-
In the past hundred years, human population expansion and globalization have changed the pattern of human-nature interactions and accelerated the emergence and spread of novel infectious diseases (1). Humans have experienced a long list of microbial threats to health, of which, 70% are believed to be from animal reservoirs (2), such as severe acute respiratory syndrome coronavirus (SARS-CoV), Middle East respiratory syndrome coronavirus (MERS-CoV), and avian influenza A (H7N9) viruses, etc., emerging in 2002–2003, 2012, and 2013, respectively (3). Among the microbial threats, pandemic-causing viruses have profound and far-reaching impacts on public health, the economy, and society. Pandemics in the past century were mainly caused by influenza viruses: 1918 H1N1, 1957 H2N2, 1968 H3N2, and 2009 H1N1, defined by World Health Organization (WHO), together with the re-emergence of H1N1 influenza virus in 1977 (4-5). At the end of 2019, coronavirus disease 2019 (COVID-19) with human coronavirus-19 (hCoV-19, also termed SARS-CoV-2 by International Committee on Taxonomy of Viruses) as the causative agent, emerged and became the largest and most devastating pandemic in the new century (6). Currently, the world is still in the midst of this coronavirus pandemic. As two pandemic-risk viruses both transmitting through respiratory tracts, it raises concerns on how SARS-CoV-2 and influenza viruses themselves, and the relevant public health measures and scientific researches influence each other.
SARS-CoV-2 and influenza viruses have many common characteristics which may correlate with the driving force of pandemics. The respiratory tract as the transmission route enables the disease to spread globally in a short time. The considerable number of latent or asymptomatic infections and mild cases brings difficulty to the control of the diseases (7). Emerging viral variants present alarming characteristics, including increased transmissibility and infectivity, alternative drug resistance, and immune escape. The wide range of animal hosts for the influenza viruses and the recently-discovered diverse susceptible animals of SARS-CoV-2 provides potentials for reemergence, though the animal reservoir of SARS-CoV-2 has not been confirmed (8). Thus, these common features of the two viruses imply that knowledge can be shared in the control of them.
-
Looking back on the hundred-year history of humans fighting against influenza, most experience of responding to the pandemic comes from this process. At the very beginning of the COVID-19 pandemics, plenty of experts on influenza took on the mission and applied the experience derived from prevention, control, and research on influenza to COVID-19. The Chinese National Influenza Center undertook most of the hCoV-19 (previous name of SARS-CoV-2) genome sequencing work in the National Institute for Viral Disease Control and Prevention of China CDC (9). Since its launch, the Global Initiative on Sharing All Influenza Data (GISAID) played an essential role in the sharing of data from influenza viruses. After initial deposition of the hCoV-19 whole genome sequences by China CDC, authorities and researchers looked to GISAID for its expertise in facilitating rapid sharing of trusted data (9). Currently, more than five million hCoV-19 genome sequences have been shared on GISAID since January 2020 and are helping the scientists study the new virus (10), together with other SARS-CoV-2 databases, such as RCoV19 from the China National Center for Bioinformation (11). Thus, the accumulated experiences, techniques, and human resources from influenza pandemic preparation have played an important role in the responses to COVID-19 pandemic (12). Interestingly, the in-depth and extensive researches on COVID-19 by a large number of scientists gathered in a short period of time have also promoted our understanding of influenza viruses and improved the prevention and response capacity. New vaccines and drugs, such as mRNA vaccine and monoclonal antibody drugs, are quickly being developed and used with emergency authorizations (13). Nucleic acid testing is becoming widely accepted (14), and traceability of the new virus has received unprecedented attention not only from the scientific community (15). The evidence of the introduction and spread of SARS-CoV-2 through cold chain also brings into reconsideration of the seasonal features of influenza viruses (16).
-
Since the emerging of COVID-19, influenza activity in different countries plunged in early 2020 and stayed at lower levels than expected during the 2020–2021 season (17-18). In China, influenza-like illness (ILI) activity across the country was significantly lower in 2020 compared to 2015–2019 (Figure 1). Furthermore, the influenza positive rate in 2021 has remained below the national epidemic threshold (15.5%) as of Week 43, although the overall weekly ILI rate and influenza positive rate since Week 13 of 2021 was slightly higher than the rate during the same period in 2020 (Figure 1). Public health interventions against COVID-19 decreased influenza activity directly. With similar routes of transmission, the mitigation methods used to prevent COVID-19 transmission also reduced influenza transmission (19). Hygiene habits of the public, including mask wearing, hand washing, and proper ventilation, have been broadly advocated. Other non-pharmaceutical interventions (NPIs) for COVID-19 also restricted the transmission of influenza, e.g., canceling of mass gatherings, closing public entertainment venues and schools, restricting domestic and international travel, issuing stay-at-home orders, and active and passive quarantine of cases with febrile respiratory syndrome. However, the reported SARS-CoV-2 and influenza virus co-infections indicated that SARS-CoV-2 itself does not repel the influenza virus in the host and no cross-immunity between the two viruses exits (20-21).
-
During the second half of the war against COVID-19, the influenza activities will become complicated and difficult to predict. Key challenges are posed to the prevention and control of the two viruses (22). First, some countries no longer consider COVID-19 a social critical disease and have lifted their social restrictions. The NPIs will be relaxed incrementally, which is expected to result in higher influenza infection over the following flu season. Second, the low circulation of the influenza virus in recent seasons challenges the prediction of potential prevalent influenza viruses from the currently limited genetic variants, which increases the likelihood of influenza vaccine mismatch. Third, similar to the emerging of the new variants of SARS-CoV-2 with higher transmission capacity and changed antigenicity, the new genetic variants of influenza viruses may also erupt under a selective pressure of current NPIs against COVID-19. Fourth, global population immunity to influenza will have decreased with very low levels of influenza activity in the recent seasons. Fifth, the shifting of medical personnel and resources in favour of COVID-19 in some countries and regions will continuously impact the capacity of health services to respond to a potential influenza pandemic (23). Furthermore, a potential co-circulation of other respiratory viruses, including respiratory syncytial virus, will make the situation more complicated in the future seasons (24).
-
Facing the complicated situation of co-circulation of SARS-CoV-2 and influenza viruses together with other respiratory pathogens, comprehensive prevention and control strategies are needed. First, it is important to enhance the WHO’s Global Influenza Surveillance and Response System to monitor the respiratory viruses (25). Effective continuous surveillance of any new variants is key for providing early warnings. The epidemic model based on the new circumstances remolded by the diseases will provide new insights into the regularity and give useful references for the strategies. Second, active NPIs are still an economic tool to control the spread and to decrease the impact of an influenza endemic. The relaxation of NPIs with the increasing coverage of SARS-CoV-2 vaccination in some countries should be gradually stepped up and fully assessed for risks. Third, rapid differential diagnosis of COVID-19, influenza, and other respiratory pathogens is needed, especially during the winter. It is a good choice to develop rapid dual or multiplex diagnostic tests to distinguish between these two viruses and other respiratory pathogens, particularly among front-line healthcare professionals and other populations with high risks for exposure. Early diagnosis will facilitate isolation, management, and treatment of both hospitalized patients and outpatients. Fourth, the average national vaccination coverage for influenza varies greatly across countries. Thus, at the same time as popularizing the COVID-19 vaccines and even its booster, influenza vaccination coverage should also be encouraged. The immunological barrier at the population-level established through vaccination is always a safe and economic pathway to interrupt transmission (26). The theme of World Flu Day this year (the 4th) is “Flu and COVID-19: Let’s get vaccinated” (27-28). Lastly, scientific investigations on these pandemic-risk viruses should also be enhanced. For instance, we should assess the risks of already emergent influenza viruses, such as human-infecting avian influenza A (H5N6) viruses including the transmission, infection, immunogenicity and drug resistance, etc. (29). The development of universal vaccines, drugs, and testing reagents will be prepared for future pandemics induced by the viruses from the same family or at least the same genera.
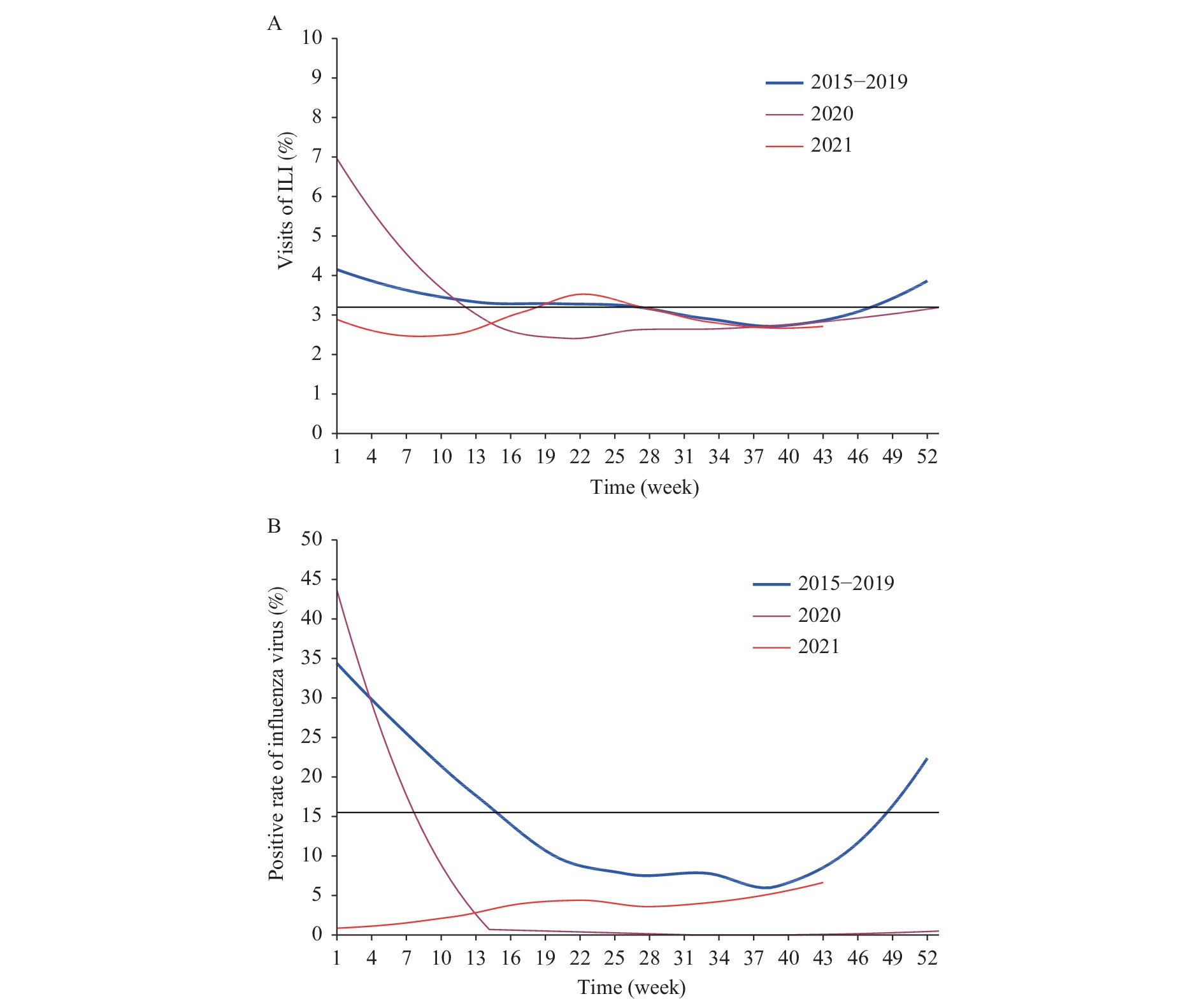 Figure 1.
Figure 1.Percentage of visits for (A) influenza like illness and (B) influenza virus positivity at sentinel hospitals in overall China, during 2020 and 2021 compared with 2015 to 2019.
Notes: Average weekly percentage of visits for ILI was 3.0% in 2020 compared with the average ILI 3.2% of 2015–2019, with a drop of 6.25% (P<0.001); the percentage was further decreased by 10% from the ILI 3.0% in 2020 to ILI 2.7% in 2021 (P<0.001). Average weekly positive influenza virus rate decreased by 61.94% (P<0.001) from 2015–2019 (15.5%) to 2020 (5.9%), and continuously decreased by 44.07% (P<0.001), from 2020 (5.9%) to 2021 (3.3%). 1) All data were collected from Chinese National Influenza Center Weekly Report (http://www.chinaivdc.cn/cnic/zyzx/lgzb/202111/t20211105_252585.htm). 2) R software (R4.0.4 version, R Development Core Team, Auckland, New Zealand) was used to analyze the data and generate the figures. 3) Two proportional tests were used to check the differences in average weekly ILI percentage and influenza virus positivity over the years from 2015 to 2021. 4) Black lines in Panel A and B denoted the national epidemic thresholds during 2015–2019, i.e. 3.26 ILI cases per 100 outpatient visits and the influenza positive rate (15.5%), respectively. 5) The blue line in Panel A indicates the calculated mean values of ILI in each week during 2015–2019. The mean values of ILI= the sum of ILI among 2015–2019/the total visits for ILI at sentinel hospitals among 2015–2019 in overall China by week; 6) The blue line in Figure B indicates the calculated mean influenza virus positivity in each week among 2015–2019. The mean influenza virus positivity = the sum of influenza virus positive samples among 2015–2019/the total samples collected for ILI at sentinel hospitals among 2015–2019 in China overall by week. Abbreviation: ILI=influenza-like illness.The emergence and re-emergence of diverse subtypes of influenza A viruses, which are known as “HxNy” mediated through the reassortment of viral genomes, together with influenza B viruses will continuously account for future pandemics. Beyond SARS-CoV and current SARS-CoV-2, we are not sure whether there will be a “SARS-CoV-z” in the future. However, with experiences from the responses to influenza and SARS-CoV-2, a series of prevention and mitigation measures, including new diagnosis and surveillance technologies, pharmaceutical measures and NPIs are developed to help preserve and boost the capacity and function of health systems across the world. We can do these better for the next virus!
-
No conflicts of interest.
HTML
| Citation: |




 Download:
Download:




