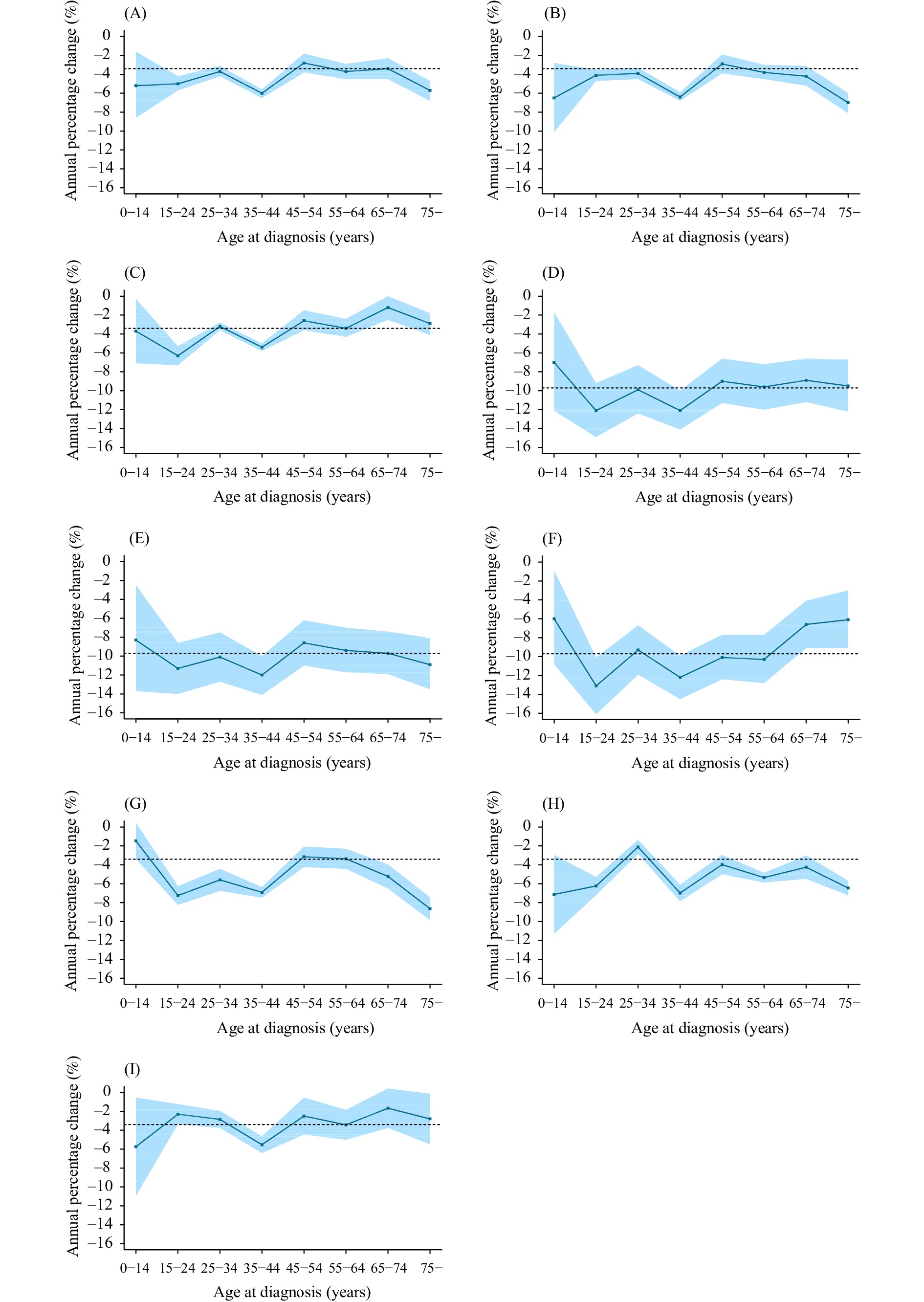
Notifications of pulmonary TB declined by 27.7% between 2008 and 2018, with an average crude decline of 3.4% per year and an average age-adjusted decline of 4.3% per year. Notifications decreased faster among older people, but slower in western China; the combination of trends led to an inflection in 2016 in the overall notification trend from decreasing to stable.
Population ageing and geographic disparities slowed tuberculosis control progress in China. Enhanced, targeted, and proactive responses are recommended to achieve the End TB targets.
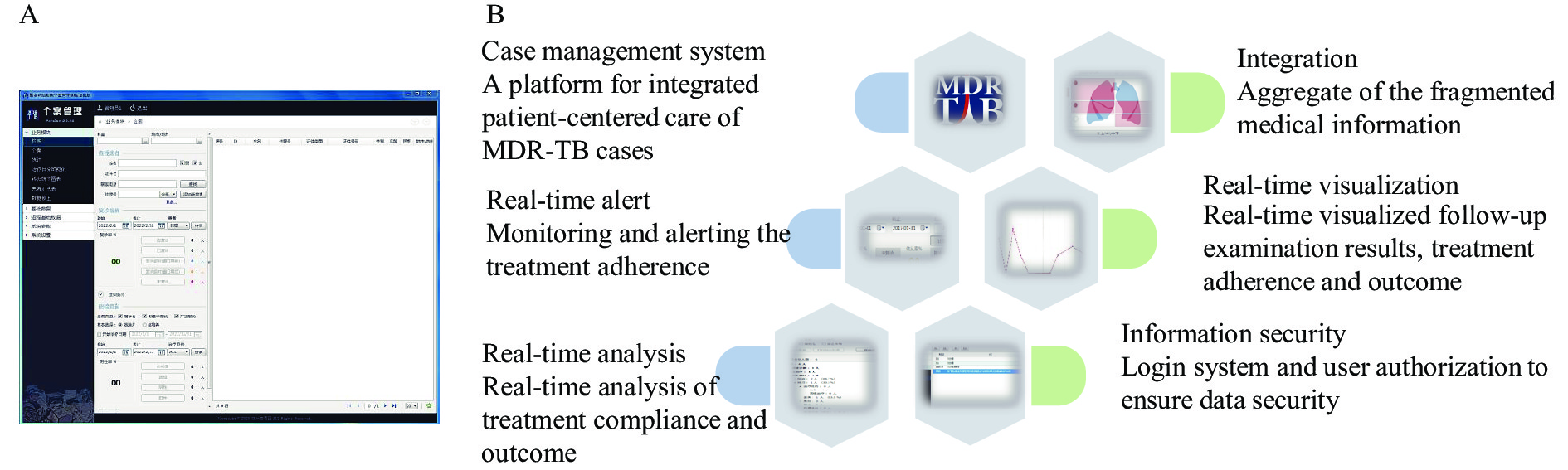
Treatment and case management of multidrug-resistant tuberculosis (MDR-TB) is a significant challenge in tuberculosis (TB) control and prevention. This pilot study aims to apply and test a new electronic information system in order to help bolster case management of MDR-TB.
The MDR-TB Case Management System (CMS) was developed and piloted in the Yunnan Tuberculosis Clinical Center (TCC) in 2017. Next, 5 sites in Yunnan were randomly selected and sampled as pilots in 2018. The real-time regular follow-up rate (RFUR) was calculated for pilot sites. Loss to follow-up (LTFU) rates of MDR-TB treatment cohorts between pilot and non-pilot sites were compared by a chi-square test. LTFU for MDR-TB treatment cohorts was then assessed by univariate and multivariate binary logistic regression.
The average regular follow-up rate was 90.7% in TCC and 73.7% in five other pilot sites of Yunnan Province respectively. The average LTFU rate for pilot sites (9.0%) was lower than non-pilot sites (20.6%, P<0.01). The risk of LTFU during MDR-TB treatment reduced 61.7% in CMS pilot cases (adjusted odds ratio: 0.38, 95% confidence interval: 0.23–0.60) compared with non-pilot cases.
As a significant supplement to the Tuberculosis Information Management System, the CMS strengthened the collection, analysis, and utilization of strategic information for MDR-TB cases. The system improved case management by embedding it as a tool of the Comprehensive Supportive Care service model.



 Subscribe for E-mail Alerts
Subscribe for E-mail Alerts CCDC Weekly RSS Feed
CCDC Weekly RSS Feed