-
Chronic obstructive pulmonary disease (COPD) is a public health challenge in China because of its high prevalence, related disability and mortality, and heavy economic burden (1-3). COPD morbidity and mortality is associated with adverse weather and air pollution (4-7). However, it is difficult for both COPD patients and medical staff to be alerted in advance of high-risk periods with existing tools. The Shanghai Meteorological Service (SMS) has developed a health forecasting service for COPD patients based on the weather and air quality forecasts. A prospective controlled trial was conducted in Pudong New Area of Shanghai from October 2019 to April 2020 to examine whether such a forecasting service being available to COPD patients and their general practitioners (GPs) could reduce visits and costs in outpatient and emergency departments (OPED) for COPD. In this study, 1,349 patients in each group were analyzed after balancing the control and intervention groups by using the propensity score matching (PSM) method. Compared with the control group, there was a 17.6% reduction in the proportion of OPED patients and a 13.9% reduction in the OPED visits in the service group. The results of this study suggest that COPD risk forecasting service could be a novel method of COPD management in public health to improve health and economic outcomes.
This study was designed as a prospective intervention study with two groups: the service group (patients receiving COPD risk forecasting service; also known as the intervention group) and the control group (patients not receiving the COPD risk forecasting service). According to previous studies, every 1 °C increase of daily mean temperature was associated with a 7.0% decrease (95% CI: 4.9, 9.0) in the risk of COPD hospitalization in Beijing (8) and a 3.0% decrease (95% CI: 2.0, 4.0) in COPD symptoms in Shanghai (4). The proportion of COPD patients receiving outpatient treatment, the primary dichotomous endpoint, was usually around 50% (3). Assuming that rate ratio of OPED visit for the service group was 0.85 compared with the control group, a total of 1,854 subjects (927 for each group) were required to detect a difference between the two groups at a 90% power with a two-sided significance level of 0.05.
COPD patients in Pudong New Area of Shanghai Municipality were selected as the local CDC had an established routine COPD management system with thousands of clinically diagnosed COPD patients registered to community health service centers. Patients consenting to participate were required to provide following information at baseline: age, sex, number of acute exacerbations of COPD (AECOPD) within the last year. Furthermore, patients selected to receive the COPD risk forecasting service were also asked to provide contact details.
Overall, there were three methods the COPD risk forecast service was provided: 1) a specially designed platform for WeChat displaying daily updated forecast information and chat groups including patients, GPs, CDC staff, and SMS staff; 2) mobile phone text messages; and 3) automated phone calls. Except for the WeChat platform, COPD risk forecast was provided regularly 2 to 3 times per week and before adverse weather events. Patients were sent an information pack that described how future weather could affect COPD and detailed advice on self-management of COPD, such as keeping warm, reducing exposure to cold temperature or air pollution, appropriate exercise, and so on. They were also advised to contact their GP if necessarily. At the end of study, adherence of patients in the service group was self-reported in questionnaire according to whether they adjusted their behavior when they were alerted in high-risk period. Their satisfaction with the forecasting service was also evaluated with answers of satisfied, moderate, or dissatisfied.
In both the service and control groups, patients had died from other diseases during the study period (October 2019–April 2020) and those less than 40 years old were also excluded. As the baseline characteristics of the service and control group were unbalanced (Table 1), the PSM method was used to balance variables and reducing the bias between the control and service groups. The method has been used with increasing frequency in observational studies and clinical trials (9), which attempts to adjust post hoc for recognized unbalanced factors at baseline to approximate a randomized data to analyze. Logistic regression was used to calculate the propensity score of each patient. Then the 1∶1 case-control matching was conducted according to the principle of neighboring matching with caliper value of 0.01. The matching variables were the patients’ age, gender, and the AECOPD counts within the last year. The service group was also divided into the WeChat group, the text group, the call group, and the mixed group (the group of patients receiving COPD risk forecast in two or more methods). After matching, monthly COPD-related OPED visits and costs of each group during the study period were collected from the information center of Pudong New Area Health Commission. All the COPD-related OPED visits were defined according to clinical diagnosis (J40, J42–J44). OPED costs for COPD were also divided into costs for registration, medication, examination, etc.
Characteristics Before PSM After PSM Patients not receiving service (n=1,631) Patients receiving service (n=2,204) P value Patients not receiving service (n=1,349) Patients receiving service (n=1,349) P value Age, years 71.7±10.3 67.9±9.3 <0.001 69.3±9.1 69.5±9.0 0.522 Male,N (%) 932 (57.1) 1303 (59.1) 0.232 761 (56.4) 774 (57.4) 0.641 AECOPD counts within the last year, N (%) <0.001 0.010 0 1,307 (80.1) 1,431 (64.9) 1,060 (78.6) 1,002 (74.3) 1 172 (10.6) 451 (20.5) 143 (10.6) 224 (16.6) ≥2 152 (9.3) 322 (14.6) 146 (10.8) 123 (9.1) Abbreviations: PSM=propensity score matching; COPD=chronic obstructive pulmonary disease; AECOPD=acute exacerbation of COPD. Table 1. Characteristics of COPD patients in groups of receiving or not receiving the COPD risk forecast service before and after propensity score matching in Pudong New Area, Shanghai Municipality from October 2019 to April 2020.
A generalized estimation equation (GEE) was used to examine the effects of COPD risk forecasting service on OPED visits and costs for COPD. Monthly visits and costs were used as dependent variables. As the number of OPED visits was approximately Poisson distributed, the Poisson distribution was used in the analysis. OPED visits were also treated into dichotomous variable (yes or no). Patients’ age, gender, and AECOPD counts within the last year were adjusted as covariates in the GEE model. All statistical analyses were conducted with R version 4.0.2 (R Development Core Team, Auckland, Nz). The geepack package was used to conduct GEE. The significance level was set at 0.05 (two-tailed).
A total of 4,880 COPD patients participated in this study. After some patients were excluded, 2,204 patients were included in the service group, and 1,631 patients were in the control group (Table 1). Before using PSM, baseline conditions of the two groups were unbalanced. In the service group, the age and proportion of patients having AECOPD in the last year were both smaller than those of the control group. After PSM, 1,349 patients in the service group were successfully matched with 1,349 controls. Patients in the control and service group were balanced in age and gender. Compared with the control group, the proportion of patients having AECOPD in the last year increased by 4.3% in the service group, whereas the proportion of patients having more than one time of AECOPD decreased by 1.7%, as shown in Table 1. After a 6-month forecasting service, 85.8% of patients in the service group reported good compliance with advice in the forecasting service. There were 88.7%, 79.6%, and 90.0% of patients satisfied with the service provided by WeChat, text, and call, respectively.
There were 545 COPD patients in the service group that visited OPED at least once for COPD for a total of 1,986 person-times during the study period, while 502 patients in the control group visited for a total of 2,031 person-times. Figure 1 showed the proportion of COPD patients visiting COPD-related OPED in the service and control groups in Pudong New Area, Shanghai, from October 2019 to April 2020. In the service group, 18.1% of patients visited OPED in December 2019, and 12.3% visited OPED in April 2020. Showing a similar time trend in the control group, there were 19.1% and 13.3% of patients visiting OPED in December 2019 and April 2020, respectively. The proportion of patients visiting COPD-related OPED in the service group was consistently lower than that in the control group from December 2019. The monthly person-times of OPED visits also peaked in December 2019 and gradually declined in the following months. In the service group, patients visited OPED for 244 times in December 2019 and 166 times in April 2020. In the control group, the figures were 258 times and 180 times, respectively.
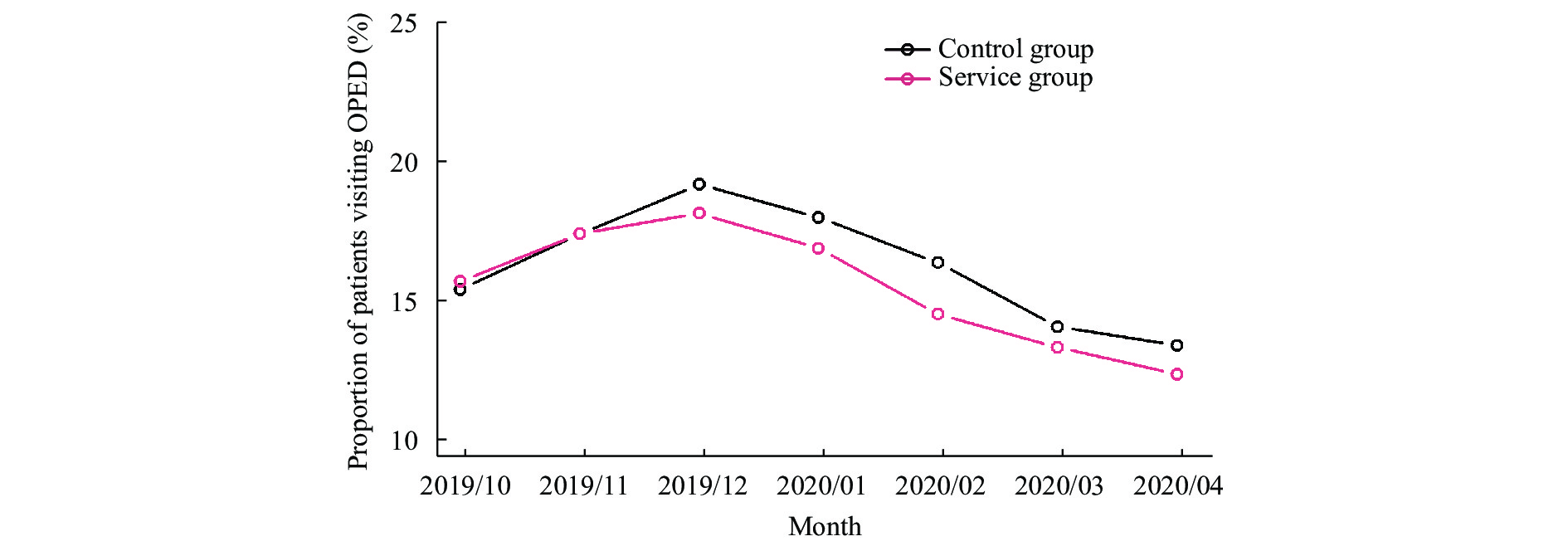 Figure 1.
Figure 1.The monthly proportion of COPD patients visiting outpatient and emergency departments for COPD in the service group (1,349 patients) and the control group (1,349 patients) in Pudong New Area, Shanghai Municipality from October 2019 to April 2020.
Abbreviation: OPED=outpatient and emergency departments.The results of the GEE models in evaluating the effects of COPD risk forecasting service on the proportion of COPD patients visiting OPED and person-times of OPED visits in Pudong New Area of Shanghai from October 2019 to April 2020 were shown in Table 2. When the proportion of patients was analyzed, the relative risk (RR) for patients receiving service relative to those not receiving it was 0.824 (95% CI: 0.686, 0.990), i.e., a 17.6% reduction with a wide 95% CI of 1.0% reduction to 31.4% reduction. When the person-times of OPED visits were used, the corresponding RR was 0.861 (95% CI: 0.744, 0.995), which meant that receiving such service had effect of reducing OPED visits by 13.9%. The RRs for patients receiving service via WeChat, text, or call were mainly less than 1 with wide CIs across 1, suggested less OPED visits although the effects were not significant for patients receiving the service only through a single method. When two or more service methods were used, there was a significant effect of reduction in person-times of OPED visits with a RR of 0.755 (95% CI: 0.597, 0.955).
Groups N Patients visiting OPED Person-times of OPED visits OPED costs, RMB Medicine costs, RMB Persons (%) RR (95% CI) Times RR (95% CI) Mean β (95% CI) Mean β (95% CI) Control 1,349 502
(37.2)Ref 2,031 Ref 511.7 Ref 422.6 Ref Service 1,349 545
(40.4)0.824
(0.686, 0.990) *1,986 0.861
(0.744, 0.995) *478.4 −11.194
(−24.579, 2.191)399.1 −9.522
(−21.285, 2.241)WeChat 204 73
(35.8)0.945
(0.659, 1.354)273 1.012
(0.768, 1.335)455.8 −0.797
(−28.194, 26.600)394.1 1.727
(−22.287, 25.741)Text 619 258
(41.7)0.855
(0.683, 1.071)919 0.913
(0.764, 1.093)505.6 −5.389
(−23.368, 12.590)420.9 −5.120
(−20.985, 10.744)Call 169 75
(44.4)0.747
(0.502, 1.112)294 0.759
(0.532, 1.084)464.3 −25.900
(−50.865, -0.935)*370.0 −24.895
(−44.945, −4.845)*Mixed 357 139
(38.9)0.756
(0.558, 1.025)500 0.755
(0.597, 0.955) *450.9 −20.258
(−39.644, -0.872)*378.1 −16.172
(−33.425, 1.081)Abbreviations: OPED=outpatient and emergency departments; Ref=reference group;RR= Relative risk.
* P<0.05.Table 2. Effects of the COPD risk forecasting service on the visits and costs of outpatient and emergency departments for COPD in Pudong New Area, Shanghai Municipality from October 2019 to April 2020.
The total OPED costs of these 2,698 patients were 1.34 million RMB during the study period, in which medicine accounted for 82.9%. The total OPED costs and medicine costs per patient due to COPD were 495.1 RMB and 410.9 RMB, respectively, during the study period. Table 2 also showed the effect of COPD risk forecasting service on the OPED costs for COPD using GEE. In general, patients receiving the COPD risk forecast service seemed to have lower total spending on OPED services and medication than those not receiving the service, although these results were not significant. The cost-reducing effects varied by way of providing the forecasting service, with significantly stronger effects in the call group and mixed group. For example, patients receiving the service via calls and in two or more methods had a decline of 25.90 RMB (95% CI: 0.87, 50.94) and 20.26 RMB (95% CI: 0.87, 39.64), respectively, per patient in OPED costs relative to those not receiving service.
HTML
-
This study evaluated the impact of environment-based health forecasting service, a new method of COPD management for the first time in China. Patients receiving the forecasting service had less visits and costs in outpatient and emergency departments due to COPD than those not receiving it between October 2019 and April 2020. It seemed that better effects could be reached by providing services via automated calls or in multiple methods than via WeChat or text messages.
In this study, compared with the control group, there was a 17.6% reduction in the proportion of OPED patients and a 13.9% reduction in the OPED visits in the service group. The effects were similar with those reported in UK (10-11), where a COPD forecasting service appeared to reduce the frequency of COPD exacerbation by 18.8% and the severity of exacerbation, but the effects did not reach statistical significance perhaps due to their smaller number of participants (only 79 patients) and lower exacerbation rates. Our study had 2,698 COPD patients participating in and using OPED visits instead of AECOPD hospitalization to enlarge outcome rates.
We used several methods to provide COPD risk forecasting service to patients. However, patients receiving the service via phone calls appeared to have less OPED visits and costs than those receiving the service via WeChat and text. It may be due to different accessibility of these methods. In this study, more than 80% of patients in the call group answered frequently whereas only around 60% of patients registered in the specific WeChat platform. As the most popular social network in China, WeChat has been widely used in chronic disease management (12). However, WeChat may be not easy for older patients to use because their education levels, income levels, and physical conditions tend to make app use more challenging. Mobile phone text message is a traditional method to send weather forecast and disease-related information to patients. The use of text messages can be also affected by its higher barrier to engagement (due to being purely text) and the patients’ education level, although there was great uncertainty of the proportion of COPD patients in the text group successfully receiving the forecasting service.
The monthly COPD-related OPED patients and visits were both found to peak in December 2019 and declined in the following months. This is possibly caused by there being more COPD morbidity in the cold season than in the warm season. Also, the coronavirus disease 2019 (COVID-19) pandemic occurred in the last 3 months of this study, which might have reduced the OPED visits for COPD to some extent. In a cross-sectional survey in Beijing (13), compared with that before the COVID-19 epidemic, fewer COPD patients maintained their pharmacological treatment. It was reported that only 15.6% of COPD patients who experienced respiratory symptoms aggravation sought medical care in hospital as 55.5% were concerned about cross-infection of COVID-19 in the hospital and the remaining 28.8% took more medication by themselves.
This study was subject to some limitations. Patients were not randomly allocated in the control and service groups. However, the PSM method had been adopted to control for selection bias to achieve the goal of balancing. In addition, some potential risk factors (the severity of COPD, respiratory infection, socioeconomic status, and smoking) associated with outpatient visit for COPD might have been missed in the baseline investigation. Moreover, the unexpected emergence of COVID-19 in the late period of the study period changed both patients’ and hospitals’ practice and resulted in trends such as less hospital visits and better self-management, which thus reduced some OPED visits in both groups during the late period and may limit the effects of the forecasting service.
Despite these limitations, the evaluation shows an association between the delivery of COPD risk forecasting service and the reduction of visits and costs of COPD patients in outpatient and emergency departments. The effectiveness of the service depends on the methods of patients receiving it. More longitudinal research with random allocation of patients and more influencing factors considered on the effectiveness of forecasting service is warranted.
Acknowledgement: All staff in community health service centers who provided assistance for patient’s recruitment and medical consultation.
| Citation: |



 Download:
Download:




